Medtech and Artificial Intelligence
SPIN Programme
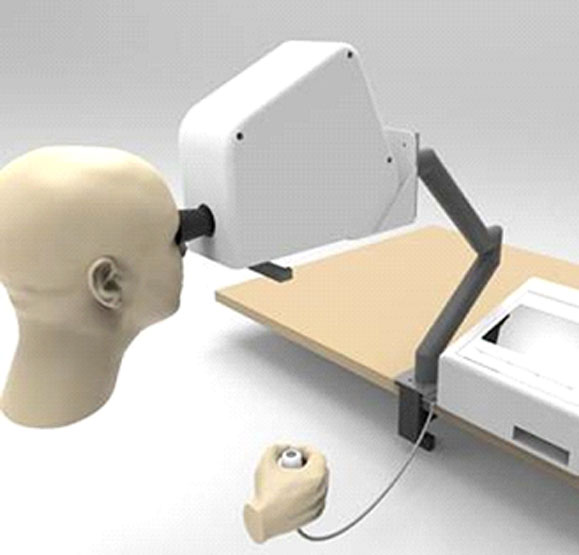
Globally, there is a need to develop new healthcare delivery models/technologies to cater for the needs of rapidly ageing patient populations. Glaucoma is an example whereby approximately 70% of patients are above 60 years old and, due to increasing average-life- span, are facing a longer time of reduced quality of life due to vision loss. Additionally, glaucoma is often detected only when one’s vision is already irreversibly impaired. This is unfortunate as early detection can allow clinical intervention that will ultimately maintain the elderly’s independence and quality of life. Currently, diagnosis and monitoring of glaucoma uses perimetry (or visual field testing) as one of the primary measures. However, current perimetry methods have major drawbacks. As part of the SPIN Program, we aim to develop a novel, Smart, User-friendly, Portable and Reliable Automated (SUPRA) perimetry device that can measure visual field that will assist early detection of glaucoma. Such a device will potentially allow perimetry services to be provided by general-practitioners, polyclinics or eldercare facilities.
The SUPRA is just one of a few medical devices being co-developed which will eventually form part of a robust multi-modal platform to make eyecare more accessible to the community.
This includes:
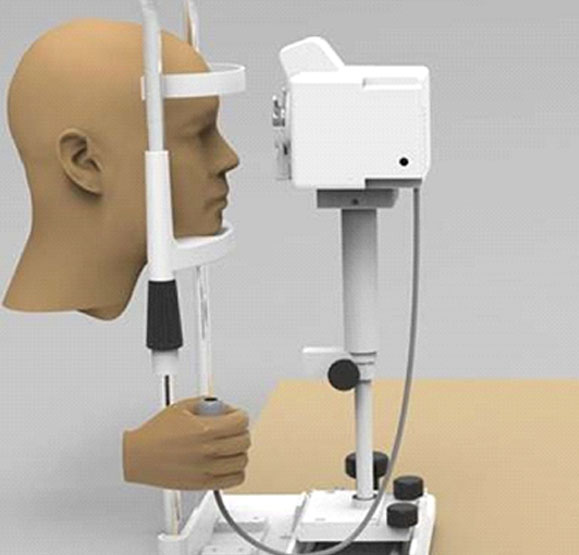
- A low-cost portable non-mydriatic fundus camera
- Portable anterior segment and slit lamp camera
- Portable photo-gonioscopy camera
- Non-contact tonometry device to measure intra-ocular pressure
- Self-administered, automated visual acuity testing
- Gait and visual field analysis in the prevention of falls
Artificial Intelligence and Ophthalmology
The potential of using artificial intelligence in Ophthalmology is huge due to the large patient pool and imaging modalities available. Most of the diagnostic tools used in ophthalmology result in images or statistics which need to be interpreted by clinicians. These results can be processed for features and fed into machine-learning algorithms like support vector machines and neural networks. Artificial intelligence can be integrated into diagnostic equipment, increasing the speed and quality of diagnosis. For example, diagnosis of basic tests can be automated, saving time for patients and allowing doctors to focus on more complex cases. We are currently testing the use of artificial intelligence on detecting diabetic retinopathy and macular degeneration, and predicting glaucoma progression.
Anterior Segment OCT Analysis of Angle-Closure Glaucoma Mechanisms
Angle closure glaucoma is a challenging diagnosis and treatment needs to be individualized. Our group has published extensively on the different mechanisms of angle closure and their optimal treatment. However, we recognize that it is difficult to make an accurate diagnosis of angle closure mechanisms on anterior segment optical coherence tomography scans without the necessary experience and expertise. As such, we designed and patented a novel algorithm which has been validated through clinical trials in NUH. We are in the process of developing a practical system which could be integrated into clinical practice of tertiary glaucoma units to improve the accuracy of identifying the different mechanisms of angle closure.
EyeDEA – Eye Drop Electronic Alarm (Glaucoma Medication Management System)
Glaucoma is the leading cause of irreversible blindness worldwide and one of the commonest chronic age-related eye diseases. Glaucoma will affect more than 100 million individuals by 2040 – with 1 in 8 going blind. There is no cure for glaucoma, and life-long eye drops are often required to lower the intraocular pressure (IOP) and keep the disease under control. In the United States alone, sales for glaucoma eye drops is estimated to reach US$2.2billion by year 2023 (C.A.G.R of 2.5%). Studies have shown that between 50% and 80% of glaucoma patients were non-adherent to their eye drops. Common factors for poor compliance include: complex eye drop regimes, poor physician-patient communication, knowledge gaps, forgetfulness, eye drop bottle exhaustion before follow-up visits, economic factors, and lack of feedback/signs from using the eye drops. Similar high rates of non-adherence have also been found in other major studies worldwide which are mostly using patient feedback surveys, and suggests a huge need for a solution to measure and improve medication adherence among glaucoma patients. To our knowledge, currently, there is no technology which directly determines and track adherence to eyedrops. Our primary aim is to develop and conduct proof-of-concept study for a novel glaucoma eyedrop adherence system, EyeDEA, comprising an App, Box and Card to address a multi-factorial issue.
We hypothesize that EyeDEA is a practical solution that improves patients’ adherence to their eye drops regimes by:
- Improving patients’ understanding of their medication regimes
- Bridging doctor-patient-caregiver communication gaps,
- Making the storage and use of eye drops an ease using a box with a built-in reminder system,
- Identifying and analyzing data regarding gaps in patient compliance to eye drops use,
- Rewarding patients for being compliant to their eye drops through incentives, and
- Simplifying the process of replenishing eye drops when they run low.

Mobile Imaging Device for Anterior Segment (MIDAS)
Ophthalmic complaints make up 2 – 5% of clinical consultations to the primary care physician. This proportion is likely to increase as the population ages and chronic conditions such as cataract, glaucoma, diabetic retinopathy and age-related macular degeneration become more prevalent. However, means of ophthalmic care is very limited in the primary care setting, and physicians commonly bemoan not only for a lack of expertise, but also a lack of avenue for direct communication with tertiary ophthalmology services. As a result, triaging of eye conditions is poorly conducted – the tertiary ophthalmology service is overburdened with non-urgent cases, while true ocular emergencies are still occasionally missed.
Our project aims to solve this mismatch between primary and tertiary care by providing a platform of direct communication between the primary care physician and a tertiary ophthalmic care centre. By providing both hardware and software support, connected through a cloud-based subscription service, we aim to provide a one-stop channel for direct communication between the primary care physician (general practitioner, polyclinic doctor, emergency physician) and ophthalmologists in a tertiary hospital. Through this, we believe we could bring tertiary level ophthalmology care directly into the community.
Team Members
Major Grants
| Grant Title & Title of Supported Projects | Funding Agency |
|---|---|
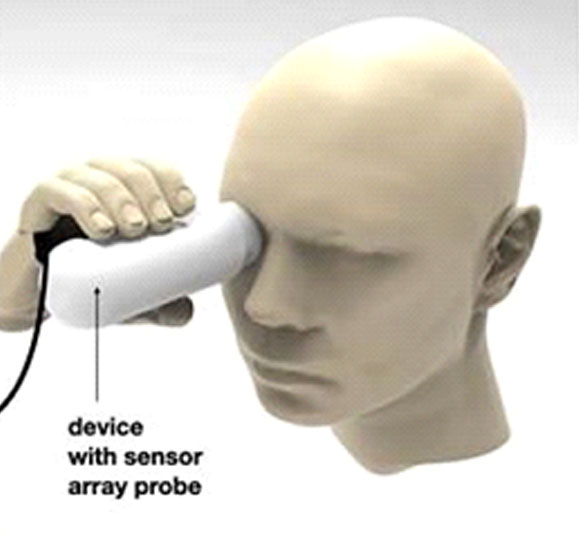
| NUHS Innovation Grant 2019 – Self-Tonometry device for monitoring of intra-Ocular Pressure (STOP) for glaucoma | NUHS |
| Engineering in Medicine - Eye Sense: Flexible Intraocular Pressure Sensor | MOE |
| Temasek Foundation Ecosperity - Community Chronic Eye Disease Screening Model Using Novel Medical Devices in Singapore | Temasek Foundation |
| Clinician Innovator Award - Developing community-friendly diagnostics for glaucoma monitoring | NMRC |
| AI-driven diagnosis with portable smartphone slit-lamp images of Asian patients | NUHS Seed Fund |
| Digital Health in Community Ophthalmology | Summit Programme in Innovation (SPIN) |
| MedMax Medical Devices Pitch for Funds - VICTAZ Portagon | MedMAx |
| NUH-NHIC Medtech Grant for SUPRA Perimetry | NUHS Internal Funding |
| Bayer-NUS Grants4Apps Challenge – EyeDEA Two-in-One Card and Wearable to improve compliance to glaucoma eye drops | Bayer Global Health |
| NUS MDG 5236 Innovation Graduate Program Seed Grant - Diabetic Retinopathy Companion Diagnostic Kit | NUS |
| National Health Innovation Centre I2P Grant - EyeDEA - a three-in-one Solution to improve eyedrop adherence | NHIC |
| National Health Innovation Centre I2P Grant - Trans-Scleral Schlemm Trabeculoplasty for Glaucoma | NHIC |
| National University of Singapore Summit in Innovation Programme - Ophthalmology | NUHS SPIN Program |
| NUH-NHIC Medtech Grant for EyeDEA – a three-in-one solution to improve eyedrop adherence | NUH-NHIC |
| National Health Innovation Centre I2D Grant – SUPRA Perimetry | NHIC |
Contact
For medical students who are interested in the medical technology research and are able to commit minimum 2 months with Ophthalmology department, please contact our research manager @ ophil@nus.edu.sg