Recovering heart attack patients in Singapore can be well cared for by highly trained and experienced nurses using digital health tools, and their quality of care “equals or even exceeds those provided by cardiologists”.

These were the findings of a trial involving 301 patients with acute myocardial infarction undergoing early revascularisation across three healthcare institutions in Singapore from July 2015 to March 2019.
NUS Nursing alumna Dr Karen Koh (PhD Nursing’17) is the co-principal investigator of the trial, dubbed “IMproving reModeling in Acute myoCardial infarction Using Live and Asynchronous Telemedicine” (IMMACULATE).
“While about 10,000 new heart attacks occur each year in Singapore, challenges remain with regard to the care of heart attack patients after they leave the hospital. Ideally, they should be reviewed just after discharge as this is when they are most vulnerable to complications,” she said.
“However, most patients wait for at least two months before getting an appointment to see their cardiologist. In the interim, some patients may be readmitted to the hospital.”
Led by cardiologist Associate Professor Mark Chan, the trial grouped patients from National University Heart Centre, Singapore (NUHCS), Tan Tock Seng Hospital and the National Heart Centre under either nurse-led remote intensive management (RIM) or cardiologist-led standard care (SC). While SC participants were treated face-to-face by their cardiologists, RIM participants underwent six months of remote consultations that included 1-blocker and angiotensin-converting enzyme inhibitor/angiotensin receptor blocker (ACE-I/ARB) dose adjustment by a centralised Advanced Practice Nurse (APN) team.
REINFORCING SELF-CARE BEHAVIOURS
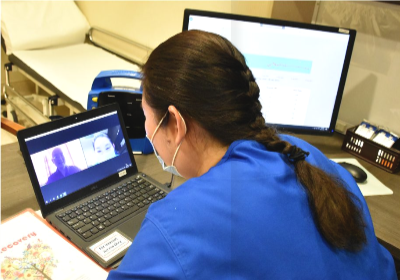
Dr Koh, a cardiac Advanced Practice Nurse with the NUHCS, and a team of three highly experienced cardiac APNs led the RIM care by making scheduled telehealth calls to the patients once a week, starting from the day after their discharge. The nurses also monitored the patients’ blood pressure and heart rate readings daily. These were keyed into devices by the patients and transmitted directly to the NUHCS’ Electronic Medical Records system.
“It’s well documented that heart attack patients rarely retain all the post-op instructions they receive from healthcare professionals upon discharge, especially after they’d suffered a life-threatening event. Through the calls, our nurses were able to reinforce self-care behaviours in bite-sized formats and work with each patient to tackle issues pertinent to his or her medical history, symptoms, medications or other lifestyle factors such as smoking or exercise,” said Dr Koh.
The protocol was to have the nurses call the patients once a week for eight weeks and subsequently once every fortnight. But if they were symptomatic, the nurses would call the patients more often. “The majority of patients who were engaged weekly by the an Advanced Practice Nurse felt that having experienced nurses to call upon as their first point of contact gave them assurance they were on the right track in their cardiac rehabilitation and were making progress,” added Dr Koh.
Another benefit was the sharing of the nurses’ notes on patients’ symptoms, concerns and risk factor management with the doctors so that these crucial issues would not be missed out during the post-procedure consultation. Similarly, patients did not need to repeat the symptoms in their discussion with the cardiologists, leaving more time for the doctors to manage their issues during the consultation.
Although the results showed that Advanced Practice Nurses, equipped and supported by an array of digital health monitoring tools, could remotely monitor and assess patients’ health daily and hold weekly consultations with them — providing a level of care not usually available from busy cardiologists running heavy clinics — Dr Koh recalled that the trial had limitations at the start when telehealth technologies had not become ubiquitous.
“As phone calls were the main mode of engagement, we were unable to pick up visual cues such as facial expressions and body language, or medical signs such as skin discolouration, shortness of breath and swelling of joints immediately. But these have now been overcome with video calls over Zoom,” she explained, adding that for some patients who require more therapeutic conversations or the human touch, video calls may still fall short.
While APNs were highly valuable in the trial as they were trained in medication titration, symptom management and triaging cases that required escalation to a cardiologist, Dr Koh said that registered nurses can be prepared for the role eventually. “We plan to partner with our community nursing team to train more nurses in symptoms management so that they attain a level of care provision to manage similar patients discharged from mainstream hospitals.”
The findings were published in the international medical journal JAMA.
Dr Koh, A/Prof Chan and the same team of investigators spanning Singapore’s three healthcare clusters are now embarking on a larger trial of 6,000 heart attack patients, in which more advanced digital tools are paired with wireless devices and wearables to enhance patients’ well-being.