Issue 46
May 2023
SCIENCE OF LIFE
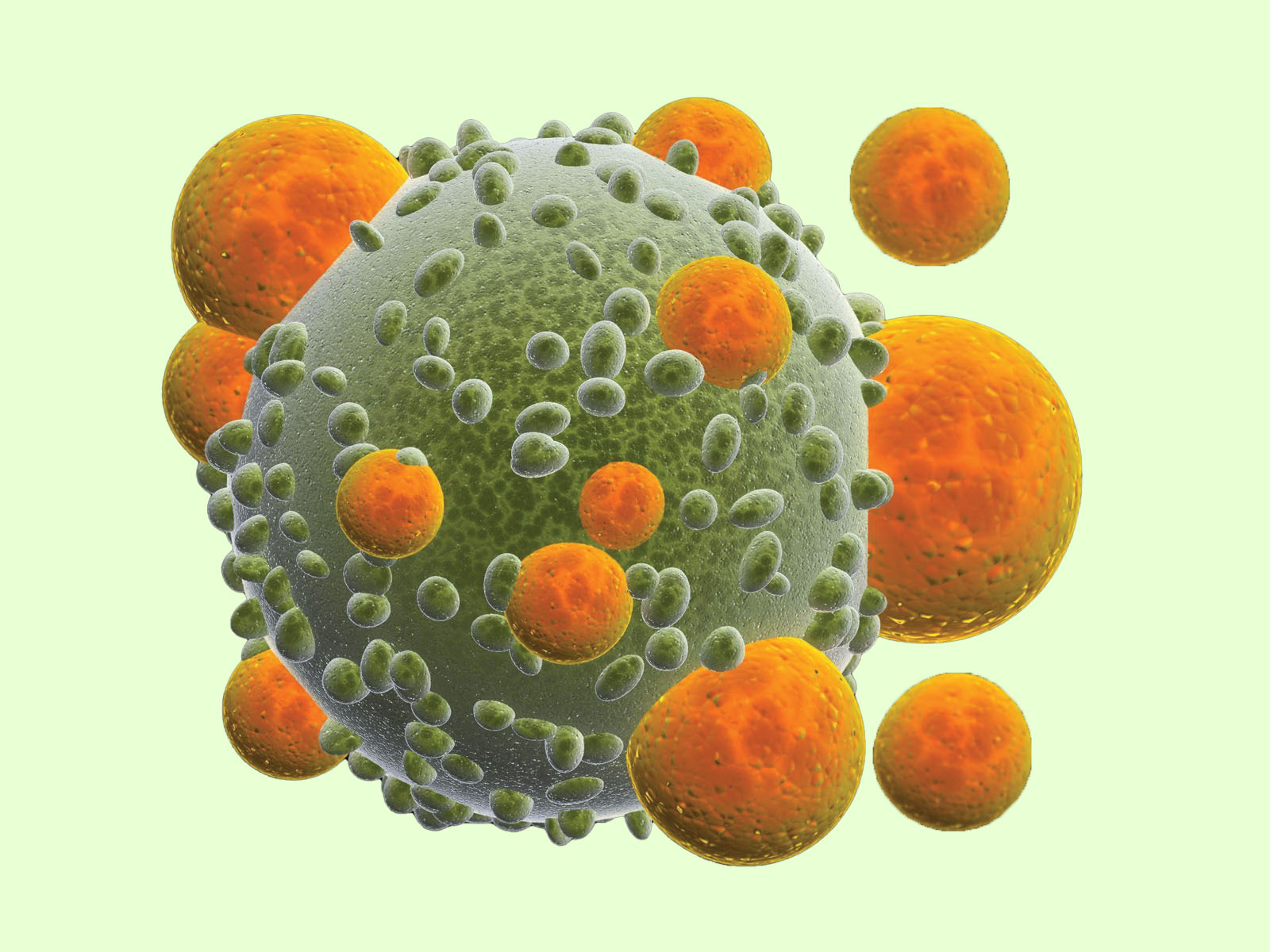
In the context of Chimeric Antigen Receptor-expressing T (CAR-T) cell therapy for cancer, researchers found that the FYN protein, rather than the lymphocyte-specific protein tyrosine kinase (LCK), allows more efficient tumour cell killing through T-cell activation.
CAR-T cell therapy involves re-engineering specific immune cells called T cells to target cancer. The treatment involves the production of CAR-T cells from the patient’s own cells, where they are then manipulated to express the CAR gene, grown to very high numbers and then re-infused into the patient. CAR-T cell therapy has not been very effective in treating solid tumours, and is often very costly.
Tackling both issues of efficacy and cost of CAR-T cell therapy, Professor Nicholas Gascoigne, Principal Investigator from the Immunology Translational Research Programme and Professor at the Department of Microbiology and Immunology at the Yong Loo Lin School of Medicine, National University of Singapore (NUS Medicine), with Dr Ling Wu and team, discovered that in CAR-T cells with CD28, the LCK is dispensable in cell signalling—the process where the cell switches on or off certain cell processes and functions, vital in activating the cell to kill tumour cells. When the LCK is disrupted, another protein, FYN, takes over cell signalling instead.
In the cell signalling pathway, the FYN protein is one of the later switches. However, since the LCK protein is the more dominant switch in T-cell activation, in normal CAR-T cells, LCK signalling is usually the main pathway activated. FYN signalling will take over when LCK signalling is disrupted.
In their study using laboratory tumour models, the CAR-T cells with disrupted LCK showed increased anti-tumour efficacy, as the CAR-T cells were able to persist longer in the body and continue killing tumour cells.
These modified CAR-T cells prevent cells transplanted from the donor from attacking the patient’s own cells, allowing for “off-the-shelf” CAR-T cell therapy. This will significantly reduce production costs for CAR-T cells and can make CAR-T cells therapy much more available and accessible to patients.
Prof Nicholas Gascoigne said, “The CAR-T field has advanced drastically over the past thirty years and presents an exciting promise of hope in cancer treatment. With this discovery, CD28 CAR-T therapy may now be used to target solid tumours such as breast and ovarian cancers, as well as reduce the cost of CAR-T therapy. This would greatly improve its accessibility to all patients.”
Click here to read more about the journal article.
More from this issue

SCIENCE OF LIFE
Mitral Valve Surgery – A Better Way
ETHICALLY SPEAKING
Who Should We Hold Responsible When AI Goes Wrong?

AFFAIRS OF THE HEART
Healthcare Systems 3.0: Perspectives of a Cardiologist and a Patient