Stronger chemotherapy for children with high-risk leukaemia boosts cure, reduces relapse rates
Published: 07 Sep 2018
A team of doctors from Singapore and Malaysia has managed to raise cure rates for a group of child leukemia patients from 69.6 per cent to 91.6 per cent while also lowering relapses from 30 per cent to 13 per cent.
The 346 children in both countries have a type of high-risk acute lymphoblastic leukaemia (ALL) that is linked to special features in their genes. Their leukaemia cells were found to be without the Ikaros gene (a development referred to as Ikaros deletion). They responded better to intensified chemotherapy treatment – 91 per cent were cured of their illness. Another group of high risk patients whose leukaemia carried the Philadelphia chromosome also received intensified chemotherapy treatment as well as a drug called imatinib.
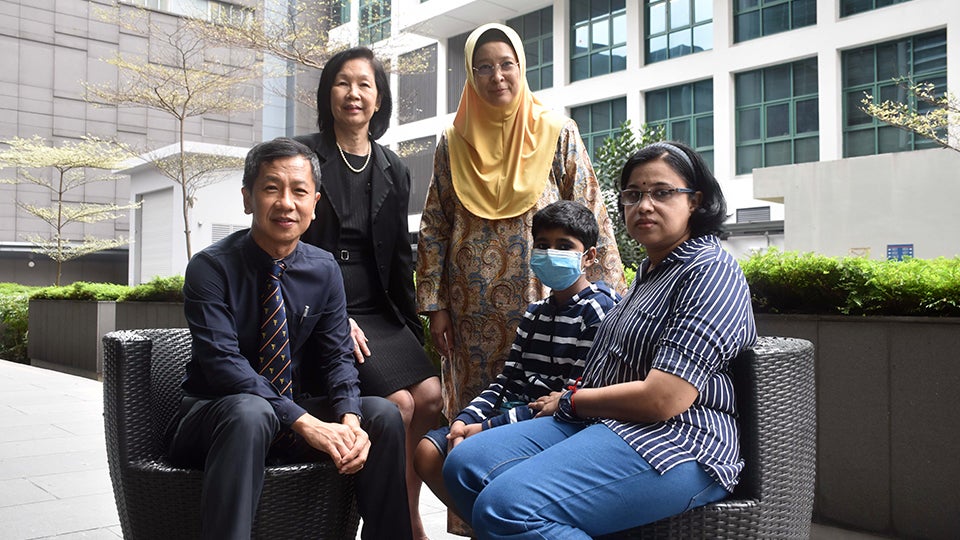
“The Holy Grail in cancer treatment is to pick up children who are more likely to relapse on standard therapy and give them better treatment. The Ikaros gene allows normal cells to mature into functional cells. About 20 per cent of children with ALL lose the Ikaros gene in their leukaemia cells, which do not mature. The leukaemia cells are stuck in an immature and constantly growing state. These children therefore have more than double the chance of relapse at 30 per cent, compared to 13 per cent in those who do not have Ikaros gene deletion,” said Associate Professor Allen Yeoh of the Department of Paediatrics at the National University of Singapore Yong Loo Lin School of Medicine. Together with Associate Professor Tan Ah Moy of the KK Women’s and Children’s Hospital (KKH) and Professor Hany Ariffin from the University of Malaya, the three doctors studied the peculiarities of these children’s leukemia and developed a new treatment protocol that turned out to be successful. Their findings were published online in July in the Journal of Clinical Oncology.
Childhood ALL is the most common form of cancer in children and affects three out of every 10 children who are diagnosed in Singapore annually. The current cure rates for children with ALL stands at 88 per cent in Singapore, and 50 to 85 per cent worldwide. The two-country study is also the first in the world to prospectively show that intensifying therapy for Ikaros gene-deleted children with ALL reduces relapse and improves treatment outcome.
The study, named the Malaysia-Singapore (Ma-Spore) ALL 2010, is a collaboration that involved a total of 346 patients from four hospitals in Singapore and Malaysia – the National University Hospital (NUH), KKH, University of Malaya Medical Centre and Sime Darby Medical Centre (SDMC) in Subang Jaya. The work builds on an earlier 2003 study by the team, which had found that reducing the amount of chemotherapy for paediatric ALL patients led to better outcomes, with a cure rate of 80.6 per cent. However, better solutions were still needed for children with high-risk disease. This led to the findings of the current study.
Although the Ma-Spore study group is only 15 years old and small compared to most cooperative groups, it has contributed important knowledge in the treatment of children with leukaemia, including two important papers in the Journal of Clinical Oncology. In their work, the Ma-Spore team explores critical treatment issues in cost-effective therapy that are important for Singapore and Malaysia, including that of Asian sensitivity to chemotherapy drugs.
“Ma-Spore success is possible because of our unique collaboration, bringing together the many leaders in childhood ALL therapy in Singapore and Malaysia to focus on unique gaps, funded both by government and charity,” Assoc Prof Yeoh added. He is also Head and Senior Consultant at the Division of Paediatric Haematology-Oncology, at the NUH and National University Cancer Institute, Singapore.
Prof Hany Ariffin, who heads the Paediatric Haematology-Oncology and Bone Marrow Transplantation Unit of the University of Malaya Medical Centre in Kuala Lumpur, is proud of the many achievements of the Ma-Spore group. “In addition to the impressive gains in survival rates, the collaboration has also facilitated transfer of knowledge and technology to the team in University of Malaya. This has allowed many children to receive sophisticated personalised leukaemia therapy, irrespective of their socio-economic standing.” Like Assoc Prof Yeoh, she strongly believes in equitable health care for all children with cancer.
The study is funded by the Singapore Ministry of Health’s National Medical Research Council Clinician Scientist Investigator Awards, Cancer Science Institute of Singapore, Children’s Cancer Foundation and Viva Foundation for Children with Cancer. Meanwhile, patients in Malaysia are also supported by research grants from University of Malaya as well as charities.
The team is now working on a new study, Ma-Spore ALL 2020, which will explore further tailoring treatment to optimise the treatment outcome of the children who are expected to fare worse. “The ultimate aim is a complete cure,” said Assoc Prof Yeoh.
“With better tools to study the leukaemia cells and better ways to treat high risk cases, we will be able to identify those who will relapse early, so that we can intervene and cure them.”
See press release.
News Coverage