One in three Singaporeans risks developing diabetes in their lifetime, prompting the Singapore Ministry of Health to declare war on diabetes in 2016. But what many don’t hear about is the silent epidemic of diabetic foot ulcers (DFUs). Up to 25% of patients with diabetes develop DFUs over their lifetime—and 10–15% of DFUs do not heal. Of these DFUs, 25% will require amputation, resulting in more than one million annual limb amputations globally. That is equivalent to one amputation every 30 seconds.
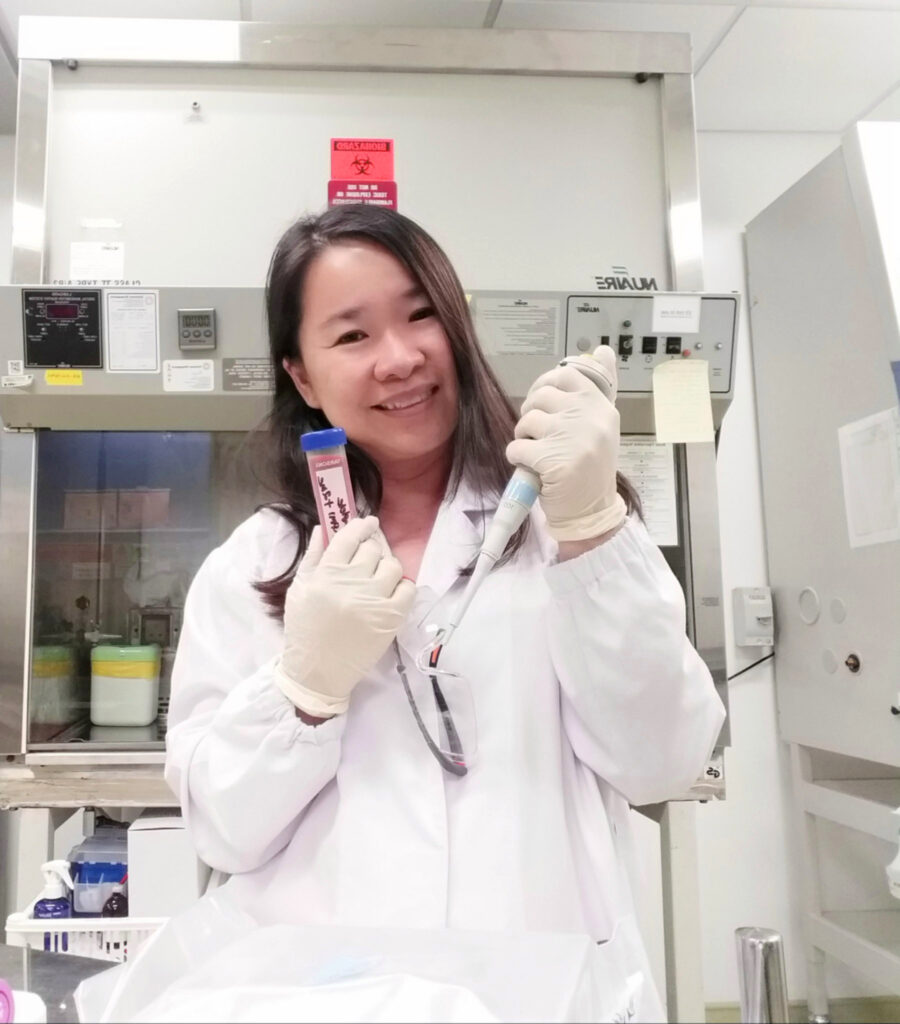
Dr Lim Fui Ping, Senior Lecturer in the Alice Lee Centre for Nursing Studies (NUS Nursing), National University of Singapore Yong Loo Lin School of Medicine, hopes to help end such tragic outcomes. She said, “The use of insulin to combat diabetes has increased the life expectancy of diabetic patients. Yet, complications associated with diabetes such as DFUs have resulted in a sharp increase in the volume of patients at hospitals worldwide.”
More than that, DFUs not only incur significant economic costs to national health systems, but also have a detrimental clinical impact—with people suffering from diabetic foot complications reportedly being more fearful of limb amputation than death.
This led her to question the ultimate goal of treatment. “Is it to lengthen life or alleviate discomfort? Innovation and new advances in medicine meant that we could keep people alive longer than ever before. I began to think of how we could use novel interventions such as stem cells to treat DFUs.”
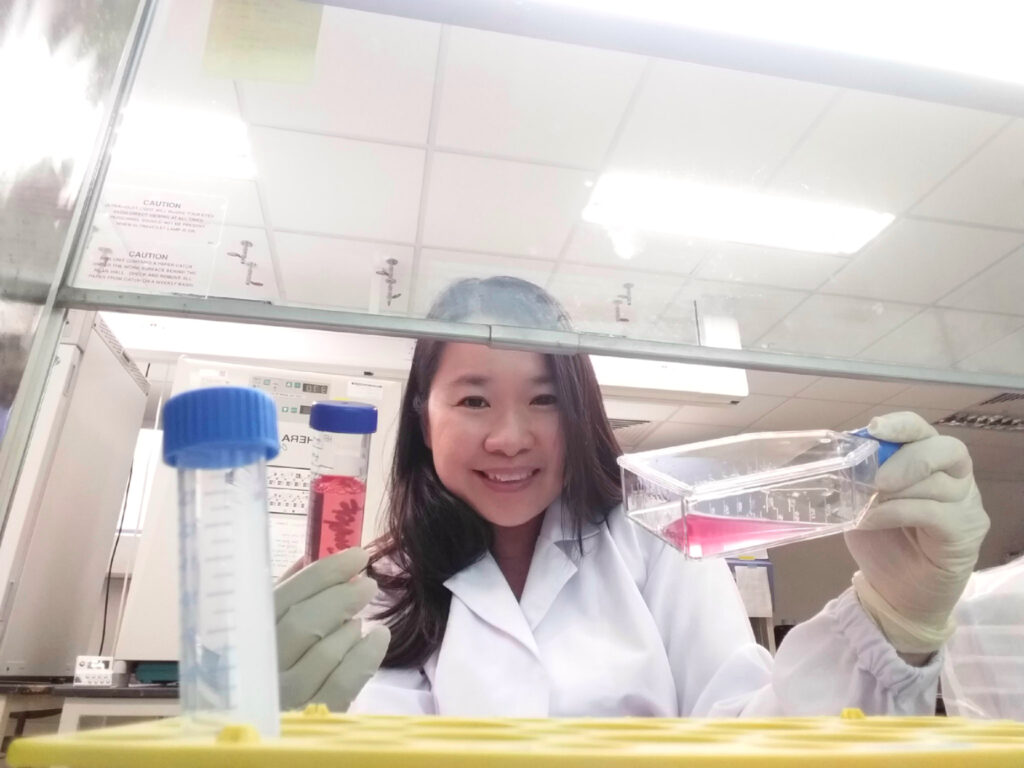
With the academic guidance and practical support from Associate Professor Phan Toan Thang, Principal Investigator of the Wound Healing and Stem Cell Research Group at the Department of Surgery, Yong Loo Lin School of Medicine; Associate Professor Jackie Ho Pei, Senior Consultant of Vascular Surgery in the Department of Cardiac, Thoracic and Vascular Surgery, National University Heart Centre; and Associate Professor Alvin Chua, Assistant Director of Transplant Research at Singapore General Hospital, Dr Lim embarked on a six-year journey to investigate the biological efficacy of mesenchymal stem cells on diabetic wound healing using two animal models.
Putting Theory to Test
Through measuring the effect of cord lining mesenchymal stem cells (CL-MSCs) on wound healing in diabetic and hyperglycaemic animal models, Dr Lim’s study has shown that experiment groups treated with CL-MSCs healed faster compared to the control group. Dr Lim shared, “We also found that anti-inflammatory markers were highest in the group with CL-MSCs injected into the peritoneal, whereas collagen structures were strongest in the group where CL-MSCs were topically applied onto the wound bed.
“It has been demonstrated in our study that CL-MSCs is a promising cell-based therapy for the acceleration of wound closure, given the challenging task of accelerating the closure of a relatively huge wound in a defective wound model. The trends seen in our inflammatory profile suggest that the mechanism involves immunomodulatory effects of CL-MSCs.”
Putting Theory to Work
Dr Lim is wasting no time in putting her intervention to use in the community—her startup, RedDot Wound Care, is working closely with the non-profit charity healthcare organisation, SATA CommHealth to bring the intervention to patients under the organisation’s care.
At this stage, Dr Lim and her team are keeping things simple. “To comply with current healthcare regulations, we use exosomes extracted from CL-MSCs for patients with DFUs. The diverse components of exosomes—which comprises secreted products from stem cells as the primary material—not only reflect their cellular origin, but also endow them with potential therapeutic functions similar to the stem cells.
“One of our most notable cases so far is a patient with a DFU that has not healed for three years—and we managed to close the wound in 16 weeks,” she shared. Beyond bringing relief to the patient, reduction in wound healing time has other implications as well. “Wounds cause pain, suffering, loss of function, psychological distress and a significant decrease in quality of life. The longer a patient has a wound, the likelier it is that complications such as infection, sepsis or limb amputations will occur—which also extends treatment time and multiplies costs.”
Putting Theory to Scale
On what’s next in the pipeline, Dr Lim said, “It is important to take scientific discoveries out of the laboratory and into the field. If we have worked hard to prove a theorem, it is then important to work even harder to ensure that we transform theorem into effective treatments and approaches to improve the health of our population and mankind. That’s the root and original purpose of research, and we will do well to remember that.”
Besides RedDot Wound Care, Dr Lim has also founded The Skin Nurse, with plans to leverage the useful properties of stem cells to promote the regeneration of healthy, functional skin, as well as to limit over-healing and scarring responses.

Dr Lim (left), with A/Prof Phan.
Did you know?
Dr Lim is the first NUS Nursing faculty member to complete a Medicine PhD at Yong Loo Lin School of Medicine, National University of Singapore.