
In August 2023, NUS Nursing students took part in the year-long Longitudinal Patient Experience (LPE)—working for the first time in teams with Medicine, Dentistry and Pharmacy students. How did it go? A lecturer and 2 students share their LPE stories with NUrSing.
On paper, Mr S looked like any other patient. He was in his mid-50s and had kidney disease which required frequent dialysis sessions.
But Mr S also loved collecting Coke merchandise and was an avid motorcyclist before he fell ill. He had a favourite neighbourhood restaurant (Tenderbest) and a regular spot in the park where he enjoyed pondering over the book he planned to write. None of these were captured in his medical history.
Helping Nursing students see beyond their patients’ medical conditions is one of the aims of the LPE segment under the Common Curriculum for Healthcare Professional Education at the Alice Lee Centre for Nursing Studies (NUS Nursing), National University of Singapore Yong Loo Lin School of Medicine.
“LPE is not new to Nursing and Medicine students. It was first piloted by NUS Nursing and NUS Medicine in 2014. With the launch of the Common Curriculum last year, we have expanded the programme to include Dentistry and Pharmacy students—making for richer learning for students. More importantly, it allows them to put theories learnt in the ‘Social and Behavioural Determinants of Health’ and ‘Health Professionalism’ into practice,” said Associate Professor Lydia Lau, Director of Education, NUS Nursing.
The Person—Behind the Patient
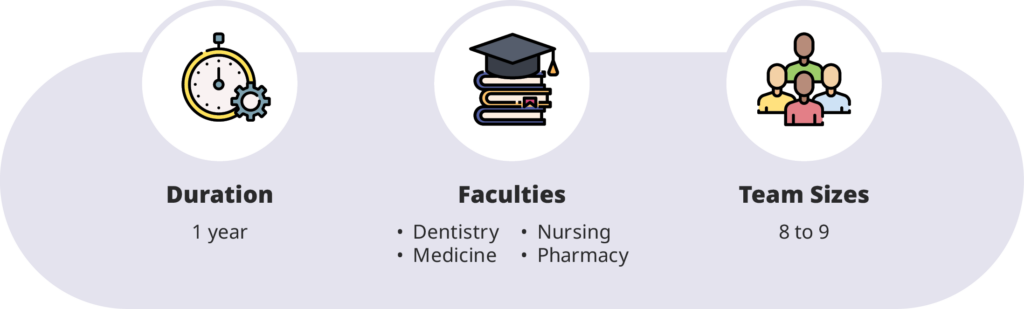
Under the programme, each team comprising 8 to 9 students from Nursing, Medicine, Dentistry and Pharmacy would carry out around 5 house visits to patients over the course of a year, with guidance from a clinical mentor.
One of the NUS Nursing clinical mentors, Lecturer Ms Lubna Shah, explained, “By having the student teams visit patients in their ‘home territory’, LPE aims to have students thinking beyond the medical aspects—such as what medical conditions they have and what medicines they take—to seeing patients in a more holistic manner. Their living conditions, daily habits and so on all inform the way they respond to care.”
LPE participant and NUS Nursing Year 1 student, Chloe Goh, appreciated the way LPE enriched her understanding of patient care. She said, “Typically, we don’t get to see our patients outside of clinical settings. LPE gave us the opportunity to see how they cope when they are at home or out in the community.”
In addition to home visits, the students also had a special mission—to complete a walk around the community with their patients. NUS Nursing Year 1 student, Rashmika Raja Mohan, said, “Our patient, Mr S, showed my team his favourite hangouts in the neighbourhood—such as the places where he buys food and spends his free time. Even though these details have nothing to do with healthcare, it helped us get to know him on a deeper level as a person.”
Ms Lubna added, “The community walk is a very important part of LPE—not only is it patient-led where the patient chooses where to go, it drives home the fact that patients are unique individuals. My students have shared that this realisation has made their healthcare work more meaningful—because they know that they are not just treating a disease, but a person with their own stories, preferences and place in the community.”
The Teams—Caring for the Patient
The LPE programme also brings Dentistry, Nursing, Medicine and Pharmacy students together to learn outside the classroom. Rashmika said, “Even though we come from different disciplines, we’ve already taken some classes together under the Common Curriculum. This helped to break the ice for our first session.”
She continued, “What was eye-opening was the questions my teammates asked—for example, the Pharmacy student would be concerned about Mr S’s medications, whereas my Medicine teammates might want to know about his medical history before diagnosis. These are not necessarily questions that I would have thought to ask myself, and they helped me understand Mr S in a more holistic manner.”
Noting that this is a view shared among many of her students, Ms Lubna said, “Students come in with their different strengths—some may be more data-centric while others are more well-versed in conversing with the patient. These are all necessary strengths. And when students watch their friends contributing in their respective areas of expertise, it serves as positive reinforcement to continue learning from one another.”
NUS Nursing Year 1 student, Chloe Goh, agreed. She said, “Our LPE teams are similar to the multidisciplinary teams we will work in after graduation—and working with my teammates from different specialisations has given me better insights into their thought processes and decisions. Additionally, it served as useful practice for communicating with other healthcare professionals in future.”
A/Prof Lau said, “The learning is not limited to between specialisations. Among Nursing students, our cohort comes from diverse backgrounds—‘A’ Levels, Nursing diploma upgraders and mid-career switchers. These varied life and Nursing experiences can add value to the experience for both the team and the patients.”
The Booster—for Experiential Healthcare Education
Notably, the LPE is different from the rest of the courses in the Common Curriculum—offering students hands-on experience in the community. Chloe said, “Unlike other NUS Nursing courses that are more skill- and theory-based, LPE is a rare opportunity to interact with patients and practise our communication skills.”
Ms Lubna added, “Many first-year students feel nervous about talking to patients during their initial clinical postings—but with this LPE experience, many students realised that patients are usually highly conversant. It takes just a little to get the conversation flowing. So I believe LPE acts as a booster for students’ confidence and prepares them for their attachments to community hospitals.”
Rashmika, who was in the midst of her first clinical posting, has indeed put these skills to good use—and more. She said, “With the LPE experience, I felt well-equipped to speak with patients and other members of the healthcare team. When I noticed I could chip in to help, I would also speak up. For example, there was this time when I saw a doctor having difficulty communicating with a patient who couldn’t seem to hear him well. Because I had successfully interacted with that patient earlier in writing, I was able to share the tip with the doctor.”
The Journey—to Patient-centric Healthcare Professionals

Now that the current run of the LPE has passed the halfway mark, the teams have spent about half a year with their patients.
By spending time with and observing changes in their patients over time, Ms Lubna’s students have also started reflecting on and adjusting their care advice. She said, “One team shared that through their observation, they realised that their patient was already following a healthy diet. Which means general healthy eating advice wouldn’t work so well—and they decided to focus on other areas instead.”
With a couple more months to go, Chloe hopes to help her patient improve mobility and continue bonding with her teammates. “I hope that we can get to know one another better as friends and fellow healthcare students—because who knows, we might just end up working together one day.”
As for Rashmika and her team, they have a surprise in store for Mr S—using the modest budget each team is given to buy a token for their patients. She said, “We are planning to give him a piece of Coke merchandise for his collection—but a small one because his house is already full of merchandise!”
Summing up, A/Prof Lau said, “With the ‘Healthier SG’ vision and its emphasis on total well-being, it has become even more important for healthcare professionals to be able to understand one another’s viewpoints, respect one another and work together. Done right— LPE will shape a more patient-centric and cohesive healthcare system in the future.”

Students having a chat with a patient at home.


