Modified nano-sized cell particles boost cancer immunotherapy, reduce side effects
Published: 16 Sep 2024
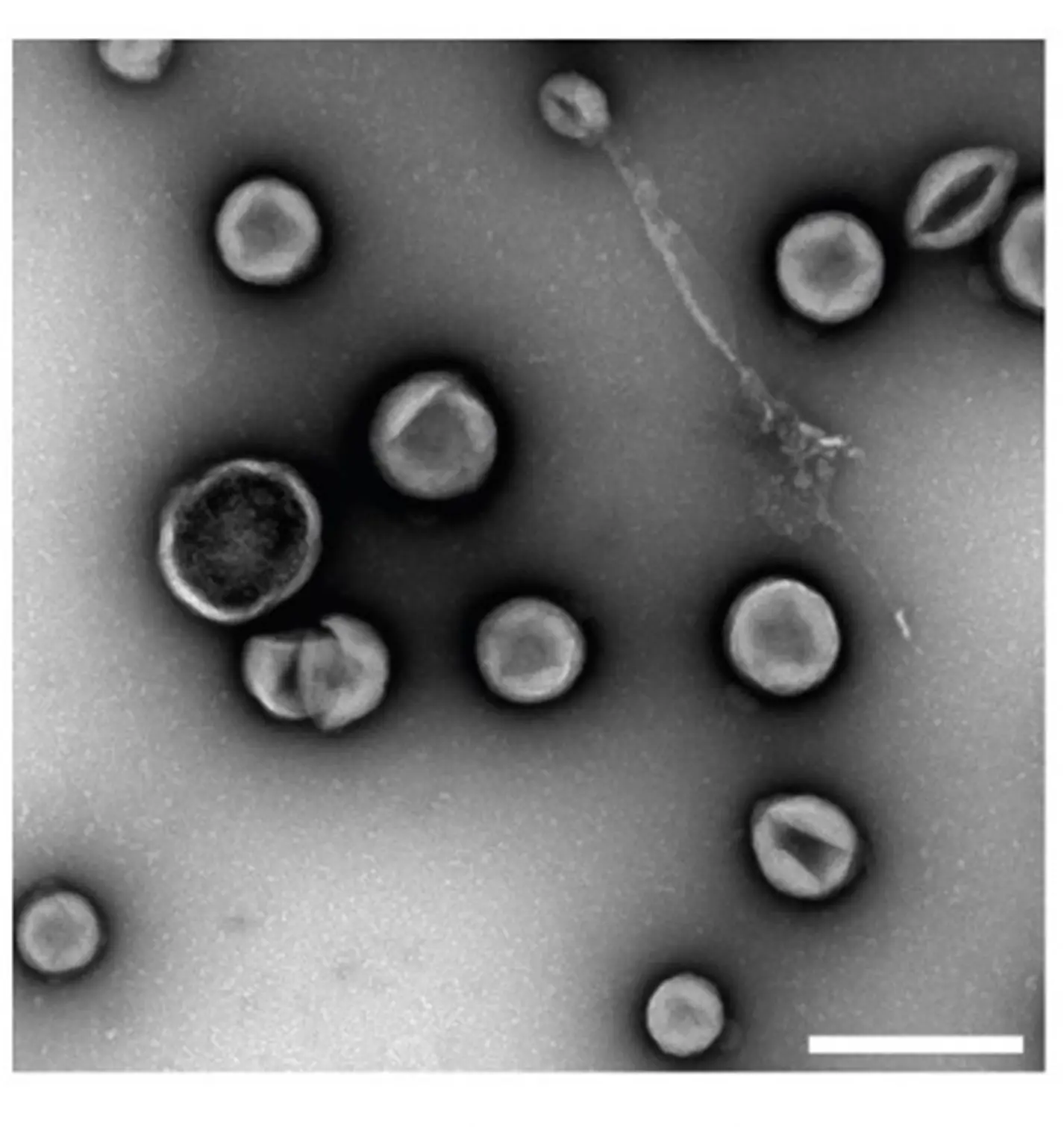
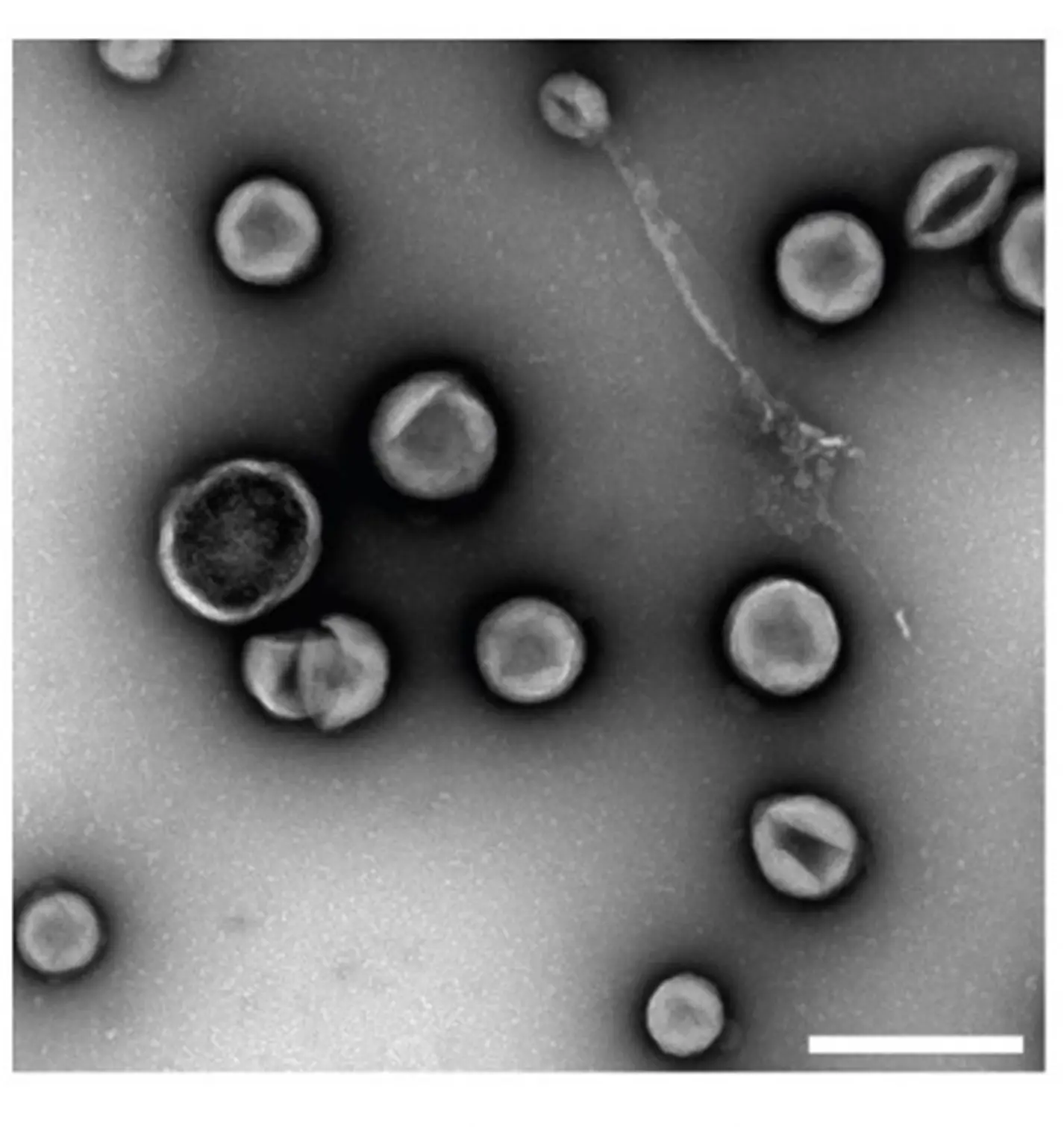
Electron micrograph of engineered extracellular vesicles at a magnification of 23,000× (Credit: NUS Yong Loo Lin School of Medicine)
Immunotherapy is a type of cancer treatment that uses the body’s own immune system to help fight cancer. It works by stimulating the immune response to recognise and attack cancer cells more effectively. The treatment involves using substances that boost the immune system, teaching immune cells to target cancer, or using engineered cells to specifically target and kill cancer cells. While it is a key approach in cancer treatment, the effectiveness of immunotherapy is limited by the risk of immune-related side effects, because the immune system, while targeting cancer cells, may also attack normal, healthy tissues. These side effects include inflammation or damage to various organs and tissues, causing a range of symptoms or complications in health outcomes.
A team led by Assistant Professor Minh Le from the Institute for Digital Medicine (WisDM) and Department of Pharmacology at the Yong Loo Lin School of Medicine, National University of Singapore (NUS Medicine) has unveiled a novel delivery platform that significantly enhances the effectiveness of cancer immunotherapy while reducing the associated side effects. This innovative approach, leveraging nano-sized particles released by cells, termed “extracellular vesicles” (EVs), represents a major advancement in the field of cancer immunotherapy.
In the study, the researchers developed a technique which modified EVs to carry multiple immune-boosting molecules called ‘immunomodulatory ligands’, for the treatment of in vivo models of metastatic pancreatic cancer and melanoma. The approach enhanced the therapeutic effectiveness of the ligands—particularly the subset Tumour Necrosis Factor Receptor Superfamily (TNFRSF) agonists, which are key in controlling immune responses against cancer. The team also found that the delivery method enhanced retention of the immune-boosting ligands in the tumour—allowing for better therapeutic effects to be achieved with lower drug doses, which in turn reduced the risk of side effects that are often seen in current immunotherapeutic treatments.
Published in Molecular Therapy, the study demonstrates that the new EV-based delivery approach can alter the tumour’s immune composition to improve treatment outcomes of patients with cancer. Notably, the approach was consistently proven to show better outcomes in terms of tumour-specific immune activation, suppression of tumour burden, overall survival and resistance to tumour rechallenge (or recurrence), compared to the current clinical standard of care, whereby the ligands are administered in their free soluble form without the EV-based delivery platform. This is remarkable as it indicates that the EV-based delivery approach is able to enhance the treatment of existing tumours and prevent the recurrence of the same cancer in the future via the development of tumour-specific immune memory.
Asst Prof Minh Le said, “We are thrilled to present this novel EV-based delivery system that not only enhances the therapeutic efficacy of immunomodulatory ligands but also significantly reduces systemic toxicity. Our findings pave the way for safer and more effective cancer immunotherapies, potentially transforming the landscape of cancer treatment.”
Read more in the press release here.