New tumour-selective light treatment could kill breast cancer cells with greater accuracy and improve tumour control
Published: 19 Jul 2023
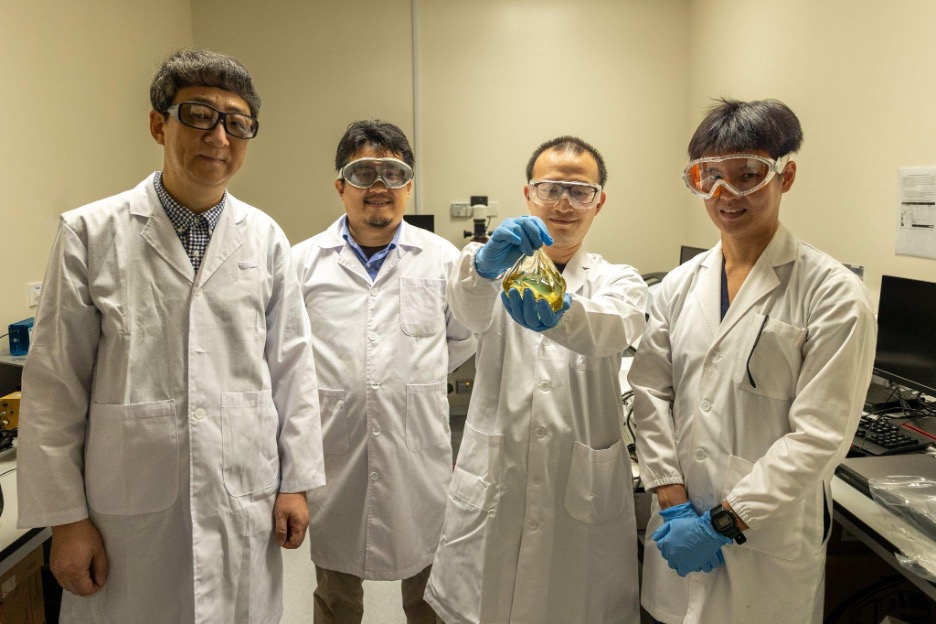
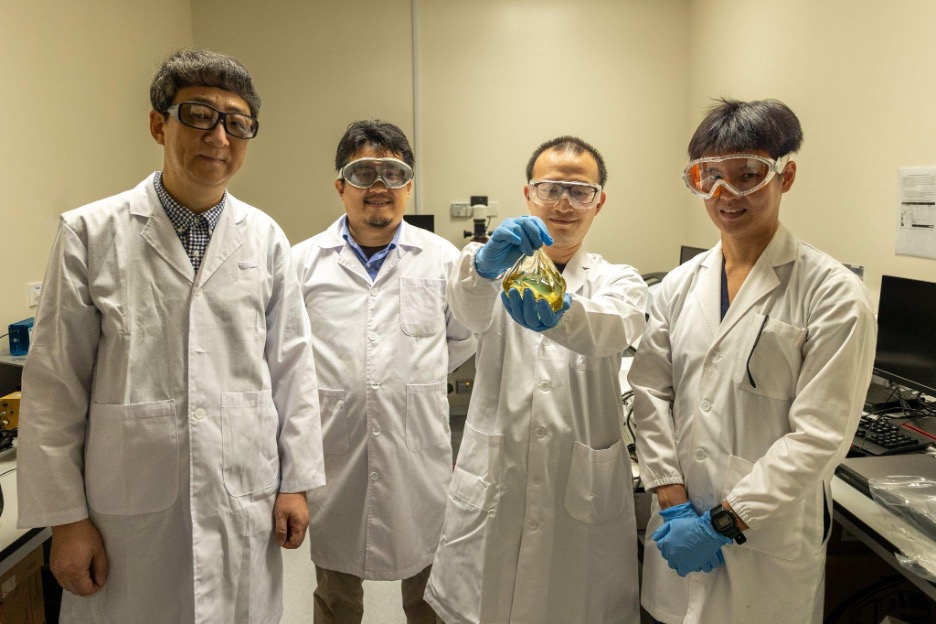
(From left to right) Professor Zhang Yong from the Department of Biomedical Engineering in the College of Design and Engineering, NUS, Assistant Professor Daniel Teh from the Department of Ophthalmology and Anatomy at the Yong Loo Lin School of Medicine, NUS (NUS Medicine), Dr Sun Bowen, Research Fellow at the Department of Biomedical Engineering in the College of Design and Engineering, NUS, and Dr Aaron Foo, Senior Resident at the National University Hospital. They are holding a sample of the breast implant developed for the treatment.
Breast cancer is the most common cancer affecting women in Singapore. Treatment is multimodal and often involves surgery to remove the cancer and lymph nodes involved.
Studies have shown that patient satisfaction has increased with breast conserving therapy (BCT) where only the tumour and a margin is removed from the body post mastectomy. For BCT, radiotherapy has to be administered after lumpectomy, which removes other abnormal tissue from the breast and some normal tissue around it. Since radiotherapy is used to induce tumour damage, there is a small risk of toxicity to the skin, lung, heart and remaining breast tissues.
To avoid the side effects and improve quality of care for breast cancer patients, a multidisciplinary team comprising medical researchers, bioengineers and clinicians from the National University of Singapore (NUS) and National University Hospital (NUH), led by Assistant Professor Daniel Teh from the Department of Ophthalmology and Anatomy at the Yong Loo Lin School of Medicine, NUS (NUS Medicine) and Professor Zhang Yong from the Department of Biomedical Engineering in the College of Design and Engineering, NUS, have, successfully delivered tumour-selective light treatment to breast cancer cells. This mode of treatment, known as photodynamic therapy, was shown to be effective in breast cancer preclinical models in their recent publication in ACS Nano.
The team worked to improve the delivery of light to tumours that lay in tissues deeper in the skin. They engineered a biologically compatible silicone breast implant loaded with nanoparticles that can be activated by highly tissue-penetrant near-infrared light. This can be converted into visible light needed for the activation 5-ALA, an FDA-approved light-activated drug which can unleash a tumour killing effect without killing cells in other regions.
“This discovery has the potential to significantly augment existing breast cancer therapies. Being able to selective destroy tumour cells without inducing adjacent tissue damage confers a significant advantage in cancer treatment. While it will probably not replace existing mainstream treatment modalities, it may still indirectly lead to a reduction in chemotherapy and/or radiation dosage by improving local tumour control,” said Asst Prof Teh.
This photodynamic therapy is a useful addition to the arsenal of existing therapies for breast cancer. When used alongside conventional treatments, photodynamic therapy can possibly reduce disease burden and indirectly help to lessen treatment-related toxicities with conventional therapies.
Read more in the media release here.