Nurses today increasingly work in interdisciplinary teams—alongside other healthcare professionals such as doctors, pharmacists and therapists. To prepare students for real-world interprofessional collaboration, NUS Nursing is taking steps to equip them with communication and teamwork skills.
One such initiative is the research project, “Improve teamwork and communication skills with TeamSTEPPS in simulation-based interprofessional education”, by Dr Chua Wei Ling, Assistant Professor, Alice Lee Centre for Nursing Studies (NUS Nursing), National University of Singapore Yong Loo Lin School of Medicine.
First Step: Establishing Effectiveness of Simulation in Teaching TeamSTEPPS
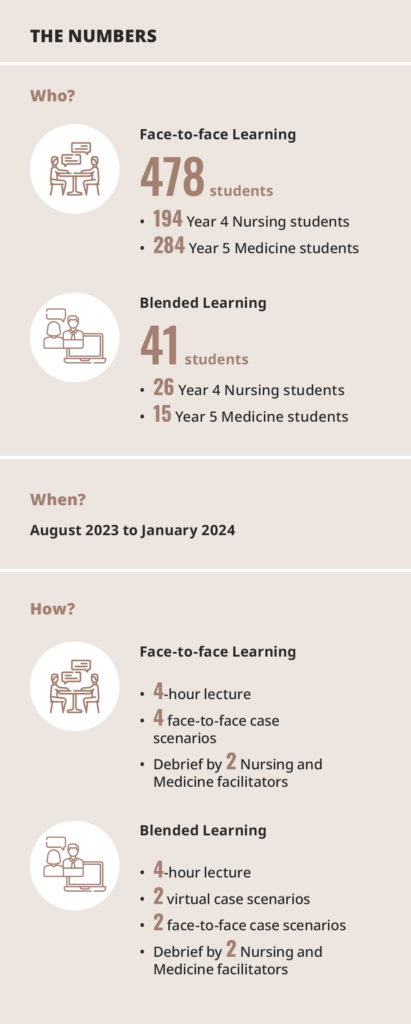
From August 2023 to January 2024, the project trained 220 Year 4 Nursing students and 299 Year 5 Medicine students in using the Team Strategies and Tools to Enhance Performance and Patient Safety (TeamSTEPPS) framework through simulation. “We chose these 2 groups of students because they are in their final year—soon to graduate and expected to play their part in such interprofessional settings,” said Dr Chua.
In the programme, students were introduced to the TeamSTEPPS framework in a 4-hour lecture, before being divided into mixed groups of Nursing and Medicine students. Each group went through 4 case scenarios, with each student getting to roleplay at least once. They were then debriefed by a pair of Nursing and Medicine facilitators.
Dr Chua said, “This was the first time we had interprofessional facilitators from the Nursing and Medicine disciplines for our simulation classes—and the feedback was overwhelmingly positive. The students shared that besides learning from their facilitators’ clinical experiences, they also saw first-hand how interprofessional communication looked like in the facilitators’ interactions with one another.”
The value of the project in preparing students to become capable healthcare professionals was apparent. However, the project had to confront challenges in timetabling, manpower and finding lab space—perennial problems for interprofessional education (IPE) initiatives.
Dr Chua said, “Nursing and Medicine run on different timetables—making it hard to find common timings for both cohorts to train together. Running such face-to-face simulation programmes is also highly resource intensive in terms of manpower and space. That inspired us to make the programme sustainable by piloting a version that incorporates blended learning. The aim was to reduce manpower needs and timetable clashes,” Dr Chua said.
Next Step: Trialling the Blended Learning Approach
To trial the effectiveness of the blended learning approach, 26 Nursing and 15 Medicine student volunteers were recruited. Dr Chua explained, “Compared to the main cohort who did all 4 case scenarios in a face-to-face setting, students who went through the blended learning format did 2 cases virtually and 2 cases physically. They would first attend the 2 virtual cases in the morning before returning to campus in the afternoon for the 2 physical cases.”
For the virtual case scenarios, the students could log in remotely, which reduced the need for lab space and standardised patients. In addition, the blended learning format also enabled the students to practice the TeamSTEPPS teamwork and communication strategies in a tiered manner. Dr Chua said, “For the face-to-face case scenarios, students had to perform the necessary clinical skills such as intubation or resuscitation—while applying the TeamSTEPPS concepts—from the get-go.
“Conversely, students starting off with virtual case scenarios could focus on practising the TeamSTEPPS concepts without the stress of having to perform clinical skills. Then when they come together for the face-to-face case scenarios subsequently on the same day, they could apply both TeamSTEPPS and clinical skills all at once.”
Dr Chua said, “Students shared that because they met and worked together with one another on cases virtually first, by the time they got together physically, they felt like they could jump right into the case scenarios as a team. There was less anxiety—and they were able to work together more effectively.”
Future Step: Scaling Up Blended Learning to the Whole Cohort

Analysing feedback from the students, Dr Chua felt encouraged by the response—over 95% of the students felt that the programme improved their knowledge, confidence and ability to communicate and work collaboratively with one another. “Despite the challenges, the feedback has affirmed the value of carrying out this IPE initiative.
“It’s especially validating when we hear from Medicine students how the experience opened their eyes to what nurses can do, or when our Nursing students share how they can now better understand the doctors’ line of reasoning,” she said. “While the team will continue with the face-to-face programme format for upcoming batches of final-year Nursing and Medicine students, there are plans to fully adopt blended learning eventually.
“We are preparing for that right now, starting with ironing out technical issues such as ensuring that the system is stable enough to host the entire cohort of students, and training our facilitators on use of the virtual platform.”