Issue 37 / February 2021
INSIGHTS
Epigenetics Opens Door to New World of Medicine

he term “epigenetics” used to conjure up memories of only what we have read about in the Dutch winter famine1, or studies on the Developmental Origins of Health and Disease2. But research has come a long way with the dissecting of epigenetic molecular mechanisms. With the growing discovery of epigenetic factors that drive cell fates or control cellular gene expression, we are seeing their real value as medicines spring from the identification of these epigenetic mechanisms. It is an exciting time to witness the threshold as new medicines now ‘cure’, rather than the conventional ones that simply slow down the course of disease.
As the world woke to yet another day of a relentless barrage of COVID-related news, a group of North American clinician-scientists released (with little fanfare?) the results of a landmark human clinical trial on gene therapy for Beta-Thalassemia and Sickle-Cell Disease3. Some have called this “molecular surgery”, because it is a permanent change that actually cures the disease. The work showed that the scourge of life-threatening blood disorders, which plagues millions of lives worldwide, can be achieved through CRISPR-editing of a gene ‘enhancer’ active only in blood cells. Gene enhancers are the epigenetic switches in our genome.
Problematic transcriptor factor crisply edited CRISPR is becoming a household name, accompanying the publicity boost from recent Nobel laureates, Jennifer Doudna and Emmaneulle Charpentier, who were celebrated for their pioneering work on CRISPR gene editing. This technology can be targeted to protein-coding genes, which comprises only 2% of the human genome, and can also be targeted to epigenetic switches, found in the rest of the 98%, and which drive gene expression and cell behaviour.
Patients who suffer the blood disorders lack the healthy version of haemoglobin in their red blood cells and cannot carry oxygen effectively. These haemoglobin proteins appear in the first six months of life to replace fetal-haemoglobin, which performs the same role, but at the fetal stage (when the baby is still in the womb). Scientists realised that the switch from fetal to adult-haemoglobin is controlled by a transcription factor. By suppressing this transcription factor, it becomes possible to retain high levels of healthy fetal-haemoglobin, thence overcoming the issue of the lack of adult-haemoglobin.
CRISPR gene editing can be targeted to protein-coding genes, which comprises only 2% of the human genome, and can also be targeted to epigenetic switches, found in the rest of the 98%, and which drive gene expression and cell behaviour.
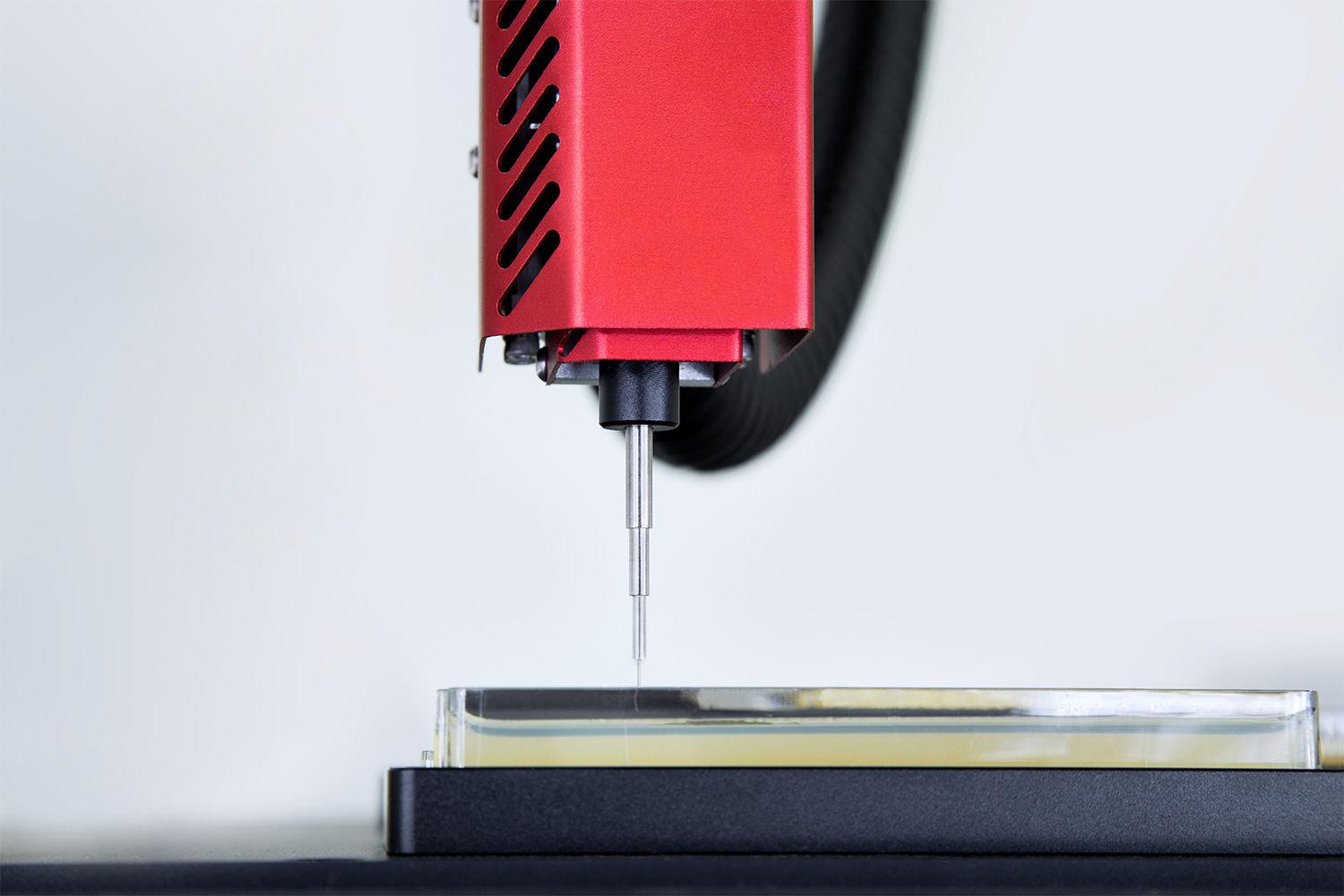
More intricately, the scientists identified the enhancer region of the transcription factor gene, which is specifically active only in blood cells, and responsible for regulating the abundance of this transcription factor. Now, by CRISPR editing, targeted to this enhancer region—one of our eponymous ‘epigenetic switches’—we have the molecular surgery that turns off the expression of the transcription factor, allows for sustained production of fetal-haemoglobin, and provides the cure so that red blood cells now have sufficient oxygen-carrying function.
This work is a brilliant example of how molecular insights, built upon molecular technologies, may bring an end to human suffering. We are now finally reaping the benefits from the human genome sequencing project accomplished about 20 years ago. Together with CRISPR technology, the future for gene therapy is promising. Epigenetics is no longer just observations or phenomena yet to be understood. We are taking firm strides into the new world of medicines that set out to cure.
-
https://www.nytimes.com/2018/01/31/science/dutch-famine-genes.html.
-
https://pubmed.ncbi.nlm.nih.gov/27609592/.
-
https://www.nejm.org/doi/full/10.1056/NEJMoa2031054.