Women diagnosed with the biologically aggressive triple-negative (TNBC) and endocrine-refractory subtypes of breast cancer confront a bleak prognosis because they respond poorly to conventional chemotherapy. Researchers from the NUS Yong Loo Lin School of Medicine have discovered that combining one of the most widely prescribed medication class for type 2 diabetes mellitus known as thiazolidinediones (TZD), with an emerging class of cancer drugs known as histone deacetylase inhibitors, elicits robust anti-tumour responses in preclinical models of these breast cancer subtypes.
In the study led by Assistant Professor Alan Prem Kumar from the NUS Centre for Cancer Research and published in Cell Death and Discovery, the NUS researchers leveraged on big-data analytics of 3,992 human breast cancer specimens, and found that cellular levels of PPAR-gamma were associated with survival outcomes in breast cancer. Higher levels seemed to correlate with better prognosis. This led the study authors to hypothesise that activating the PPAR-gamma pathway could represent a novel therapeutic strategy against breast cancer.
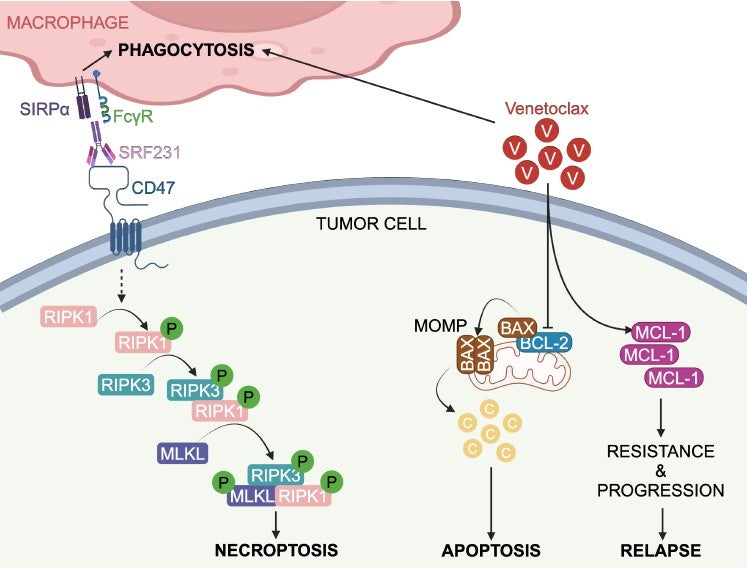
They also observed that levels of PPAR-gamma in cancer cells were inversely correlated with expression of certain histone deacetylases (HDACs). Further experiments revealed that this is because HDACs, proteins that regulate the expression and activity of genes by altering DNA compaction, led to reduced PPAR-gamma levels in cancer cells. Interestingly, prognostically-poor subtypes of breast cancer such as triple-negative breast cancer and endocrine-resistant breast cancers, were found to have high levels of HDAC activity and lower levels of PPAR-gamma.
The researchers found that individually, TZDs and HDAC inhibitors had limited anti-tumour effects when used as single agents. However, when both classes of drugs were administered concurrently, the combination treatment was synergistic and greatly stalled disease progression in mouse models of triple-negative breast cancer and endocrine-resistant breast cancer.
One of the clinically important aspects of this study is the “repurposing” of existing, US FDA-approved drugs. Drug repurposing, also known as drug repositioning, refers to a strategy of redeploying ‘old drugs’ in drug discovery. “This is an attractive proposition because ‘older drugs’ usually have well-known and established safety profiles, which de-risks the drug development process and can shorten approval timelines” according to Dr Nicholas Syn, one of the lead authors of the study.
Dr Loo Ser Yue, another of the lead authors in the study added, “This anti-tumour effect was mediated not only through the direct effect of combination therapy on restraining cancer cell proliferation, but also by curbing the growth of blood vessels which supply nutrients and oxygen to cancer cells (also known as ‘angiogenesis’). Remarkably, we also found that although HDAC inhibitors potentiate the cytotoxicity of TZDs against aggressive breast cancer cells, normal healthy cells were spared from the cell-killing effect of this combination drug regimen.”
Cancer is a leading cause of death and illness worldwide, and represents a present and growing challenge in Singapore. As such, the NUS Centre for Cancer Research (N2CR) aims to develop innovative new ways to detect, cure and prevent cancer by undertaking internationally leading fundamental research that advances the understanding of cancer, and by translating these research discoveries into clinical practice to benefit patients. Research aspires to further understand key genetic and epigenetic changes that drive the origin and progression of cancer in different tissues, particularly those forms prevalent in Asia; develop new therapies to target specific cancers in specific patients; and gain insights into the genetic and environmental variations that underlie cancer susceptibility.
N2CR is carefully organized to motivate interdisciplinary collaborations – spanning from bench to bedside and back again – to drive research in key areas. The programme empowers fundamental and clinical researchers from NUS Medicine, the Cancer Science Institute, the National University Cancer Institute Singapore and the National University Health System to work together, alongside scientists and technologists from other disciplines, to address major challenges. The work is enabled by cancer site-specific resources which include the collection of patient samples and databases with clinical information. It will focus on three cross-cutting themes that promote powerful interdisciplinary collaborations between fundamental researchers, enabling technologists and clinical investigators.
More details can be found in the press release here.
For link to article in Cell Death and Discovery, please click here.