How perceptions of residents toward assessment influence learning: A qualitative study
Published online: 7 January, TAPS 2020, 5(1), 46-53
DOI: https://doi.org/10.29060/TAPS.2020-5-1/OA2080
Jaime L. Pacifico1, Julie Anne S. Villanueva1, Sylvia Heeneman2 & Cees van der Vleuten2
1Internal Medicine, De La Salle Medical and Health Sciences Institute, Philippines; 2Maastricht University, The Netherlands
Abstract
Any form of assessment activity will act as a stimulus and provoke an educational response. There is a risk however that the response will not result in a beneficial educational response, thus there is a need to monitor and understand the relationship between assessment and learning. This is true at any level of education including postgraduate medical education. To understand how residents perceived assessment, we interviewed 20 residents from the departments of internal medicine and paediatrics. Our goal was to determine how assessment influenced their motivation to accumulate knowledge and skills and attain the competence levels expected of a specialist. We utilised grounded theory to analyse the data. Our results showed that the trainees acknowledged that assessment, in general, has a positive influence on their learning, it motivated them to study and fostered an active learning attitude. A high degree of self-directed learning was also present among the residents. An interplay of new or interesting patient cases, concern for the welfare of the patients, engagement with the consultants, and a supportive environment contributed to creating the motivation for the residents to study.
Keywords: Assessment, Perceptions, Postgraduate Medical Education, Qualitative Study, Clinical Training
Practice Highlights
- Any form of assessment activity serves as a stimulus and provokes an educational response.
- Assessment in residency motivated the trainees to study and fostered an active learning attitude.
- Perceptions of credibility, fairness and commitment of assessors to trainees’ welfare matter.
- Patients, engagement with consultants and a supportive environment contributed to motivation.
I. INTRODUCTION
Any form of assessment activity will result in an educational response, however, the unpredictability of this response requires careful monitoring to realise the desired educational outcomes and to recognise the unwanted effects (van der Vleuten, 1996). Assessment can influence how a student learns through the content, design and scheduling and regulatory structure of the assessment program (Schuwirth & van der Vleuten, 2010). When does assessment itself become a barrier to learning and when does the response to assessment promote learning? Holmboe, Durning and Hawkins (2018) assert that the responsibility lies on the program administrator of any assessment program to conduct a systematic review on the potential consequences of any assessment exercise, whether positive or negative, regardless whether the examination is conducted in the classroom or at a national level. Through the years, decisions about method of assessment are primarily based on consideration of its validity and reliability (Norcini & McKinley, 2007). But is this indeed the only attribute of an assessment procedure that is of importance? An in-depth and systematic review of any assessment program on the potential consequences compels that the perceptions of the trainees are included.
When non-medical higher education students were asked about assessment, they talked about fairness instead of validity. It was clear that fairness as alluded to by students, is a representation of how the educationalist defines validity (Sambell, McDowell, & Brown, 1997). In a review involving non-medical higher education students, it was shown that approaches to learning are strongly influenced by the students’ perceptions of the assessment methods (Segers, Nijhuis, & Gijselaers, 2006; Struyven, Dochy, & Janssens, 2005). The same relationship between assessment and approach to learning is echoed in studies involving nursing students in clinical and classroom settings (Leung, Mok, & Wong, 2008; Tiwari et al., 2005). Among medical students, it has also been shown that students would adapt their learning strategies to the perceived requirements of the evaluation (Newble & Jaeger, 1983). These studies substantiate the well quoted maxim that assessment drives learning, although as McLachlan (2006) argues the oft-repeated axiom ‘assessment drives learning’ is misleading and is more complicated, for example, different students are motivated by different reasons and assessment does not influence learning in all contexts.
In postgraduate medical education, whether assessment is a driver of learning and how it directs learning is less established. The continuing challenge for the program directors and clinical faculty is to understand the relationship between assessment and learning and to be able to promote learning as intended (van der Vleuten, Schuwirth, Scheele, Driessen, & Hodges, 2010). In postgraduate medical settings, it is of paramount importance to evaluate the educational effects of assessment, because of the high stakes and risks involved. Although such is also expected in undergraduate medical education, according to Holmboe, Hawkins and Huot (2004), “residency is the last structured experience to ensure that young physicians have sufficient clinical skills” (p. 874) thus the urgent and serious need to influence learning through assessment methods done in clinical training.
The remaining intriguing question in postgraduate medical training is, how do the trainees perceive their current assessment practices and how do these facilitate their learning? Given this research question, we conducted this study to: 1) look into the perceptions of postgraduate trainees undergoing residency training as to how assessment practices influence their motivation to accumulate knowledge and attain the competence levels expected of a specialist, and 2) to determine if there are identifiable conditions or factors associated with assessment practices that can facilitate or deter learning.
II. METHODS
A. Setting
The study was done among residents of the internal medicine (IM) and paediatrics departments at De La Salle University Medical Center (DLSUMC) in the Philippines. DLSUMC serves as the academic institution of De La Salle University College of Medicine. Undergraduate medical education in the Philippines requires a bachelor’s degree and postgraduate medical education such as residency is done after passing the national licensure examination. The duration of residency in IM and paediatrics is three years and is a prerequisite to further training such as adult or paediatric cardiology. Evaluation of the residents included assessment of their knowledge and skills which were done through summative written examinations, mostly multiple choice questions, and Objective Structured Clinical Examinations (OSCEs), attitudes were assessed through a Likert-scale questionnaire. The OSCEs consisted of 12 stations. The scope of the written examinations and the OSCEs include the presentation, diagnosis, and management of the major and more common IM diseases. These assessment methods are done at least twice a year, throughout the three years of training. The examiners are the consultants belonging to the department of IM. During the time this study was done, there was no assessment that involved direct observation of the trainees other than through OSCEs.
B. Data Collection
A convenient sampling was done of second- and third-year residents in both departments since we needed trainees who have already experienced at least one year of training and have experienced several assessment processes. Twenty residents were interviewed for this study, ten males and ten females. Fourteen residents were from the department of IM and 6 were from the department of paediatrics. Seven were third-year residents and 13 were second-year residents during the time of the study. The interviews were conducted by a single person, who was not connected to the current training program of any of the departments. The interviews were done in both English and Filipino and the interviews were later transcribed in English. The interviews lasted from 45 minutes to 1 hour per subject. The residents were notified the interview was voluntary. A semi-structured interview was done using a published guide initially (Dijksterhuis, Schuwirth, Braat, Teunissen, & Scheele, 2013). However, consistent with the iterative nature of grounded theory and utilising constant comparison the interview questions were modified as initial results became available, which informed the succeeding interview guide.
C. Data Analysis
A grounded theory was used to explore how postgraduate trainees in IM and paediatrics perceived assessment of their knowledge and skills during training, and the contributions of these assessments to their learning and their clinical performance (Charmaz, 2014; Glaser & Strauss, 1967; Watling & Lingard, 2012). Grounded theory is an inductive method which allows theories to emerge from the data gathered. Simultaneous data collection and analysis were done which is characteristic of grounded theory. All the interviews were transcribed and during the early data analysis, some of the concepts that emerged from the early transcripts were utilised to guide in the ensuing interviews. Constant comparative method was employed throughout the data analysis. Codings were subsequently organised into concepts and elevated to categories. There was consultation and comparison between JLP and JAS with regard to the codes and analysis of the collected data. During the coding process, memos were written that elaborated on the different codes. Data collection was stopped when saturation was attained, by saturation we mean the data were leading to recurring themes and there was adequate data to support a theory that is comprehensive and credible. In addition, for saturation, our emphasis was on the quality of data rather than its frequency (Morse, 1995). Cognizant of the effects of the researchers in the data collection and analysis and subsequent creation of concepts and knowledge, the background of the different authors are as follows: JLP is a practising internist and cardiologist, and has been a faculty in the college of medicine for many years. He was former chair of the department of IM. JSV is a recent graduate of IM training. SH is a biologist with an educational background. CvdV has training in psychology and psychometrics with many years of engagement in medical education and medical education research. This is the second study together of JLP, SH and CvdV.
III. RESULTS
There was a general positive acceptance among the trainees regarding the role of assessment in their training, as discussed under ‘assessment and its impact’, below. There are two important categories that came out from our data, we called these categories: the mediating factors and stronger motivators. We define mediating factors as prerequisites for learning, these preconditions were necessary for assessment to be meaningful to the trainees. The second category we termed the ‘stronger motivators’. These were situations/conditions which we discovered to contribute to the motivation of the trainees to learn, they were equally as important as the actual assessment in influencing the trainees positively and driving them to strive to be better clinicians. Table 1 summarises the results.
| Categories | Sub-Categories |
| Mediating factors | Credibility of assessment |
| Fairness/unfairness | |
| Interpersonal relations | |
| Commitment of assessors | |
| Stronger motivators | Interesting/new cases |
| Concern for patient’s welfare | |
| Engagement with consultants | |
| Supportive environment |
Table 1. Summary of results
A. Assessment and Its Overall Impact
The trainees agreed that assessment had a positive influence on both their clinical education and performance.
“Assessment improves knowledge of a case, lack of knowledge of a case motivates me to read more in the same way that poor performance prompts us, residents, to exert efforts to improve.”
(IM-1)
One perceived effect of assessment was that trainees were more conscious of their actions especially at the bedside and this improved clinical performance. The residents agreed that assessment positively influenced their learning because:
“I was forced to study and ask questions, learned to prioritise and manage cases, and even one’s personality tended to improve.”
(IM-4)
Assessments improved clinical performance as residents were inclined to study more, facilitating that when they would encounter these cases in the future, they would be more prepared to manage such cases. The OSCE had a positive effect on clinical performance by testing the confidence of the residents.
“You are face to face with the consultant during the OSCE, so it will test your confidence. You may know it theoretically but anxiety can get in the way… at least here they practice in practicals how to explain well even when you are with consultants or seniors.”
(P-1)
For some residents, assessment had a constructive impact on their day to day duty by being aware of what mistakes to avoid and by knowing which patients to give more attention to. Many of these beneficial effects followed on the awareness and what was learned through mistakes in the past, which were facilitated through the assessment practices.
B. Mediating Factors
Although there was a general agreement among the participants in the study that an assessment program had beneficial educational and clinical performance effects, there were certain minimum conditions that were perceived as necessary so that the assessment would be meaningful and would have an impact. These mediating factors that facilitated learning and had an impact on the clinical performance are credibility, fairness, interpersonal relations (between the trainees and supervisors), and commitment.
As for credibility, if the assessment was not perceived as valid, it had no influence on resident learning and performance. The educational role of assessment was readily lost if there was uncertainty regarding the validity of the evaluation.
“If I do not agree with the evaluation it will not have an effect on my performance.”
(P-2)
There was also a perception among the trainees that receiving an unfair assessment would demotivate a trainee, wherein the trainee stopped to try hard since his/her efforts were not properly judged.
“If you receive a wrong assessment… you lose the motivation to pursue to learn, the work becomes very tedious and a lot of your energy is spent being anxious.”
(IM-4)
The evaluator had to have more than superficial knowledge of the residents they were evaluating. Several trainees expressed that they doubted the ability of their consultants to evaluate them effectively in the absence of sufficient interaction between the consultants and the trainees. Another perception was that the consultants did not really see them at work, at the emergency room for example, yet were asked by the department to evaluate them, which obviously caused concerns on the validity of their evaluation.
The last mediating factor was the perceived commitment of consultants towards their role as evaluators. Some expressed doubt about the commitment of the consultants who were evaluating them because of the perception that they were spending limited time in performing their role as evaluators. Such perception tended to undermine the positive effects of their presence and participation in the training of the residents.
“Our consultants who evaluate us who are perceived to be sincerely concerned with us as trainees, have more impact in clinical performance.”
(IM-2)
C. Stronger Motivators to Study and Perform Optimally
Although many trainees thought that assessment had an impact on their learning and performance, we identified some peripheral factors inherent in the training program which served as a catalyst, increasing the motivation of the residents, these effects were either independent of the assessment process or in conjunction with it. These factors or conditions that promoted a stronger incentive for the residents were: interesting and/or new cases, concern for patient’s welfare and/or outcomes, engagement with consultants and a supportive environment.
D. Interesting and/or New Cases
This was the strongest motivation as expressed by the trainees, both as a reason to study or to improve their clinical performance. Exposure to new cases motivated more than examinations or grades to study. New cases refer to diseases or conditions they have not seen before or rarely see such that encountering these motivates them more, giving them the needed confidence to handle such cases better in the future.
“I am more driven by the cases I see and I am happy when faced with something I do not know.”
(IM-4)
E. Patient’s Welfare or Outcome
Many residents found a strong incentive to study harder during their rotation in a particular ward out of a sincere desire to contribute significantly in the recovery and successful management of the patients they handled or encountered. This consideration for a good outcome of their patients created a strong desire to learn more about the case. A trainee expressed that his/her goals had significantly changed from pleasing their consultants as a first year resident to pleasing their patients as a third year resident.
“But on day-to-day duties my motivation already shifted since I am more confident now. During my shift, my goal is on how I can help the patient get better, rather than how I can please the consultants.”
(IM-4)
F. Engagement with the Consultants
It was a prevailing view of many of the trainees that interactions with consultants increased motivation to study or to perform better.
“Interaction with consultant is the best reinforcement to learning and has impact on daily duties.”
(IM-3)
The intermittent moments of one-on-one interaction between the trainee and the consultant was a much valued teaching-learning opportunity for the residents, was something residents awaited and had the impact of creating a strong incentive for them to study. These interactions were a critical affirmation for the trainees and had a crucial influence on facilitating the development of competence they need as future clinicians.
G. Supportive Environment
A learning environment that encouraged the trainees to try to excel was crucial so that the trainees would be uplifting each other in terms of continuously improving their knowledge and skills. The trainees acknowledged that the absence of such a kind of environment would not foster learning. As one trainee said:
“…in the presence of such an environment I will try to do good not because I have been reprimanded but because I am inspired by my co-trainees.”
(IM-2)
The residents conveyed that their departments must make an effort to create an atmosphere that promotes excellence and maintain an unmistakable uplifting standard which would push the residents to aspire to work hard. Also, an environment where residents feel there is ‘respect for everyone’ fosters motivation among the trainees to study more and perform well.
IV. DISCUSSION
This study explored, through the experiences of resident trainees, how assessment influenced their motivation to accumulate knowledge and skills and attain the competence levels expected of a specialist. We limited our study to the general perception of the residents with regard assessment and how it impacted their learning and not into the specific aspects of their clinical performance. Our results showed that assessment in general positively affected the residents as they were conscious of their actions, and they were inclined to study more.
Our results also revealed there are factors we considered as the catalyst, indirectly related to the assessment process that influenced their desire to learn and improve clinical performance.
There are two messages from this study. Firstly, it was clear there is no single assessment factor that promoted learning. An interplay of several elements within an assessment process ultimately promoted learning – these were patients the residents encounter and concern for their welfare, engagement with the consultants and a supportive environment. The subtleties among these factors and how they interacted with the residents are critical in promoting learning of the residents. Secondly, it is noteworthy to mention that our findings suggest of a considerable degree of self-directed learning (SDL) among the residents who participated in our study, even in the absence of a formal structure on SDL within the departments. Although used interchangeably SDL and self-regulated learning (SRL) are different. SDL refers to the general approach a learner adopts for his own learning whereas SRL is focused on the important learning processes (Gandomkar & Sandars, 2018). In our study, a trainee’s desire to be a good specialist is a reason that was a predominant motivation, which was a key driver of SDL. In the process through SRL, the trainees utilise several cognitive and metacognitive processes to guarantee that the intended learning is met (Gandomkar & Sandars, 2018). The phrase “the self is a bigger motivation to study” from one of the participants, typified the aspiration of the residents to reach another level in their medical education.
Several studies have cited patient care and implicitly patient’s outcome as a vital influence on how residents learn. Nothnagle, Anandarajah, Goldman and Reis (2011) in a study reported that residents acknowledged patient care as the strongest incentive for SDL, adding that residents’ engagement to learn was stronger when it was clinically driven. Similarly, the large role patient’s outcome played as a motivator among the residents in this study has been reported elsewhere (Sagasser, Kramer, & van der Vleuten, 2012; Watling, Driessen, van der Vleuten, & Lingard, 2012). Berkhout et al. (2015) emphasised that the clinical environment is characterised by unique features that influence opportunities to self-regulate which include the patients and the interactions with patients. Matsuyama, Nakaya, Okazaki, Leppink and van der Vleuten (2018) reported that rural physicians in Japan were motivated to initiate learning strategies in a self-regulated manner because of the knowledge that they could upgrade health care in a particular community. The above studies are in congruence with our finding that patients create a powerful drive among residents to strive to become a competent physician.
From the perspective of the residents, the consultants were very instrumental in supporting learning and in giving feedback that was acceptable to the trainees, even if it was negative. The residents felt very strongly that sufficient and meaningful interactions with consultants were valuable in fostering learning because of the perceived increased knowledge and experiences of the consultants. Wong (2011) in a study comparing Canadian and Thai residency programs, reported that knowledge and scholarship were given more premium at the Thai program compared to the Canadian program. It can be surmised that it is reflective of a shared cultural value regarding education among Southeast Asian cultures. Additionally, the residents were more inclined to accept a negative assessment to improve themselves from a consultant who was perceived to be committed to the department and the training of the residents than from a consultant who is perceived to have less commitment. This resonated with the conclusion of Watling et al. (2008) where they investigated the perceptions and experiences of residents toward in-training evaluation process, that such a process became meaningful to the residents only when there is engagement between the evaluator and the residents. Holmboe, Ginsburg and Bernabeo (2011) commenting on the short and frequent rotation among clinical faculty in the USA, stress that such a situation makes it hard for trainees to establish a meaningful relationship with the clinical faculty which predisposes to superficial assessment. Steven, Wenger, Boshuizen, Scherpbier and Dornan (2014) in their research involving clerks in clinical workplace, concluded that the willingness of clinical practitioners to interact with students is the main element that influenced their learning and their education can be enhanced further by involving learners more dynamically in what they referred to as the ‘communicative processes’ of the clinical communities. Nothnagle et al. (2011) in their study of residents’ views toward SDL revealed that residents expressed a need for coaching or guidance to maximise their learning. Sagasser et al. (2012) researching among postgraduate trainees conveyed that affirmation from supervisors and mentors were sought by trainees, as well as from their peers. Faculty must be aware they can influence each specific phase of a resident’s learning process especially since residents look up to them to validate the interpretation and construction of meaning based on what the residents experienced (Teunissen et al., 2007).
The learning environment is an important determinant of behaviour of students or trainees, for this reason many instruments have been designed to measure the learning climate in postgraduate settings (Genn, 2001). The departments must be aware they can promote learning or actually discourage it (Boor et al., 2008). Thus, there is a real need to be aware of how the residents perceive their learning environment within their departments or within the hospital. There is now recognition that it is imperative that hospitals include residents’ training as a part of organisational initiatives to enhance quality, safety and value in patient care, in so doing producing a high quality graduate medical training (Weiss, Bagian, & Nasca, 2013). With regard to SRL, there is definite interaction between the personal, behavioural and environmental aspects that govern self-regulation (Zimmerman, 1989). In a review of the published researches on SRL, van Houten-Schat et al. (2018) concluded that the use of SRL is not maximised in the clinical settings and recommends that a deliberate effort to design a learning environment that offers trainees the opportunity to apply their goal setting skills and helps improve their SRL confidence.
Our findings have shown that indeed any assessment method results in an educational response from postgraduate medical trainees. Our residents do complain, however, that consultants have limited interactions with them, yet these consultants are asked to evaluate them. Such complaints could be overcome by the introduction of direct observation of trainees through workplace based assessments (WBA). Being able to accurately observe resident-trainees performing clinical tasks such as history taking and physical examination and in the process deliver applicable feedback is one of the most important aspects of medical training (Norcini & Burch, 2007). Additionally, the opportunity for feedback which is inherent in these workplace assessment methods is equally important to their role in assessment (Norcini, 2010).
A. Strengths and Weaknesses of the Study
We chose IM and paediatrics because they are two departments without surgical skills and the expected competencies between the two are not very different in terms of knowledge and skills. Involving other residents from departments that train their residents to acquire the needed surgical skills may reveal different resident’ perspectives. Our study was done in a training institution with no WBA methods implemented yet, it would be interesting to study how WBA methods would change the perceptions of these residents toward assessment and the impact of the assessment program itself among the residents. Another limitation is that our study involves a single institution, and we are aware that some institutions may have situations which simulate a ‘hidden curriculum’ which changes the response of the trainees and their perceptions to the assessment practices.
V. CONCLUSION
In postgraduate medical education, trainees acknowledge that assessment positively influences their clinical training and performance. However, it is imperative that the following are considered before assessment can be assumed to contribute to the training and clinical performance of trainees, these are credibility, fairness, inter-personal relations between the trainee and the evaluator and commitment of the evaluator. Additionally, assessment drives learning through an interplay of different elements which include the patients and concern for their welfare, interactions with the consultants or supervisors and the learning environment. The residents, despite the absence of formal training or guidance from the clinical faculty, manifested a high degree of SDL to achieve their goals. The contributory effects of patients toward training of residents must be further researched to add more to the motivation of residents, and when better understood this can be applied even in undergraduate medical settings. Training institutions must make an effort to create an environment that stimulates learning and must be conscious of how the learning environment influences their trainees.
Notes on Contributors
Jaime L. Pacifico, MD, is a cardiologist and a faculty in the college of medicine at De La Salle University in the Philippines. He is a PhD student at Maastricht University. His studies are about perceptions of the learning environment in postgraduate medical education.
Julie Anne Villanueva, MD, is an internist in the Philippines.
Sylvia Heeneman, PhD, has a background in biomedical sciences and is currently an educational researcher and PhD supervisor in this field at Maastricht University.
Cees van der Vleuten, PhD, is the scientific director of the School of Health Professions of Maastricht University. He has published widely on medical education, particularly assessment. He supervises PhD students from the same university.
Ethical Approval
This study was approved by the ethical review board of the De La Salle Medical and Health Sciences Institute, Dasmarinas, Cavite, Philippines.
Acknowledgements
The authors wish to thank all the residents who voluntarily participated in this study.
Funding
This is an unfunded study.
Declaration of Interest
The authors declare that they have no competing interests.
References
Berkhout, J. J., Helmich, E., Teunissen, P. W., van den Berg, J. W., van der Vleuten, C. P. M., & Jaarsma, A. D. C. (2015). Exploring the factors influencing clinical students’ self-regulated learning. Medical Education, 49(6), 589-600. https://doi.org/10.1111/medu.12671
Boor, K., Scheele, F., van der Vleuten, C. P. M., Teunissen, P. W., Den Breejen, E. M. E., & Scherpbier, A. J. J. A. (2008). How undergraduate clinical learning climates differ: A multi-method case study. Medical Education, 42(10), 1029-1036. https://doi.org/10.1111/j.1365-2923.2008.03149.x
Charmaz, K. (2014). Constructing grounded theory. Thousand Oaks, CA: Sage Publications.
Dijksterhuis, M. G. K., Schuwirth, L. W. T., Braat, D. D. M., Teunissen, P. W., & Scheele, F. (2013). A qualitative study on trainees’ and supervisors’ perceptions of assessment for learning in postgraduate medical education. Medical Teacher, 35(8), e1396-e1402.
https://doi.org/10.3109/0142159X.2012.756576
Gandomkar, R., & Sandars, J. (2018). Clearing the confusion about self-directed learning and self-regulated learning. Medical Teacher, 40(8), 862-863.
https://doi.org/10.1080/0142159X.2018.1425382
Genn, J. M. (2001). AMEE Medical Education Guide No. 23 (Part 2): Curriculum, environment, climate, quality and change in medical education – A unifying perspective. Medical Teacher, 23(5), 445-454.
https://doi.org/10.1080/01421590120075661
Glaser, B., & Strauss, A. (1967). The discovery of grounded theory: Strategies for qualitative research. Chicago, IL: Aldine Transaction.
Holmboe, E., Ginsburg, S., & Bernabeo, E. (2011). The rotational approach to medical education: Time to confront our assumptions? Medical Education, 45(1), 69-80. https://doi.org/10.1111/j.1365-2923.2010.03847.x
Holmboe, E. S., Durning, S. J., & Hawkins, R. E. (2018). Practical guide to the evaluation of clinical competence. Philadelphia, PA: Elsevier Health Sciences.
Holmboe, E. S., Hawkins, R. E., & Huot, S. J. (2004). Effects of training in direct observation of medical resident’s clinical competence: A randomized trial. Annals of Internal Medicine, 140(11), 874-881. https://doi.org/10.7326/0003-4819-140-11-200406010-00008
Leung, S. F., Mok, E., & Wong, D. (2008). The impact of assessment methods on the learning of nursing students. Nurse Education Today, 28(6), 711-719.
Matsuyama, Y., Nakaya, M., Okazaki, H., Leppink, J., & van der Vleuten, C. (2018). Contextual attributes promote or hinder self-regulated learning: A qualitative study contrasting rural physicians with undergraduate learners in Japan. Medical Teacher, 40(3), 285-295.
https://doi.org/10.1080/0142159X.2017.1406074
McLachlan, J. (2006). The relationship between assessment and learning. Medical Education, 40(8), 716-717. https://doi.org/10.1111/j.1365-2929.2006.02518.x
Morse, J. M. (1995). The significance of saturation. Qualitative Health Research, 5(2), 147-149.
https://doi.org/10.1177/104973239500500201
Newble, D. I., & Jaeger, K. (1983). The effect of assessments and examinations on the learning of medical students. Medical Education, 17(3), 165-171. https://doi.org/10.1111/j.1365-2923.1983.tb00657.x
Norcini, J. J. (2010). Workplace assessment. In T. Swanwick (Ed.), Understanding medical education: Evidence, theory and practice (pp. 232-245). London, England: Wiley-Blackwell. https://doi.org/10.1002/9781118472361.ch20
Norcini, J. J., & Burch, V. (2007). Workplace-based assessment as an educational tool: AMEE Guide No. 31. Medical Teacher, 29(9-10), 855-871.
https://doi.org/10.1080/01421590701775453
Norcini, J. J., & McKinley, D. W. (2007). Assessment methods in medical education. Teaching and Teacher Education, 23(3), 239-250. https://doi.org/10.1016/j.tate.2006.12.021
Nothnagle, M., Anandarajah, G., Goldman, R. E., & Reis, S. (2011). Struggling to be self-directed: Residents’ paradoxical beliefs about learning. Academic Medicine, 86(12), 1539-1544. https://doi.org/10.1097/ACM.0b013e3182359476
Sagasser, M. H., Kramer, A. W., & van der Vleuten, C. P. (2012). How do postgraduate GP trainees regulate their learning and what helps and hinders them? A qualitative study. BMC Medical Education, 12(1), 67.
https://doi.org/10.1186/1472-6920-12-67
Sambell, K., McDowell, L., & Brown, S. (1997). “But is it fair?”: An exploratory study of student perceptions of the consequential validity of assessment. Studies in Educational Evaluation, 23(4), 349-371.
Schuwirth, W. T., & van der Vleuten, C. P. M. (2010). How to design a useful test: The principles of assessment. In T. Swanwick (Ed). Understanding medical education: Evidence, theory and practice (pp.195-207). London, England: Wiley-Blackwell.
Segers, M., Nijhuis, J., & Gijselaers, W. (2006). Redesigning a learning and assessment environment: The influence on students’ perceptions of assessment demands and their learning strategies. Studies in Educational Evaluation, 32, (3), 223-242. https://doi.org/10.1016/j.stueduc.2006.08.004
Steven, K., Wenger, E., Boshuizen, H., Scherpbier, A., & Dornan, T. (2014). How clerkship students learn from real patients in practice settings. Academic Medicine, 89(3), 469-476. https://doi.org/10.1097/ACM.0000000000000129
Struyven, K., Dochy, F., & Janssens, S. (2005). Students’ perceptions about evaluation and assessment in higher education: A review. Assessment & Evaluation in Higher Education, 30(4), 331-347.
https://doi.org/10.1080/02602930500099102
Teunissen, P. W., Scheele, F., Scherpbier, A. J. J. A., van der Vleuten, C. P. M., Boor, K., Van Luijk, S. J., & van Diemen-Steenvoorde, J. A. A. M. (2007). How residents learn: Qualitative evidence for the pivotal role of clinical activities. Medical Education, 41(8), 763-770.
https://doi.org/10.1111/j.1365-2923.2007.02778.x
Tiwari, A., Lam, D., Yuen, K. H., Chan, R., Fung, T., & Chan, S. (2005). Student learning in clinical nursing education: Perceptions of the relationship between assessment and learning. Nurse Education Today, 25(4), 299-308. https://doi.org/10.1016/j.nedt.2005.01.013
van der Vleuten, C. P. M. (1996). The assessment of professional competence: Developments, research and practical implications. Advances in Health Sciences Education, 1(1), 41-67. https://doi.org/10.1007/BF00596229
van der Vleuten, C. P. M., Schuwirth, L. W. T., Scheele, F., Driessen, E. W., & Hodges, B. (2010). The assessment of professional competence: Building blocks for theory development. Best practice and research clinical obstetrics and gynaecology, 24(6), 703-719.
https://doi.org/10.1016/j.bpobgyn.2010.04.001
van Houten-Schat, M., Berkhout, J., van Dijk, N., Enderdijk, M., Jaarsma, D., & Diemers, A. (2018). Self-regulated learning in the clinical context: A systematic review. Medical Education, 52(10), 1008-1015.
https://doi.org/10.1111/medu.13615
Watling, C., Driessen, E., van der Vleuten, C. P. M., & Lingard, L. (2012). Learning from clinical work: The roles of learning cues and credibility judgements. Medical Education, 46(2), 192-200. https://doi.org/10.1111/j.1365-2923.2011.04126
Watling, C. J., Kenyon, C. F., Zibrowski, E. M., Schulz, V., Goldszmidt, M. A., Singh, I., … Lingard, L. (2008). Rules of engagement: Residents’ perceptions of the in-training evaluation process. Academic Medicine, 83(10), S97-S100. https://doi.org/10.1097/ACM.0b013e318183e78c
Watling, C. J., & Lingard, L. (2012). Grounded theory in medical education research: AMEE Guide No. 70. Medical Teacher, 34(10), 850-861.
https://doi.org/10.3109/0142159X.2012.704439
Weiss, K. B., Bagian, J. P., & Nasca, T. J. (2013). The clinical learning environment: The foundation of graduate medical education. JAMA, 309(16), 1687-1688.
https://doi.org/10.1001/jama.2013.1931
Wong, A. K. (2011). Culture in medical education: Comparing a Thai and a Canadian residency programme. Medical Education, 45(12), 1209-1219.
https://doi.org/10.1111/j.1365-2923.2011.04059.x
Zimmerman, B. J. (1989). A social cognitive view of self-regulated academic learning. Journal of Educational Psychology, 81(3), 329-339.
http://dx.doi.org/10.1037/0022-0663.81.3.329
*Jaime L. Pacifico
De La Salle University College of Medicine,
De La Salle Medical and Health Sciences Institute,
Dasmarinas, Cavite, Philippines
Tel: +63 46 481 8000
E-mail: jlpacifico@dlshsi.edu.ph
Published online: 7 January, TAPS 2020, 5(1), 25-45
DOI: https://doi.org/10.29060/TAPS.2020-5-1/OA2073
Margaret Tan1, Jonathan S. Herberg1, Celestial Yap2,3, Dujeepa D. Samarasekera4 & Zhi Xiong Chen2,3,4,5,6
1Institute of High Performance Computing, Agency for Science, Technology and Research (A*STAR), Singapore; 2Department of Physiology, Yong Loo Lin School of Medicine, National University of Singapore, Singapore; 3National University Cancer Institute, National University Health System, Singapore; 4Centre for Medical Education, Yong Loo Lin School of Medicine, National University of Singapore; 5KK Women’s and Children’s Hospital, Singapore; 6Office of Student Affairs, National University of Singapore
Abstract
Given the high investments in training and mentoring graduates who have chosen the research career path, and considering a high attrition of these graduates moving on to non-research type of careers, it is important to understand the factors that motivate young scientists to stay on the job as they could make important contributions to a better world with their scientific endeavours. It is in this context that we conducted an exploratory study to understand the factors that may drive the scientists’ performance as well as their expectations to remain in the research career paths. We found evidence for an indirect link (through research commitment) between need-for-cognition and career performance as well as evidence of an effect of research commitment on the anticipated research career length. There was also evidence that continuance commitment (but not other extrinsic factors) affects anticipated research career length, and that organisational support is linked to perceived research performance. Implications of our findings for student selection and graduate mentoring are discussed.
Keywords: Research Career Path, Scientist’s Motivation, Graduate Mentoring, Intrinsic and Extrinsic Motivations
Practice Highlights
- Research commitment and organisational support are predictors of perceived research performance.
- Research commitment and continuance commitment are predictors of anticipated research career length.
- Develop intellectually stimulating curriculum and work tasks to promote research motivation and innovations.
- Develop holistic curriculum to include knowledge management and domain expertise in graduate education.
- Encourage STEM employers to create more attractive careers and conducive workplace culture and conditions.
I. INTRODUCTION
Building a scientist’s expert domain knowledge is a long-term investment. Many years of education guidance and training are required to nurture each scientist to be competent in the field of expertise. Although the bachelor’s degree is often the stepping-stone in building a Science, Technology, Engineering and Mathematics (STEM) career, more advanced skills and specialised know-how developed during Masters and PhD programs are often required in order for a scientist to progress. Beyond PhD studies, a researcher aspiring to be independent requires further exposure to the scientific environment through postdoctoral fellowships. During this period, supervisors play an important role in the education and training of these young scientists, guiding, mentoring and nurturing them to be innovative in developing research that is of relevance to the world. In addition to research experience, the scientist needs pragmatic skills such as resource management. Yet, globally, young scientists including the best and the brightest, are leaving research careers for other non-research related careers independent of job competition, availability of funding and number of publications (Callaway, 2014; Roach & Sauermann, 2017).
In the early 2000s, when Singapore identified life sciences as the next pillar of economic growth, the government forged ahead to develop this sector, and one of the ways was for the university to become part of the ‘university-government-industry’ trinity to train and prepare the country’s limited human resource for this important sector. Considering that national policies and institutions are obliged to provide long-term and extensive investments to nurture these graduates in order for them to produce research innovations, attract investments, and stimulate economic and intellectual growth, there is an urgent need to understand why increasing number of promising STEM postgraduates opt to leave their scientific career paths to pursue non-research related careers that are not aligned to their prior education and training.
While the reasons for leaving STEM research careers could be due to changing job preferences because of self-perceived inability to do research, and misalignment in the expectation and reality of what research has to offer, the factors for this self-perceived research performance and misalignment in expectation and reality of research careers remain unknown. Therefore, this study aims to investigate and understand the factors that may influence the graduates’ perceived research performance and anticipated career longevity in scientific research paths. Identifying the factors that lead to the attrition of the STEM workforce will help educational institutions to refine or enhance graduate programs. The findings will also help educational leadership to understand the unmet needs and socio-psychological perceptions of the research scientists, and to address the intrinsic (personalised) and extrinsic (environmental/ organisational) factors which may motivate them to persevere towards successful careers in scientific research.
A. Conceptual Framework
Review of the literature suggests that a scientist’s research career performance and longevity may be rooted in specific motivational tendencies and can be driven by perspectives supported by the organisational culture and environment. It is in this context that the study investigates the factors that determine the scientist’s research career path longevity. We propose a conceptual framework as shown in Figure 1 that takes into account the individual traits such as the need-for-cognition, need-for-closure, and intrinsic motivation in identifying career performance. The two constructs, the need-for-cognition and need-for-closure, are integral to one’s knowledge-seeking motivation, and they are both linked to driving intrinsic motivation that has a direct effect on perceived research performance, which in turn affects the scientist’s choice to remain in the research career. However, we also propose that the commitment to remain in a research career over the long term is moderated by extrinsic factors such as perceived support in the work environment/organisation, supervisor’s support, and work autonomy. In other words, a graduate’s choice to remain in a research career path is influenced by perceived research performance with extrinsic factors in the work environment moderating the relationship.
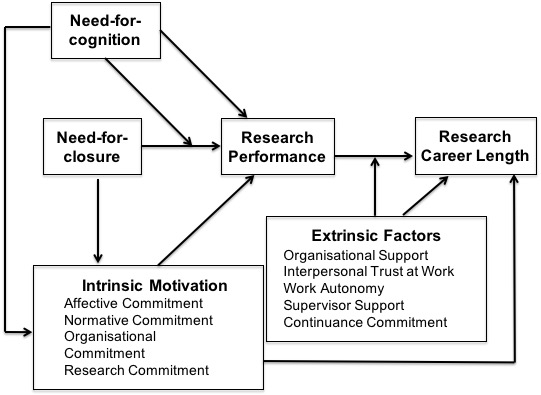
Figure 1. The conceptual framework of cognitive and motivational constructs and their links to perceived research performance and anticipated research career length
Need-for-cognition refers to the extent one gains pleasure from effortful cognitive processing, such as figuring out solutions for difficult puzzles (Cacioppo & Petty, 1982). It has general utility and predictive power in social and educational psychology as a stable personality trait that shapes knowledge-seeking behavioural tendencies across a diverse range of situations (Fortier & Burkell, 2014; Szumowska & Kossowska, 2016, 2017). In our framework, the need-for-cognition is directly linked, as well as indirectly linked, through intrinsic motivation to career performance. As success in a research career path depends on a stable motivation to solve difficult and often long term problems, individuals who have a high need-for-cognition should exhibit better performance through their drive toward pursuing challenging questions out of curiosity. They tend to have a greater inclination to devote time and effort to difficult issues with deep analysis. Further, the need-for-cognition also opens one to new ideas, and facilitates willingness to engage in argument and having differing perspectives (Mussel, 2010). In fact, knowing that accumulating one’s knowledge is based on one’s prior research, the high need-for-cognition not only contribute to better performance but it should also influence long term career.
Need-for-closure refers to one’s need to obtain clear-cut answers to questions. Depending on situational factors, a higher need-for-closure can entail a greater motivation to seek information in carrying out cognitive tasks, or contrariwise a greater resistance to incorporating new information that challenges answers subjectively seem sufficient for getting tasks done (Roets, Kruglanski, Kossowska, Pierro, & Hong, 2015). For instance, if early cues suggest a feasible solution to a problem, a higher need-for-closure can result in a greater resistance to assimilating new information that may later challenge the earlier solution. On the other hand, a higher need-for-cognition can help spur an individual to seek new knowledge when significant uncertainties are made apparent. Thus, an individual’s need-for-cognition is a source for a variety of impacts on one’s motivation to seek and incorporate new knowledge; as such it is important to specify its roles in the context of determining a scientist’s research path and longevity.
The need-for-closure could be viewed as specifying a form of motivated cognition, leading to different goals depending on circumstances, rather than specifying a general lack of motivation for cognitive processing (Kruglanski et al., 2012; Kruglanski & Webster, 1996). In situations of high ambiguity and significant knowledge gaps, such as might be present at the start of a research endeavour, one’s need-for-closure can trigger significant devotions of cognitive effort toward obtaining clear answers. On the other hand, when seemingly satisfactory answers are obtained, a higher need-for-closure can entail goals to avoid acknowledging subsequent conflicting evidence and ambiguities requiring additional research. Hence, we propose that the link between need-for-closure and career performance may be moderated by need-for-cognition. This reflects the idea that different psychological motivations and capacities can interact to influence behavioural tendencies (Fortier & Burkell, 2014; Hill, Foster, Sofko, Elliot, & Shelton, 2016; Szumowska & Kossowska, 2016, 2017). For instance, if one’s need-for-cognition is low, a higher need-for-closure may only weakly improve, or even detract from perceived research performance, as one may have a tendency to crystalise knowledge too early in the research process, and be resistant to modifying knowledge based on follow-up research. Experimental evidence supports the notion that individuals with a higher need-for-closure have a higher tendency to “seize” early information cues in cognitive decision tasks, and to “freeze” the knowledge thereby acquired, being less prone to modify knowledge from subsequent information cues (Roets et al., 2015). It is possible that a high need-for-cognition can counteract the knowledge “freezing” tendency in high need-for-closure individuals, thereby sustaining their motivation for further knowledge-seeking behaviours following initial knowledge formation. This is consistent with the finding that individuals high in both needs tend to engage most predominately in information-seeking behaviours indicative of intellectual openness (Fortier & Burkell, 2014; Szumowska & Kossowska, 2016, 2017), which we propose as a key component for successful research careers.
Intrinsic motivation is an essential construct for understanding performance and choice to stay in the career. Motivation generally refers to an individual’s inclination to devote effort toward goals; however, intrinsic motivation arises from one’s desire for self-improvement and genuine interest, rather than from external pressures (Koestner & Losier, 2002). For intrinsic motivation to be maintained, one’s needs for autonomy (sense of self-control), competence (sense of capability) and relatedness (sense of social connectedness and purpose) have to be obtained while one engages in effortful activities toward achieving long-term goals (Ryan & Deci, 2000). Empirical research supports the notion that intrinsic motivation, as compared to more extrinsic forms of motivation, is critical for long-term academic performance (Taylor et al., 2014). In our model, intrinsic motivation has a direct link not only to performance, but also to long-term career choice, i.e. the likelihood of choosing to stay on a given research career path over an extended period of time, rather than changing careers. Thus, we propose the importance of intrinsic motivation in driving career performance and choice to remain in it.
Extrinsic factors include organisational culture and structure that support the work environment comprising such components as i) perceived support and value (conveyed by the organisation; Lambert, 2000); ii) interpersonal trust at work (Cook & Wall, 1980); iii) work autonomy, which includes approach to perform the tasks (or the degree of choice one has in determining the means and plans for completing the tasks), and scheduling autonomy (or how much flexibility one has in the timing of completion of tasks and goals; Breaugh, 1985, 1999) and iv) supervisor support. For research work, a mentor relationship is important to generate interpersonal trust and confidence. By mentor relationships, we refer to the degree of research guidance, coaching, and support that the scientist receives from his or her mentors. Better mentor relationships can lead to an increased motivation to maintain one’s career as a research scientist, in addition to sustaining increased performance. Further, extrinsic motivation also involves one’s continuance commitment referring to one’s inclination to remain in a given job for practical considerations; hence we propose that while better perceived research performance tends to increase anticipated research career length, the strength of this link is moderated by extrinsic factors.
II. METHODS
Ethical approval was obtained from the Institutional Review Board, National University of Singapore (NUS) to conduct the survey questionnaire investigation. Participants completed an online questionnaire (hosted on SurveyMonkey) that took about 45 minutes to complete. The online survey was conducted over a period of nine months.
A. Participants
The target respondents consisted of the STEM postgraduate students and PhD fellows. The administrative staff independent of the investigators sent out individual emails to each of the following departments and faculties to seek their approval to disseminate the survey – NUS Yong Loo Lin School of Medicine (12 Heads of Department, Vice-Dean [Research], Assistant Dean [Research] and Vice-Dean [Academic Medicine]), Faculty of Arts and Social Sciences (Vice-Dean, Research), Faculty of Engineering (Vice-Dean, Research), Faculty of Science (Vice-Dean) and NUS Graduate School (Executive Director). Once approval was obtained, their secretaries were requested to send an email invitation containing the survey link to each of their respective postgraduate students and PhD fellows to participate in the survey.
Participants were given three weeks to complete the questionnaire. Reminder emails were sent to the participants to complete the survey if they had not done so. 92 participants took part in the survey. Among the 63 participants who provided their demographic details, 32 were male and 31 were female. The ages ranged from 21 to 44 years old, with the majority between 25 to 34 years old. On average, they had about 2 to 6 years of research experience. Majority respondents came from Biomedical & Related Sciences (44), with the rest as follows: Engineering & Technology (6), Natural Sciences (excluding Biological Sciences; 4), Social Sciences (3), Agriculture & Food Sciences (2), Biological Sciences (2), Healthcare & Related Sciences (1) and Healthcare Services (1). We used responses from 64 participants for the regression and path analyses on anticipated research career length.
B. Questionnaire Design
We developed a survey instrument measuring various constructs of the model by adapting validated questionnaires established in the industrial organisation and cognitive psychology literature. The questionnaire consists of four parts as follows – i) 64 closed-ended questions on a 6-point Likert scale, ii) 10 closed-ended questions, iii) 2 ranking questions, and iv) a demographic section. For all scale questions, participants indicate their responses on a six-point Likert scale by indicating whether they “Strongly Disagree”, “Disagree”, “Slightly Disagree”, “Slightly Agree”, “Agree”, or “Strongly Agree”. For each construct, a participant’s agreement ratings across the construct’s items were averaged (with negatively framed items reverse-coded), to obtain an overall rating for the construct. The appendix shows the questions that we used for the various constructs.
To assess Need-for-Cognition, we utilised eight items from the Cacciopo et al. validated for the need-for-cognition scale (Cacioppo & Petty, 1982). Need-for-Closure was also assessed by eight validated items as well (Roets & Van Hiel, 2011). Organisational Commitment was measured directly through participants’ ratings of items from the established Cook & Wall scale (Cook & Wall, 1980), as well as items assessing their Affective Commitment (in relation to their organisation) and their Normative Commitment (to remain in their organisation; Allen & Meyer, 1990), as these latter sets of items pertain to their motivation to remain in their current education or work environment. As a distinct component of Intrinsic Motivation, we included five items measuring the participant’s Research Commitment. These items are likely to most directly reflect intrinsic motivation, as they were adapted from the validated Intrinsic Motivation Inventory (Ryan & Deci, 2000), and contextualised with the aim to assess directly participants’ intrinsic motivation for engaging in research tasks in relation to their work or education. Next, our main Extrinsic Factors component, Organisational Support was measured from the validated Lambert et al. scale (Lambert, 2000) which directly assesses the degree of support participants perceive to come from their organisational environment. In addition, we included other organisational-related subscales, which we propose to reflect extrinsic factors in relation to one’s research career. These consist of items assessing participant’s Supervisor Support, Interpersonal Trust at Work, and Work Autonomy granted by the organisation (Breaugh, 1999; Cook & Wall, 1980). Lastly, as an extrinsic factor distinct from organisational factors, we included items to measure participants’ Continuance Commitment, or the degree to which they are motivated to remain in their work environment for extrinsic rather than intrinsic reasons (Allen & Meyer, 1990).
To assess participants’ perceived research performance, we had five questions, which we intended to indicate how strongly they viewed their level of performance (and their co-workers’ view of their performance). In addition, participants indicated their expected research career length in terms of choosing one of five responses, ranging from “less than 2 years” to “more than 10 years”, which we coded on a five-point ordinal scale. In addition, we had questions designed to elicit direct feedback from participants regarding their motivations, expectations, and experiences in their work or education environment.
III. RESULTS
Through our 10 closed-ended questionnaires on the participants’ research and career aspiration, the descriptive statistics showed some 84.5% of the participants were motivated to pursue a STEM career as indicated by their early passion or participation in science and research (Question 5). In fact, some 95.3% started to think about attending graduate school even before or during their undergraduate years (Question 6). However, despite their early enthusiasm to pursue a science and research career, it is discouraging that 54.7% intended to continue research in an academic or research setting (Question 7), and worse only 25% see themselves working in research and development beyond 10 years after their PhD (Question 9). Thus, it is not surprising that 23.4% were unlikely/very unlikely to take up non-academia/non-research careers after PhD (Question 8) and for those who were likely/very likely to take up non-academia/non-research careers, they included careers in banking and finance, management and consulting, and corporate positions in biotech and pharmaceutical firms (Question 10). It appeared that remuneration is an important deciding factor (68.8% cited it) whether or not to stay in research (Question 11); indeed, they also want increases in their current salary (Question 13). The findings also showed that the top two factors influencing participants’ decision to stay or leave a research and development career are physical work environment (e.g. equipment, ergonomics, cleanliness – Question 15) and working conditions (e.g. organisation culture – Question 16). In terms of the descriptive statistics, it is a concern to note that participants see the unattractiveness to pursue a scientific research career despite early strong motivation, prior to graduate studies.
Furthering our investigations using the closed-ended questionnaires, we analysed the relationship between our scale-construct metrics and a) participants’ self-rated research career performance (as reflected in the mean of the five questions at the end of Part D of the survey; and b) participants’ expected research career length, as reflected in their responses (coded as 1 to 5) to the question “How long do you see yourself working in research and development after your PhD?” To address these latter questions, we applied multiple regression analyses and path analyses. Multiple regression analyses were applied for each of our two dependent variables (the metric of self-rated research performance, and of anticipated research career length). For each dependent variable, a stepwise regression was calculated with all the subscale scores initially entered as separate predictors, and with the Akaike Information Criteria (AIC) utilised to select which subscale predictors to keep in the final stepwise model. In addition, for predicting perceived research performance, which was a mean rating across several items, we applied linear multiple regression models, but for predicting anticipated research career length, comprising a single item rating for each participant, we applied ordinal logistic regressions, to avoid in the latter case the more questionable approximation of treating a single-item rating as though it were on an interval scale.
For a more direct test of the proposed links in our conceptual framework, we developed two path analysis models. First, to examine the loadings of the intrinsic motivation and the extrinsic factors constructs on their respective subscale scores, we conducted a confirmatory factor analysis. The indicators for the intrinsic motivation construct were taken as its subscale scores (affective commitment, normative commitment, organisational commitment, and research commitment). The manifest indicators for the extrinsic motivation construct were the scores on the subscales for organisational support, interpersonal trust at work, supervisor support, work autonomy, and continuance commitment. The fit statistics for this factor analysis was adequate: Confirmatory Fit Index (CFI) = 0.91; Root Mean Square Error of Approximation (RMSEA) = 0.08; c2 = 36.60, df = 26, p = 0.08. However, the standardised loadings for affective commitment (.09) and for continuance commitment (.13) were not statistically significant. Therefore, in our initial structural equation model (SEM), we dropped these indicators. The endogenous variable of anticipated research career length was treated as ordinal, with weighted least square mean and variance adjusted estimation applied. This SEM however had poor model fit statistics: CFI = 0.56; RMSEA = 0.23; c2 = 412, df = 95, p < 0.01. These fit statistics were improved when a link between Extrinsic Factors and perceived Research Performance was included (rather than, as with our original conceptual model, only having only the link between Extrinsic Factors and Anticipated Research Career Length included): CFI = 0.66; RMSEA = 0.20; c2 = 333, df = 94, p < 0.01. However, as these statistics are still far from adequate overall model fit, we settled on a simplified, single-indicator path analysis approach. Intrinsic motivation was represented by the Research Commitment subscale score, as this subscale was most directly relevant in being based on the validated Intrinsic Motivation Inventory, and in the final stepwise model utilising the subscale scores as predictors for perceived Research Performance since Research Commitment and Organisational Support were the only significant subscale predictors. For the regression analysis predicting Anticipated Research Career Length, in the final stepwise model Research Commitment and Continuance Commitment were the only significant predictors. Based on these considerations, we implemented two single-indicator path analysis models. Both utilised Research Commitment as the indicator for Intrinsic Motivation. For the Extrinsic Factors indicator, our first path analysis model utilised Organisational Support, whereas our second one utilised Continuance Commitment. The fit statistics for our first path analysis are substantially improved over the more complicated SEMs: CFI = 0.91; RMSEA = 0.12; c2 = 13.0, df = 7, p = 0.07. For our second path analysis, the fit statistics were very strong: CFI = 1.00; RMSEA = 0.00; c2 = 5.01, df = 7, p = 0.66. Thus, for the purpose of exploring potentially important causal links among critical variables, our final path analysis models both include one link that was not in our conceptual framework, which is the link between “extrinsic factors” and perceived “research performance”. They also focus specifically on the research commitment component of intrinsic motivation, and (separately) on the organisational support and on the continuance commitment components of extrinsic factors.
Our results showed that the research commitment component of intrinsic motivation may be the driver in influencing perceived research performance (as it is significant in both the final model output; Table 1, Figures 2 and 3). Organisational support component of extrinsic factors, on the other hand, seems to impact perceived research performance, and is the only significant extrinsic factors subscale in the stepwise regression for predicting perceived research performance (Table 1 and Figure 2). Table 1 shows the final AIC stepwise model, for the intrinsic and extrinsic subscales that affect career performance.
| Predictor | β | t | p |
| Research Commitment | .43 | 4.78 | <.01** |
| Organisational Commitment | .17 | 1.66 | .10 |
| Organisational Support | .21 | 2.15 | .04* |
| Supervisor Support | .19 | 1.85 | .07 |
Note: Standardised coefficients, t-statistics, and p-values for final model in AIC stepwise regression for predicting perceived research performance (with intrinsic motivation and extrinsic factors broken down into subscales).
Adjusted R2 = .54, F(4,66) = 21.68, p < .01
*p < .05, **p < .01
Table 1. Stepwise regression results for perceived research performance with construct subscales
Focusing on the paths in Figure 2 that lead to perceived research performance (in the path analysis with organisational support as the extrinsic factor indicator), we found that the direct link from need-for-cognition is non-significant, whereas that from research commitment is significant. In addition, the indirect link between need-for-cognition and perceived research performance, through research commitment, is statistically significant (β = 0.17, p < .05). Also, the link between organisational support and perceived research performance is significant. Lastly, need-for-closure has no direct or indirect effect on perceived research performance, and there is no interaction effect of need-for-cognition on need-for-closure to influence perceived research performance. In addition, in our path analysis that includes continuance commitment as the extrinsic factor indicator, there is no effect of continuance commitment component on perceived research performance (Figure 3).
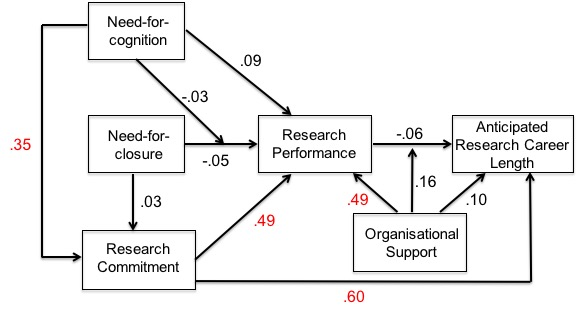
Note: The research commitment subscale represents intrinsic motivation, and the organisational support subscale represents extrinsic factors. Links are labelled with standardised coefficients. Coefficients in red are statistically significant.
Figure 2. Path analysis of the conceptual framework (research commitment and organisational support)
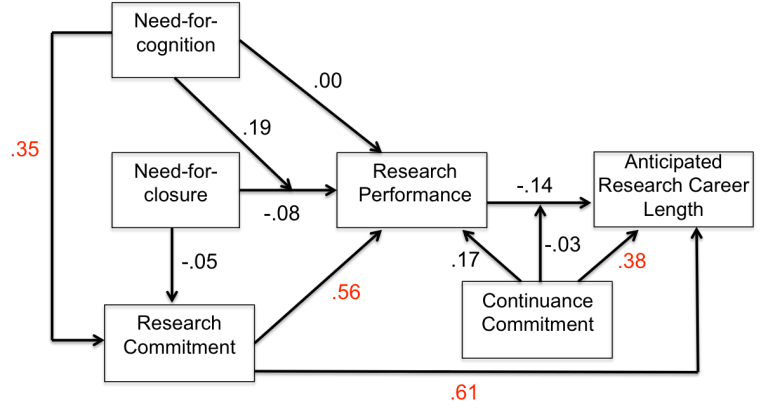
Note: The research commitment subscale of intrinsic motivation and the continuance commitment subscale of extrinsic factors are the only subscales with significant beta coefficients. Links are labelled with standardised coefficients. Coefficients in red are statistically significant.
Figure 3. Path analysis of the conceptual framework (research commitment and continuance commitment)
Thus, perceived research performance may be significantly predicted by research commitment, i.e. items assessing intrinsic motivation for research. Furthermore, need-for-cognition may indirectly affect perceived research performance, by influencing research commitment. Organisational support may, in addition, be an important predictor of perceived research performance. In other words, scientists with high need-for-cognition, high intrinsic motivation coupled with strong positive extrinsic factors may perform better in research, which we proposed might increase the likelihood of them staying on in research careers. However, satisfying their need-for-closure may not necessarily enhance their perceived research performance, or lead them to remain in STEM careers.
| Predictor | β | t | p |
| Research Commitment | 1.32 | 4.51 | <.01** |
| Interpersonal Trust | -.43 | -1.58 | .11 |
| Continuance Commitment | .64 | 2.47 | .01* |
Note: Standardised coefficients, t-statistics, and p-values for final model in AIC stepwise ordered logistic regression for predicting anticipated research career length (with intrinsic motivation and extrinsic factors broken down into subscales).
*p < .05, **p < .01
Table 2. Stepwise regression results for anticipated research career length with construct subscales
Our stepwise ordinal logistic regression analysis for predicting anticipated research career length that included the individual subscales for intrinsic motivation and for the extrinsic factors scale suggests that research commitment (within intrinsic motivation) and continuance commitment (within extrinsic factors) may be important, as they are the only statistically significant predictors in the final stepwise model (Table 2).
From our path analysis of predictors that affect anticipated research career length, with organisational support as the extrinsic factors indicator, we found no effect from perceived research performance, from organisational support, or from the organisational support by perceived research performance interaction. The only direct link to anticipated career length comes from research commitment (Figure 2). However, the indirect effect of need-for-cognition, through research commitment, is in the marginal area of statistical significance (β = 0.21, p = .06). In our path analysis that includes continuance commitment as the extrinsic factors indicator, we found a statistically significant effect of continuance commitment on anticipated research career length (Figure 3).
IV. DISCUSSION
We believe that this is the first study in Singapore to investigate the factors to determine perceived research performance and anticipated career longevity of scientists in the STEM environment. We envisaged that graduates who are inclined towards and enjoy effortful cognitive activities are likely to do well in research activities. The findings of the study, however, suggest that future education as well as career policies concerning graduate students’ recruitment may need to focus on identifying individuals who demonstrate their psychological cognitive trait in pursuing investigative and creative research. In a similar context, academic chairs of graduate schools and institutions should be mindful of designing programs that are geared towards enhancing and sustaining the researchers’ cognitive and motivational aspirations.
It is not surprising to note that individuals, who are intrinsically motivated or having stronger commitment to do research are likely to perceive themselves to perform better, but only when organisational support and environment are favourable and conducive. In this context, it appears that programs for training and nurturing graduate students need to focus not only on providing domain knowledge competence but to also understand researchers’ aspirations and life purposes, and expressed by participants, they can be as diverse as the need to “provide for family”, to pursue “personal achievement” or be a “stepping stone in academia”. Given that organisational culture, supervisory support and their interdependency have been shown to be important in how employees perceive their value to the organisation and reciprocate in kind, our lack of significant correlations could be due to the limitation of the small sample size as our study only obtained about 10 to 20 percent response rate (92 out of estimated 500 to 1000 participants reached) and with only 64 completed usable responses compared to higher response rates and completed usable responses in other studies (Shoss, Eisenberger, Restubog, & Zagenczyk, 2013).
In terms of anticipated career longevity, there is no single factor that is able to predict an individual’s likelihood to choose and embark on a long-term research career trajectory. What is striking is that perceived research performance is unable to predict for anticipated career longevity. This suggests that even if an individual performs well in research, there is no certainty that he or she may continue to pursue research as a long-term career. Indeed, our finding confirms previous work showing that postgraduates may leave the research career path independent of publications and funding (Roach & Sauermann, 2017). However, there is evidence to suggest that individual elements of particular factors may be indicative for anticipated career longevity. Specifically, individuals who are committed to research and emotionally attached to the institution are more likely to stay on and be committed in research careers. This suggests that it may be beneficial for graduate mentoring programs to incorporate activities that are likely to enhance emotional bonding of students with their institutions, which in turn may increase their affinity towards research careers. It seems that the findings suggest that research commitment or a passion to do research is a key ingredient to perceived performance success and anticipated career longevity.
Understanding the factors that influence commitments to perceived research performance and anticipated career longevity is important to guide the design of scholarship policies to mitigate declining scholarship and increasing attrition among graduate students pursuing the STEM career paths. Currently, training of graduate students mainly involves undertaking a suite of domain-related course modules and embarking on a research project over a specified period of usually 4 years, leading to a thesis. Students are encouraged to publish but often, this is not a mandatory requirement. These students are also required to support and perform teaching duties as one of the program requirements. For early career scientists, the training is less structured where trainees typically spend an undefined amount of time in a research setting working on various projects. Given that “research can be too mentally challenging and stressful” as cited by a participant, it is therefore crucial to have effective, supportive and readily approachable mentors. Supervisors of graduate students and early career scientists are typically universities’ faculty or research institutes’ principal investigators who may not have formal training in mentorship. Currently, in Singapore, there is no systematic training of supervisors on how to supervise and mentor students in a holistic manner. Perhaps, it may be useful to take guidance from best practices for doctoral training in Europe and North America, and contextualise these to local settings and conditions (Barnett, Harris, & Mulvany, 2017).
We would like to suggest that future education and training of graduate students and early career scientists should not only focus on developing programs that build depth and breadth of domain knowledge but they must instil the desire for intellectual contribution to society. Scholarships should enhance the researchers’ intrinsic motivation of their research commitment and help them to appreciate their contributions to their research endeavours. Guidelines should be in place to provide supervisors with the necessary guidance for effective and holistic mentorship, and to shift from an output-oriented mindset to a human development-centric mindset. Although we have no evidence from direct feedback to suggest a link between organisational support and continuance commitment, nevertheless, given that forms of organisational support such as physical work environment and working conditions are the top two factors influencing participants’ decision to stay or leave a scientific research career, this may suggest a potential link between organisational support and continuance commitment. In brief, we believe these changes would alter mentor-mentee behaviour and relationship, creating a conducive and trusting environment with strong organisational and supervisory support for fostering meaningful research that is aligned to each organisation’s goals and objectives.
V. LIMITATIONS
A limitation of this study is that the sample sizes are small, and as the study is a questionnaire survey, only perceived research performance and self-declared expected research career length were used. We acknowledged that research performance could be measured more objectively in terms of number of academic publications and citations, however, our definition of research performance also encompasses subjective aspects which are harder to evaluate such as having an inquisitive mind, taking initiatives to explore innovations, providing ethical scholarly behaviour that includes collaborations. We note that self-declared expected research career length may not reflect reality, and it would have been more realistic to evaluate actual periods that the scientists stayed on in their successful research careers versus those who did not. However, this is logistically challenging to carry out with potentially more confounding variables that are difficult to define.
VI. CONCLUSION
In conclusion, we hope that our findings will provide insights to implore domain curriculum developers and prospective research-oriented employers to incorporate intellectually stimulating learning or work components that will motivate and strengthen research commitment. Indeed, education policymakers should explore areas of support that are lacking in graduate education while policymakers of research institutes should provide making research careers and workplace conditions more conducive and attractive for retaining scientific talents. Indeed, the many issues surrounding STEM career deserve attention and especially in the context that many young scholars who aspire to do research at the onset eventually choose to leave their research careers (Kavallaris et al., 2008). For instance, participants cited that “career stability is very limited” as projects are based on research funding; consequently it has been touted as having weak career development prospects when funding runs out. Researchers also often cited that they are “underpaid in the research field” and “pay for them is very low, relative to other industries”. Hence, having adequate annual leave considering that they tend to work long hours to finish a project, better remuneration that is more comparable to other industries, and greater assurance towards a clearer career roadmap would ensure a more research continuance commitment.
We hope that other researchers would replicate this study to delve deeper into the importance of understanding the cognitive and psychological needs of the researchers, enhancing research commitment in the community and developing strong organisational ties in influencing research performance and commitments as well as longevity in research careers among graduate students and early career scientists.
Notes on Contributors
Dr Margaret Tan, PhD, was a senior scientist at A*STAR prior to setting up SmartWerkz, an AI-driven ontological system that delivers immersive extended reality skills coaching to facilitate effective application of knowledge assets. She was also an Associate Professor at NTU and NUS specialising in knowledge management and organisational behaviours.
Dr Jonathan Herberg, PhD, has worked over five years as a research scientist (cognitive psychologist) at A*STAR IHPC. He obtained his PhD in Psychology from Peabody’s Cognition and Cognitive Neuroscience Program at Vanderbilt University. His research includes experimental and educational psychology, collaborative learning, human-computer interaction, psychometrics and predictive analytics.
A/Prof Celestial Yap, MBBS, PhD, is the Education Director for Health Professions at the Department of Physiology and an Affiliate Associate Professor from the National University Cancer Institute. She is also the Integration Lead Educator in undergraduate medical curriculum. Her research interests include medical education and graduate research training.
Dr Dujeepa D. Samarasekera, MBBS, MHPE, FAMS, FAcadMEd, FAMEE, is the Director of Centre for Medical Education, National University of Singapore and the President of the Western Pacific Regional Association of Medical Education. He also consults for the Singapore Ministry of Health on medical education matters.
Dr Zhi Xiong Chen, PhD, is the Deputy Education Director from the Department of Physiology and the Assistant Dean of Students at NUS. He is also the Integration Lead Educator in undergraduate medical curriculum and a Joint Scientist at KKH. His research interests include health professions education.
Ethical Approval
This research received approval from the NUS-Institutional Review Board (NUS-IRB Ref No. B-15-256). Consent was obtained from participants for the research study.
Acknowledgements
The authors would like to thank Mr Yeo Su Ping for the administrative help rendered throughout the study.
Funding
No funding is involved in this paper.
Declaration of Interest
The authors report no conflict of interest. The authors alone are responsible for the content and writing of the article.
References
Allen, N. J., & Meyer, J. P. (1990). The measurement and antecedents of affective, continuance and normative commitment to the organization. Journal of Occupational and Organisational Psychology, 63(1), 1-18.
https://doi.org/10.1111/j.2044-8325.1990.tb00506.x
Barnett, J. V., Harris, R. A., & Mulvany, M. J. (2017). A comparison of best practices for doctoral training in Europe and North America. FEBS Open Bio, 7(10), 1444-1452. https://doi.org/10.1002/2211-5463.12305
Breaugh, J. A. (1985). The measurement of work autonomy. Human Relations, 38(6), 551-570. https://doi.org/10.1177/001872678503800604
Breaugh, J. A. (1999). Further investigation of the work autonomy scales: Two studies. Journal of Business and Psychology, 13(3), 357-373. https://doi.org/10.1023/A:1022926416628
Cacioppo, J. T., & Petty, R. E. (1982). The need for cognition. Journal of Personality and Social Psychology, 42(1), 116-131. http://dx.doi.org/10.1037/0022-3514.42.1.116
Callaway, E. (2014). Life outside the lab: The ones who got away. Nature, 513(7516), 20-22. http://dx.doi.org/10.1038/513020a
Cook, J., & Wall, T. (1980). New work attitude measures of trust, organizational commitment and personal need non‐fulfilment. Journal of Occupational Psychology, 53(1), 39-52. https://doi.org/10.1111/j.2044-8325.1980.tb00005.x
Fortier, A., & Burkell, J. (2014). Influence of need for cognition and need for cognitive closure on three information behavior orientations. Proceedings of the Association for Information Science and Technology, 51(1), 1-8. https://doi.org/10.1002/meet.2014.14505101066
Hill, B. D., Foster, J. D., Sofko, C., Elliot, E. M., & Shelton, J. T. (2016). The interaction of ability and motivation: Average working memory is required for need for cognition to positively benefit intelligence and the effect increases with ability. Personality and Individual Differences, 98, 225-228. https://doi.org/10.1016/j.paid.2016.04.043
Kavallaris, M., Meachem, S. J., Hulett, M. D., West, C. M., Pitt, R. E., Chesters, J. J., . . . Khachigian, L. M. (2008). Perceptions in health and medical research careers: the Australian Society for Medical Research Workforce Survey. Medical Journal of Australia, 188(9), 520-524.
https://doi.org/10.5694/j.1326-5377.2008.tb01766.x
Koestner, R., & Losier, G. F. (2002). Distinguishing three ways of being highly motivated: A closer look at introjection, identification, and intrinsic motivation. In E. L. Deci & R. M. Ryan (Eds.), Handbook of self-determination research (pp. 101-121). Rochester, NY: University of Rochester Press.
Kruglanski, A. W., Bélanger, J. J., Chen, X., Köpetz, C., Pierro, A., & Mannetti, L. (2012). The energetics of motivated cognition: A force-field analysis. Psychological Review, 119(1), 1-20. http://dx.doi.org/10.1037/a0025488
Kruglanski, A. W., & Webster, D. M. (1996). Motivated closing of the mind: “seizing” and “freezing.”. Psychological Review, 103(2), 263-283. http://dx.doi.org/10.1037/0033-295X.103.2.263
Lambert, S. J. (2000). Added benefits: The link between work-life benefits and organizational citizenship behavior. Academy of Management Journal, 43(5), 801-815. https://doi.org/10.5465/1556411
Mussel, P. (2010). Epistemic curiosity and related constructs: Lacking evidence of discriminant validity. Personality and Individual Differences, 49(5), 506-510. https://doi.org/10.1016/j.paid.2010.05.014
Roach, M., & Sauermann, H. (2017). The declining interest in an academic career. PLoS One, 12(9), e0184130. https://doi.org/10.1371/journal.pone.0184130
Roets, A., Kruglanski, A. W., Kossowska, M., Pierro, A., & Hong, Y. Y. (2015). The motivated gatekeeper of our minds: new directions in need for closure theory and research. Advances in Experimental Social Psychology, 52, 221-283. Academic Press. https://doi.org/10.1016/bs.aesp.2015.01.001
Roets, A., & Van Hiel, A. (2011). Item selection and validation of a brief, 15-item version of the Need for Closure Scale. Personality and Individual Differences, 50(1), 90-94. https://doi.org/10.1016/j.paid.2010.09.004
Ryan, R. M., & Deci, E. L. (2000). Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. American Psychologist, 55(1), 68-78. http://dx.doi.org/10.1037/0003-066X.55.1.68
Shoss, M. K., Eisenberger, R., Restubog, S. L., & Zagenczyk, T. J. (2013). Blaming the organization for abusive supervision: The roles of perceived organizational support and supervisor’s organizational embodiment. Journal of Applied Psychology, 98(1), 158-168. http://dx.doi.org/10.1037/a0030687
Szumowska, E., & Kossowska, M. (2016). Need for closure and multitasking performance: The role of shifting ability. Personality and Individual Differences, 96, 12-17. https://doi.org/10.1016/j.paid.2016.02.055
Szumowska, E., & Kossowska, M. (2017). Need for cognitive closure and attention allocation during multitasking: Evidence from eye-tracking studies. Personality and Individual Differences, 111, 272-280. https://doi.org/10.1016/j.paid.2017.02.014
Taylor, G., Jungert, T., Mageau, G. A., Schattke, K., Dedic, H., Rosenfield, S., & Koestner, R. (2014). A self-determination theory approach to predicting school achievement over time: The unique role of intrinsic motivation. Contemporary Educational Psychology, 39(4), 342-358. https://doi.org/10.1016/j.cedpsych.2014.08.002
*Zhi Xiong Chen
Department of Physiology,
Yong Loo Lin School of Medicine,
National University of Singapore,
2 Medical Drive, MD9, Singapore 117593
Tel: +65 6516 3231
E-mail: zhixiong_chen@nus.edu.sg
Published online: 7 January, TAPS 2020, 5(1), 16-24
DOI: https://doi.org/10.29060/TAPS.2020-5-1/OA2126
Junji Haruta1, Ai Oishi2 & Naoko Den3
1Department of Medical Education, Faculty of Medicine, University of Tsukuba, Japan; 2Primary Palliative Care Research Group, Centre for Population Health Sciences, Usher Institute of Population Health Sciences and Informatics, University of Edinburgh, United Kingdom; 3Ouji-Seikyo Hospital, Japan
Abstract
Background: Studies have reported positive impacts from community engagement in end-of-life (EoL) care. However, few studies have used a narrative for health promotion. Thus, we examined how and what lay participants learned through an EoL care education program using narrative.
Methods: A case study in educational research was implemented through qualitative process evaluation. The program was conducted in a hospital in Japan. Participants living in the surrounding community were recruited by convenience sampling. We conducted 90-minute focus groups with participants at two and eight months after the completion of the program. All data were audio-recorded, transcribed verbatim, and analysed using thematic analysis.
Result: We identified five themes. First, participants reconstructed the concept of EoL care using their own experience and new knowledge gained in the program. Second, the stories in the program stimulated participants to recall their feelings and emotions, which caused catharsis effects. Third, the stories evoked other perspectives through metacognition. Fourth, their experience inspired altruism towards patients and their families at the EoL. Fifth, they reflected on their own deaths as an extension of their relationship with others. This learning process was consistent with Kolb’s experiential learning. Their experience enabled lay participants to overcome the existential terror of death while using the narrative mode of thinking to perceive their relationship with others as a symbolic identity.
Conclusion: The educational program using narrative deepened lay participants’ understanding of the concept of EoL care. Such programs have the potential to enhance community engagement in EoL care.
Keywords: Lay-People Learning, Public Health, Palliative Care, Qualitative Research, Narrative Medicine
Practice Highlights
- We developed an end-of-life (EoL) care education program using narrative, and have clarified how and what lay-people learned through the program.
- Interaction among laypeople inspired the five process; reconstructing their understanding, recalling emotions, evoking other perspectives, inspiring altruism and reflection on their own death.
- A narrative about end-of-life care created the opportunities to face the inconceivable death and deepened lay participants’ understanding of the concept of EoL care.
- A narrative has the potential to enhance the engagement of the community in EoL care.
I. INTRODUCTION
The World Health Organization recommends that end-of-life (EoL) care be approached by integrating general population with hospital-level care (World Health Organization, 2014). While EoL care and health promotion are understood to belong to different categories (Rosenberg & Yates, 2010), there is a need for a more open societal attitude in facing and discussing death and dying (Kellehear, 2012). In addition to individuals who are receiving EoL care themselves, their family and social group also become aware of their own health and well-being in the context of life-limiting illnesses (Radbruch et al., 2009). However, laypeople tend to experience more problems near death than medical professionals, such as stigma and loneliness, which might cause distress among patients and their families. Various education programs have been developed around the world to solve these problems.
Our review of published education programs for EoL care found that community resources have been used in a number of projects, such as naturally occurring social networks (Leonard, Horsfall, & Noonan, 2015; Mills, Rosenberg, & McInerney, 2015) and externally facilitated networks (Leonard et al., 2015). Community resources have also been used in direct support from trained community volunteers (Jack, Kirton, Birakurataki, & Merriman, 2011), and in programs such as work with schools (Hartley, 2012), businesses (Hall, Shucksmith, & Russell, 2013) and professionals (Richardson, 2002). Further, seed grants have been awarded to support community-led projects in the field of death, dying, loss and care (McLoughlin, 2013.). Conducting a program requires several areas of focus, such as writing a will and advance care planning (Seymour, Almack, Kennedy, & Froggatt, 2013), but can also involve exploring society’s perception of death and dying through local or national conversation (Patterson & Hazelwood, 2014) or improving the experiences of those living with life-limiting illnesses (Mitchell & Burton, 2006). However, few studies have examined how laypeople learn in education programs.
Story-based learning (McQuiggan, Rowe, Lee, & Lester, 2008), which combines story contexts and pedagogical support strategies, may be an effective way to deliver an educational experience because laypeople are more likely to adopt the narrative mode over the logico-scientific mode of thinking (Clandinin & Connelly, 2000). Narratives are widely used in public health promotion in the UK (Talley, 2011). However, a systematic review of narrative-based interventions for health promotion concluded that more research is needed to determine how these interventions can best be used (Perrier & Martin Ginis, 2016). Process evaluation can allow the examination of participant views on the intervention, as well as investigation of any contextual factors and determination of the processes that mediate observed intervention effects (Al-HadiHasan, Callaghan, & Lymn, 2017). It is important to evaluate “how” laypeople learn in public health promotion, as the learning process uses narrative to improve health literacy.
II. METHODS
A. Aim
We clarified how lay participants learned through an EoL care education program using narrative.
B. Design
We conducted a case study in educational research (Creswell, 2012). The case was constructed by the interaction of laypersons and healthcare professionals, with a program constructed using narrative. Since our focus was on gaining an in-depth picture of the learning process through narrative among individuals, we involved only a series of cases in a community hospital. To focus on the learning process of lay participants, we undertook qualitative process evaluation using audio-recordings of the group dialogue in each session and focus group (FG). We reported in accordance with the consolidated criteria for reporting qualitative research guidelines (Tong, Sainsbury, & Craig, 2007).
| Session | Date | Theme | Content | Assignment | Leading professional |
| 1 | 24 Jul 2014 | Sharing the experience of palliative care | Lecture: What is palliative care?
Video: Narratives of cancer patients Group discussion |
To write your understanding of palliative care based on the lecture and book readings | Physician |
| 2 | 25 Sep 2014 | Understanding the changes experienced by people who are facing death and discussing how we can support them | Lecture: Process of acceptance and active listening
Group discussion |
To write your understanding of the lecture and book readings | Nurse
Medical social worker |
| 3 | 27 Nov 2014 | Engaging in decision making for your loved one | Lecture: Process of decision making
Role play: Professionals conduct a brief role play of a case Group discussion |
To reflect on one’s view of life and death and thoughts for one’s family, and to write these down in a letter | Physician
Physical therapist |
| 4 | 26 Feb 2015 | Our view on life and death
|
Sharing the assignment from the previous session | Nurse
Pharmacist |
Table 1. Contents of the program
C. Setting of the Education Program
The study setting was a 150-bed hospital in Tokyo with a palliative care unit established in May 2014. We delivered a community education program to laypeople at the hospital to enhance their understanding of EoL care from July 2014 to February 2015. The learning outcome of the program was “to learn together about EoL care and to take action to promote health and well-being at the EoL based on one’s own values”. We adopted a narrative-centred approach as a learning strategy. Narrative-centred learning is defined as a narrative pedagogy that integrates methods such as case method teaching and problem-based learning to encourage self-directed learning and participant engagement (McQuiggan et al., 2008). Each session was 2 hours, during which the participants were engaged in constructing and telling stories in a small group. Healthcare professionals in the hospital played the role of facilitators, after prompting information from the lecture was given (Table 1). Participants were given an assignment at the end of each session to write their own story relating to the given topic. If a lay participant could not participate in the session, he or she was asked to watch a video recording of the session. We deliberately placed a 3-month interval between sessions with the expectation that participants would reflect on what they had learned from the sessions in their daily lives.
D. Participants
Using a community publication on health information produced by the hospital and convenience sampling, we recruited laypeople living in the catchment area of the hospital to attend all four sessions of the program (Babbie, 2007). Lay participants contacted the hospital after having seen an advertisement for the course in the community publication. The first author (JH, male) sent letters to the participants to confirm their willingness to participate in the study. We did not establish exclusion/inclusion criteria for literacy level or health status. Since JH and the third author (ND, female) had worked in the hospital, some lay participants knew JH and ND. Other participants built a proper relationship with JH and ND through the EoL program. At the start of the program, during the educational sessions, and during the FGs, we informed the participants that they were not obliged to talk and could leave if they became emotionally upset or experienced a breakdown.
E. Data Generation
All group dialogues during three sessions (excluding the fourth session in order that participants did not hesitate to share their own view on life and death) in a room of the hospital were audio-recorded to mainly focus on the learning process. Additionally, we conducted three 90-minute FGs, namely two FGs within one month after completion of the program and a third FG eight months after completion. JH facilitated the FGs using prompt questions and took field notes while preparing and conducting the program and in post-program FGs. All FGs were conducted in a quiet room in the hospital. All audio-recorded dialogue and FGs were transcribed verbatim by JH. We could not return the transcripts to lay participants because some participants were reluctant to do so. Accordingly, AO and healthcare professionals who joined the program checked for discrepancies between group dialogues during the three sessions and the verbatim transcriptions of the FGs. JH was a general physician in the hospital and a final-year PhD student at the time of data collection. JH had received training in qualitative research as part of the PhD program.
|
Table 2. Prompting questions in FGs
F. Analysis
A thematic analysis was adapted for data analysis (Braun & Clarke, 2006). First, JH and second author (AO, female) separately read and deductively coded the transcripts. AO had undertaken qualitative research training by the time of data analysis in the UK. JH then created inductive codes based on the research questions and initial coding, with any disagreements with AO resolved by discussion. Once JH and AO agreed on the coding, all researchers discussed the themes that emerged from the codes and how these themes interacted until we were in full agreement. The whole process was iterative, which allowed us to achieve a richer interpretation of the data. Thus, researchers crystallised the data and confirmed the interpretation based on the field notes as a triangulation process.
III. RESULTS
A. Participants
Eighteen laypeople living in the local area of the hospital participated in this program. All participants were aged 50–70 years and all but one participant was female. The backgrounds of all participants and their presence/absence in the four sessions and three FGs are shown in Table 3. Four lay participants watched the video because they could not participate in the session. All cases of absence from the sessions or FGs were due to personal reasons of the participants.
| Background of lay participants | Session 1 | Session 2 | Session 3 | Session 4 | FG 1 | FG 2 | FG 3 | |
| Gender | Age | |||||||
| F | 67 | ○ | ○ | ○ | ― | ― | ― | ― |
| F | 61 | ○ | ○ | ○ | ○ | ― | ― | ― |
| F | 74 | ○ | ○ | ○ | ○ | ○ | ― | ○ |
| F | 65 | ○ | ○ | ○ | ○ | ― | ○ | ○ |
| F | 72 | ○ | ○ | ○ | ○ | ― | ○ | ― |
| F | 53 | ○ | ○ | ○ | ○ | ― | ○ | ― |
| F | 66 | ○ | ○ | ○ | ○ | ― | ― | ○ |
| F | 74 | ○ | ○ | ○ | ― | ― | ― | ― |
| F | 60 | ○ | Video | ○ | ― | ○ | ― | ― |
| F | 51 | ○ | ○ | ― | ○ | ○ | ― | ― |
| F | 69 | ○ | ○ | Video | ○ | ○ | ― | ― |
| F | 60 | ○ | ○ | ○ | ○ | ○ | ― | ― |
| F | 63 | ○ | Video | Video | ○ | ― | ○ | ○ |
| F | 64 | ○ | ○ | ○ | ○ | ― | ○ | ○ |
| M | 74 | ○ | ○ | ○ | ○ | ― | ― | ○ |
| F | 63 | ○ | ○ | ○ | ○ | ― | ― | ― |
| F | 71 | ○ | ― | ○ | ○ | ― | ― | ― |
| F | 67 | ○ | ○ | ― | ― | ― | ― | ― |
Note: FG 1, FG2 – Focus groups within one month after completing the program.
FG 3– Focus group eight months later after completing the program.
Table 3. Backgrounds of all participants and presence (〇)/absence (-) in four sessions and three FGs
| Themes | Sub-themes | Example of the texts |
| Reconstructing the concept of EoL care
|
Correcting the previous knowledge of palliative care
|
“I thought that palliative care was the same as hospice care. However, my understanding of palliative care has changed since I was diagnosed with cancer and was advised that palliative care would start at the start of treatment.” |
| Connecting the knowledge of palliative care with real world | “I understood the connection with the community. Not many people know about community palliative care. I likewise did not know anything about these services before attending the program.” | |
| Contributing to the spread of knowledge on palliative care | “I show photos of the books used in the program on my blog and have described what I learned in the program and my thoughts on palliative care. This has become my most popular post ever.” | |
| Recalling feelings and emotions | Conflict between patient’s hope and hospital rules | “Because my husband pulled out the infusion needles himself, he was tied up to the bed and said that he was treated like a criminal. “ |
| Regret regarding a late transition to palliative care | “If I had known about palliative care earlier, I could have had him receive palliative care earlier.” | |
| Perplexity about an acquaintance discontinuing treatment | “My teacher (living with metastatic breast cancer) says that she is thinking of stopping medical treatment because she thinks it is a waste of money and makes her feel guilty. I think that she should receive medical treatment for as long as she can.” | |
| Catharsis effect | “My husband died two years ago. I think that I have become able to accept his death since attending the program. Learning and having a chance to learn have helped me to accept my mental condition of the past two years. I feel calm now.” | |
| Embarrassment in real experiences | “I have a friend in hospital. When I went to see her previously, we talked a lot about the many funny things that have happened in the past to help her remember. However, we did not talk much when I visited last time. I could not find the words when I noticed she was facing her own death. Since then I have been thinking about how I should behave in front of friends’ family members and what I can do for my friend as a person.” | |
| Evoked other perspectives through metacognition | Differences between theirs’ and others’ perspectives | “I was impressed by the explanation about anger. I thought that I might be unable to accept anger.” |
| “The role plays allowed watchers to consider what they should do if they were put in the same situation. I think this was good.” | ||
| Differences among family members | “Because I only have sons, I get feelings of wishing I had a daughter like the oldest daughter who looks after her parents in the role play.” | |
| Differences among professionals | “I think it is preferable that specialists help families overcome such difficulties.” | |
| Inspiring altruism | Motivation to commit to supporting others in EoL | “For me, I want cancer patients and their families to spend the rest of their lives in peace.” |
| Reflecting on their own impending death | Mitigating their fear of death | “I don’t think it is necessary to be afraid of death but I am confident that I have been living well up until now.” |
| Appreciation of others | “When I die, I want to say “thank you” to my family and friends.” | |
| “I think that family members should mentally support the patient; so, it is better to ask them to look after me than to not ask at all.” |
Table 4. Emergent themes and sub-themes based on analysis of group dialogue and FGs
We focused on how laypeople learned in the program throughout the study. A total of 12 lay participants participated in the FGs. Through the analysis, we extracted five themes: reconstructing the concept of EoL care, recalling feelings and emotions, evoking other perspectives through metacognition, inspiring altruism, and reflection on one’s own death (Table 4).
B. Theme Analysis
1) Reconstructing the concept of EoL care: The program deepened participants’ understanding of the concept of EoL care by allowing them to compare their own experience with relatives or friends at the EoL and their image of EoL with those of other participants. Each session led participants to reconstruct their stories about the EoL. Triggered by these stories, participants discovered situations in their daily lives with a link to EoL, as follows.
“I thought that hospices were a place where morphine would be given to patients until their death. I have learned a lot about palliative care from the program, which has improved my understanding of palliative care.”
Additionally, reading related books that were introduced in a series of sessions and dialogue with others allowed them to consolidate and articulate their previously vague understandings. For example, they generated a new understanding of EoL care by reflecting on such things as their own experience after gaining new knowledge about the difference between hospice care in a palliative care unit and the concept of EoL care, including its connection with the community and family/psychological support, and realisation of the spread of EoL care, as follows.
“I reached the conviction that I could receive family/psychological support. I have learned that if my husband is admitted to this hospital, I will also be supported as a family member.”
Furthermore, their new-found understanding motivated them to contribute to disseminate the ‘right’ concept of EoL. On the other hand, some healthcare professionals who joined the small group dialogues as facilitators faced challenges in being unable to control the participants’ story-telling.
2) Recalling feelings and emotions: Constructing stories stimulated participants to recall their inner experiences and emotions. As a result, participants verbalised their recalled feelings such as conflict, regret and perplexity in a group dialogue. This verbalisation of their emotions was a catharsis of the stress they had felt, as follows.
“My husband died two years ago. I think that I have become able to accept his death since attending the program. Learning and having a chance to learn have helped me to accept my mental condition of the past two years. I feel calm now.”
Moreover, through the program, participants embodied emotions associated with their experience with relatives or friends at the EoL when recalling their internal feelings. These narrative-based experiences widened their cognitive understanding of EoL care at the emotional level.
3) Evocation of other perspectives through metacognition: Specific external experiences during the sessions stimulated participants’ interest. Additionally, by verbalising their interests, participants noticed their emotions, differences between their own and others’ perspectives, and the context to which they belonged, such as families and professionals. Participants understood the need for expert assistance as they came to understand these perspectives. For example, participants showed appreciation to healthcare professionals for providing emotional support and management, which was given according to the different perspectives of different family members, as follows.
“I thought that families of cancer patients could not be as generous to patients’ emotional changes, including anger as the family in the role play. I think it is preferable that specialists help families overcome such difficulties.
Through their cognition of other perspectives, they learnt how to access self-monitoring and self-representation as metacognition.
4) Inspiring altruism: Considering the understanding of EoL care inspired altruism as a latent need, defined as a desire that cannot be expected to articulate due to a lack of information (Langford, 1995). Participants expressed their understanding of EoL as stories through their participation in the program and their reading of books, which reminded them of their altruistic feelings, embedded as latent needs. Participants were motivated to commit to supporting patients and their families who were suffering at the EoL as volunteers.
“For me, I want cancer patients and their families to spend the rest of their lives in peace. And I have learned to feel compassion for families with cancer patients. It is important to support such families.”
5) Reflecting on their own impending death: By gaining an understanding of EoL care, during which time they consulted with others who felt fear and anxiety regarding facing their death, participants started to anticipate their own deaths. This helped them to alleviate their fear and anxiety on the subject. In addition, they developed an appreciation for those on whom they will rely at their own EoL.
“I used to think that death was cruel, painful and scary, but I do not really think that now because there are people we can talk to as part of palliative care services. I don’t think it is necessary to be afraid of death but I am confident that I have been living well up until now.”
IV. DISCUSSION
We described laypeople’s learning patterns through an EoL care education program, in which EoL care through narrative-centred learning and interactions with other participants inspired five processes, namely reconstructing their understanding, recalling emotions, evoking other perspectives, inspiring altruism and reflection on their own death. The process led them to convince that EoL was individual for every person and the EoL care was rooted in the understanding of their own life.
Lay participants learned not only about EoL care but also about the value of their own life in this education program. In previous studies of palliative education for healthcare professionals, undergraduate education on palliative care covers humanistic aspects and holistic views (Centeno, Ballesteros, Carrasco, & Arantzamendi, 2016; Horowitz, Gramling, & Quill, 2014). In graduate education, palliative care experts define comprehensive and essential palliative care competencies for internal medicine or family medicine residents, and residents improve their knowledge in a 2-week palliative rotation (Olden, Quill, Bordley, & Ladwig, 2009; Schaefer et al., 2014). In reality, it is nonetheless difficult for residents to alleviate the psychological distress felt by patients and families in palliative care (McFarland, Maki, & Holland, 2015). Considering this challenge, it is understandable that laypeople are more likely to harbour a stereotyped understanding of EoL and stigma around death compared to healthcare students or professionals. However, this study suggests that constructing stories enables lay participants to recognise their perception of the EoL and reflect on their own experience and feelings, similar to healthcare professionals (Arai et al., 2017). Narratives evoked participants’ feelings and induced a catharsis of emotions after they expressed and verbalised these feelings. Through this process, lay participants acquired metacognition of death and dying by sharing and verbalising their own understanding and feelings about dying and well-being, which voluntarily promoted an altruistic desire to commit to EoL care and motivated them to contribute to disseminating the interpretation of EoL. In addition, they had opportunities to leverage their own existing experiences based on constructing stories, which is different from Kolb’s experiential learning (Kolb, 1984). In previous health education programs, health professionals used information from standard epidemiological studies to change the misapprehensions of laypeople (Allmark & Tod, 2006; McConnachie, Hunt, Emslie, Hart, & Watt, 2001; Prior, 2003). However, in addition to providing knowledge, encouraging participants to construct their own stories deepened their understanding of EoL care with respect to their own values. While lay participants reflected on their own impending death, lay participants anticipated death as an extension of their own life and learned how healthcare professionals provide care to dying patients and their families through stories. Moreover, lay participants anticipated their own death with respect to their relationship with others. In social psychology, existential terrors, which are a basic psychological conflict that results from having a self-preservation instinct whilst realising that death is inevitable, can be managed by embracing cultural values or symbolic systems that provide enduring meaning and value to life (Curtis & Biran, 2001). A narrative-based program may provide laypeople with a sense that they are connected to someone, which will ultimately enable laypeople to deflect fear and manage their fear of death. Through this process, participants may attain an altruistic desire to express personal preferences for situations in which others benefit (Batson, 1997) because they realise the stress of the situation on others and develop respect for their well-being (Batson, 2010). Lay participants gained enhanced empathy for patients or their families who were suffering in the face of death and dying, which motivated altruistic behaviours to commit to EoL care.
Throughout the narrative-centred learning, rather than learning through structured knowledge in textbooks and lectures from healthcare professionals, lay participants reconstructed their own narratives consisting of a series of actions and stories describing concrete events and experiences. Bruner illustrated that there are two distinct modes of understanding (Bruner, 2009). The first is the logico-scientific mode of organised thinking based on reason. The second is the narrative mode associated with the creation of stories. People complementarily use the two cognitive modes to understand the world according to the situation. Laypeople are more likely to adopt the narrative mode in daily life. Through communication with others, laypeople realise how they understand the world they live in. However, healthcare professionals tend to use the logico-scientific mode in public health promotion for laypeople because they themselves learned through structured knowledge in textbooks. This leads to a mismatch between healthcare professionals and laypeople, and highlights the need to reflect on differences in modes of thinking when developing learning strategies. A chain or sequence of narratives from scattered experiences can be connected and arranged into an identifiable structure (Prins, Avraamidou, & Goedhart, 2017). In addition, stories motivate people to identify novel perceptual, emotional, and motivational experiences and are suited to alternative learning paradigms such as guided discovery (McQuiggan et al., 2008). Lay participants were able to enhance their understanding of the EoL through sharing and comparing their experiences with each other using the narrative mode. As a result, they acquired the metacognition and motivation to commit to the suffering of others.
A. Strengths and Limitations
There are three main limitations of this study. First, lay participants who participated in the program might be more open to learning about EoL among the general population. However, most participants initially misunderstood the concept of EoL care and some hesitated to share their experiences with relatives or friends at the EoL. This narrative-based approach was useful for such participants in deepening their understanding of EoL care and leading them to acknowledge that death is an extension of life. Second, two researchers (JH and ND) participated in developing the program and JH acted as a facilitator in the FGs. While we tried to provide a neutral environment and asked questions to encourage free speech, we may have asked inductive questions. Additionally, lay participants might have unconsciously or consciously mimicked the intentions of researchers due to self-selection bias and reporting bias because they agreed to participate in the study. To evaluate data credibility, JH, ND and another researcher (AO) who did not participate in running the program conducted a triangulation of the data (Walker, Holloway, & Wheeler, 2005). We assessed data that arose from free, frank and honest interactions and found that the group which included one particular researcher (JH) maintained a good relationship in which everyone asked frank questions or provided dissenting opinions. We might have missed critical views which could have been raised by other potential participants who were absent at the FGs. Third, we could not follow up on outcomes such as engaging community and social networks. Further study is needed to continue participation observations and follow-up to determine the longer-term outcomes of this narrative-based program.
V. CONCLUSION
We evaluated the process of a health education program on EoL care using the strategy of narrative-centred learning. Lay participants deepened their understanding of EoL care while reconstructing their knowledge, recalling their own experiences and emotions, evoking other perspectives, inspiring altruism and reflecting on their own deaths. Such a program has the potential to enhance community engagement in EoL care.
Notes on Contributors
JH, AO and ND contributed to the design and implementation of the research, analysis of the results and writing of the manuscript.
Ethical Approval
This study was reviewed and approved by the ethical committee of the hospital (No. 69), which considered sampling, informed consent, and the confidentiality of participants. All participants provided written informed consent for participation and audio-recordings of the group dialogue and FGs.
Acknowledgements
We sincerely appreciate the healthcare professional staff at the palliative care unit in the hospital used as a study setting.
Funding
This work was supported by a grant-in-aid from Japan Primary Care Association (no grand number, from April 2014 to March 2016).
Declaration of Interest
The authors declare that they have no competing interests.
References
Al-HadiHasan, A., Callaghan, P., & Lymn, J. S. (2017). Qualitative process evaluation of a psycho-educational intervention targeted at people diagnosed with schizophrenia and their primary caregivers in Jordan. BMC Psychiatry, 17(1).
http://doi.org/10.1186/s12888-017-1225-2
Allmark, P., & Tod, A. (2006). How should public health professionals engage with lay epidemiology? Journal of Medical Ethics,32(8).
http://doi.org/10.1136/jme.2005.014035
Arai, K., Saiki, T., Imafuku, R., Kawakami, C., Fujisaki, K., & Suzuki, Y. (2017). What do Japanese residents learn from treating dying patients? The implications for training in end-of-life care. BMC Medical Education, 17(1), 205.
http://doi.org/10.1186/s12909-017-1029-6
Babbie, E. (2007). The Ethics and Politics of Social Research. In E. Babbie (Ed.), The Practice of Social Research (11th ed.).
Belmont, CA: Thomson Wadsworth.
Batson, C. D. (1997). Self-other merging and the empathy-altruism hypothesis: Reply to Neuberg et al. (1997). Journal of Personality and Social Psychology,73(3), 517–522.
http://doi.org/10.1037/0022-3514.73.3.517
Batson, C. D. (2010). Empathy-induced altruistic motivation. In M. Mikulincer & P. R. Shaver (Eds.), Prosocial motives, emotions, and behavior: The better angels of our nature. Washington, DC, US: American Psychological Association.
http://dx.doi.org/10.1037/12061-001
Braun, V., & Clarke, V. (2006). Using thematic analysis in psychology, 3, 77–101.
http://doi.org/10.1191/1478088706qp063oa
Bruner, J. S. (2009). Actual Minds, Possible Worlds. Cambridge, Mass: Harvard University Press.
Centeno, C., Ballesteros, M., Carrasco, J. M., & Arantzamendi, M. (2016). Does palliative care education matter to medical students? The experience of attending an undergraduate course in palliative care. BMJ Supportive & Palliative Care, 6(1), 128–134. http://doi.org/10.1136/bmjspcare-2014-000646
Clandinin, D. J., & Connelly, F. M. (2000). Narrative inquiry: Experience and story in qualitative research. Narrative Inquiry. http://doi.org/10.1111/j.1365-2850.2008.01331.x
Creswell, J. W. (2012). Educational research: Planning, conducting, and evaluating quantitative and qualitative research (4th ed.). Boston, MA: Pearson.
Curtis, V., & Biran, A. (2001). Dirt, disgust, and disease: Is hygiene in our genes? Perspectives in biology and medicine, 44(1), 17–31. http://doi.org/10.1353/pbm.2001.0001
Langford, D. P., & Cleary, B. A. (1995). Orchestrating Learning With Quality. Milwaukee, WI: American Society for Quality.
Hall, D., Shucksmith, J., & Russell, S. (2013). Building a compassionate community: Developing an informed and caring workplace in response to employee bereavement. Bereavement Care, 32(1), 4–10.
http://doi.org/10.1080/02682621.2013.779819
Hartley, N. (2012). ‘Let’s talk about dying’: Changing attitudes towards hospices and the end of life. In Sallnow L, Kumar S, Kellehear A (Eds.), International Perspectives on Public Health and Palliative Care (pp. 156–7). Abingdon: Routledge. http://doi.org/10.4324/9780203803189
Horowitz, R., Gramling, R., & Quill, T. (2014). Palliative care education in US medical schools. Medical Education, 48(1), 59–66. http://doi.org/10.1111/medu.12292
Jack, B. A., Kirton, J., Birakurataki, J., & Merriman, A. (2011). “A bridge to the hospice”: The impact of a community volunteer programme in Uganda. Palliative Medicine, 25(7), 706–715. http://doi.org/10.1177/0269216310397566
Kellehear, A. (2012). Compassionate cities: Public health and end-of-life care. QJM: An International Journal of Medicine, 106(12), 1071–1075. http://doi.org/10.4324/9780203019955
Kolb, D. A. (1984). Experiential learning:experience as the source of learning and development. Upper Sadle River: Prentice-Hall.
Leonard, R., Horsfall, D., & Noonan, K. (2015). Identifying changes in the support networks of end-of-life carers using social network analysis. BMJ Supportive and Palliative Care, 5(2), 153–159. http://doi.org/10.1136/bmjspcare-2012-000257
McConnachie, A., Hunt, K., Emslie, C., Hart, C., & Watt, G. (2001). “Unwarranted survivals” and “anomalous deaths” from coronary heart disease: prospective survey of general population. BMJ, 323(7327), 1487–1491.
http://doi.org/10.1136/bmj.323.7327.1487
McFarland, D. C., Maki, R. G., & Holland, J. (2015). Psychological distress of internal medicine residents rotating on a hematology and oncology ward: An exploratory study of patient deaths, personal stress, and attributed meaning. Medical Science Educator, 25(4), 413–420.
http://doi.org/10.1007/s40670-015-0159-x
McLoughlin, K. (2013). Compassionate Communities Project Evaluation Report. Retrieved from http://hdl.handle.net/101-47/621066
McQuiggan, S. W., Rowe, J. P., Lee, S., & Lester, J. C. (2008). Story-based learning: The impact of narrative on learning experiences and outcomes. In International Conference on Intelligent Tutoring Systems, 5091, 530–539. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-540-69132-7_56
Mills, J., Rosenberg, J. P., & McInerney, F. (2015). Building community capacity for end of life: an investigation of community capacity and its implications for health-promoting palliative care in the Australian Capital Territory. Critical Public Health, 25(2), 218–230. http://doi.org/10.1080/09581596.2014.945396
Mitchell, L., & Burton, E. (2006). Neighbourhoods for life: Designing dementia‐friendly outdoor environments. Quality in Ageing and Older Adults, 7(1), 26–33.
http://doi.org/10.1108/14717794200600005
Olden, A. M., Quill, T. E., Bordley, D., & Ladwig, S. (2009). Evaluation of a required palliative care rotation for internal medicine residents. Journal of Palliative Medicine, 12(2), 150–154. http://doi.org/10.1089/jpm.2008.0246
Patterson, R., & Hazelwood, M. (2014). ‘Dining with Death’ – conversation menus as a means of educating people about death, dying and bereavement. BMJ Supportive & Palliative Care, 4(Suppl 1), A77.
http://doi.org/10.1136/bmjspcare-2014-000654.219
Perrier, M.-J., & Martin Ginis, K. A. (2016). Changing health-promoting behaviours through narrative interventions: A systematic review. Journal of Health Psychology, 23(11), 1499–1517. http://doi.org/10.1177/1359105316656243
Prins, R., Avraamidou, L., & Goedhart, M. (2017). Tell me a Story: the use of narrative as a learning tool for natural selection. Educational Media International, 54(1), 20–33.
http://doi.org/10.1080/09523987.2017.1324361
Prior, L. (2003). Belief, knowledge and expertise: the emergence of the lay expert in medical sociology. Sociology of Health & Illness, 25(3), 41–57. http://doi.org/10.1111/1467-9566.00339
Radbruch, L., Payne, S., Bercovitch, M., Caraceni, A., De Vlieger, T., Firth, P., … De Conno, F. (2009). White Paper on standards and norms for hospice and palliative care in Europe: Part 1. European Journal of Palliative Care, 16(6), 278–289.
Richardson, J. (2002). Health promotion in palliative care: The patients’ perception of therapeutic interaction with the palliative nurse in the primary care setting. Journal of Advanced Nursing, 40(4), 432–440. http://doi.org/10.1046/j.1365-2648.2002.02391.x
Rosenberg, J. P., & Yates, P. M. (2010). Health promotion in palliative care: The case for conceptual congruence. Critical Public Health, 20(2), 201–210.
http://doi.org/10.1080/09581590902897394
Schaefer, K. G., Chittenden, E. H., Sullivan, A. M., Periyakoil, V. S., Morrison, L. J., Carey, E. C., … Block, S. D. (2014). Raising the bar for the care of seriously ill patients: Results of a national survey to define essential palliative care competencies for medical students and residents. Academic Medicine: Journal of the Association of American Medical Colleges, 89(7), 1024–1031.
http://doi.org/10.1097/ACM.0000000000000271
Seymour, J. E., Almack, K., Kennedy, S., & Froggatt, K. (2013). Peer education for advance care planning: Volunteers’ perspectives on training and community engagement activities. Health Expectations, 16(1), 43–55.
http://doi.org/10.1111/j.1369-7625.2011.00688.x
Talley, J. (2011). Metaphor, narrative, and the promotion of public health. Genre: Forms of Discourse and Culture, 44(3), 405–423. http://doi.org/10.1215/00166928-1407576
Tong, A., Sainsbury, P., & Craig, J. (2007). Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. International Journal for Quality in Health Care, 19(6), 349–357.
http://doi.org/10.1093/intqhc/mzm042
Walker, J., Holloway, I., & Wheeler, S. (2005). Guidelines for Ethical Review of Qualitative Research. Research Ethics Review, 1(3), 90–96.
http://doi.org/10.1177/174701610500100304
World Health Organization. (2014). Strengthening of palliative care as a component of integrated treatment throughout the life course. Journal of Pain & Palliative Care Pharmacotherapy, 28(2), 130–134.
http://doi.org/10.3109/15360288.2014.911801
*Junji Haruta
1-1-1 Tennoudai, Tsukuba,
Ibaraki, 305–8576 Japan
Tel: +81-29-853-3189
Email:junharujp@md.tsukuba.ac.jp
junharujp@gmail.com
Published online: 3 September, TAPS 2019, 4(3), 91-98
DOI: https://doi.org/10.29060/TAPS.2019-4-3/OA2091
Caitlin Harrison1, Rhys Jones2 & Marcus A. Henning3
1The University of Auckland, Aotearoa, New Zealand; 2Te Kupenga Hauora Māori, The University of Auckland, Aotearoa, New Zealand; 3Centre for Medical and Health Sciences Education, The University of Auckland, Aotearoa, New Zealand
Abstract
Formal Indigenous health curricula often exist in institutional contexts that tacitly condone racist discourses that are at odds with the goal of developing culturally safe health professionals. Recognition of the impact of informal and hidden curricula on learners has increased, yet few studies have provided empirical evidence about this aspect of health professional education. This study sought to examine characterisations of Māori (Indigenous New Zealanders) in learning environments at the University of Auckland’s Faculty of Medical and Health Sciences. A cross-sectional study design based on the Stereotype Content Model elicited student perceptions (n = 444) of stereotype content in undergraduate nursing, pharmacy and medical programmes. The Stereotype Content Model identifies interpersonal and intergroup perceptions in relation to warmth and competence. These perceptions are considered fundamental and universal to the impressions people form when meeting one another. Stereotyping is associated with distinct affective and behavioural responses that can lead to discrimination. In this study, students rated perceived warmth and competence characterisations pertaining to four target ethnic groups (Māori, Pacific Nations, Asian and Pākehā/European). Characterisations of Māori warmth were rated lower than Pacific Nations peoples, comparable to Pākehā/European and higher than characterisations of Asian peoples. In reference to competence characterisations, Māori were rated equal to Pacific Nations peoples and lower than both Asian and Pākehā/European peoples. This study’s results highlight a degree of incongruence between the University of Auckland’s formal Māori Health curricula and messages conveyed in the broader institutional context, with implications for educational outcomes and students’ future clinical practice.
Keywords: Indigenous Health, Health Professional Education, Stereotype Content Model, Informal/Hidden Curriculum
Practice Highlights
- Undergraduate nursing, pharmacy and medical students’ perceptions of ethnic group stereotype content in the University of Auckland’s Faculty of Medical and Health Sciences’ learning environments were evaluated to identify areas of incongruence with the formal Hauora Māori (Māori Health) curriculum.
- The findings indicated that characterisations of Māori are incongruent with formal curricular objectives.
- Māori students perceived characterisations of Māori in their learning environments more negatively than non-Māori students.
- The findings have implications for students’ educational outcomes, their future clinical practice, and Māori workforce recruitment and retention.
I. INTRODUCTION
Indigenous health educators work to enact decolonised, anti-racist curriculum and pedagogies (Curtis, Reid, & Jones, 2014; Jones et al., 2019). The need for transformative teaching and learning in this area is evidenced by persistent ethnic inequities in health outcomes and health care quality (Jones et al., 2010; Wilson & Barton, 2012). In Aotearoa, New Zealand, the context for this study, inequities between Māori (the Indigenous peoples of Aotearoa) and non-Māori are apparent across most health measures, including life expectancy, mortality rates, disease-specific morbidity and many of the key health risk factors and determinants of health (Harris et al., 2012; Ministry of Health, 2015; Stats NZ Tatauranga Aotearoa, 2015). Access to and quality of healthcare is inequitable for Māori compared to non-Māori (Hill, Sarfati, Robson, & Blakely, 2013; Jansen & Jansen, 2013), and in the healthcare system, Māori experience racial discrimination by health professionals (Harris et al., 2012).
Formal Indigenous health curricula exist in concert with and in the context of what Hafferty (1998) identified as the ‘informal’ and ‘hidden’ curriculum. Hafferty (1998) described the ‘informal’ and ‘hidden’ curriculum as the implicit learning and teaching that take place within educational institutions and function at the interpersonal and structural levels, respectively. The resulting tacit knowledge, accrued from multiple experiences, is unexamined, taken-for-granted and tends to reproduce the unjust social orders that formal Indigenous health curricula seek to subvert (Paul, Ewen, & Jones, 2014). Hauora Māori (Māori health) academics at the University of Auckland describe the broader institutional culture and context in which they work as one that often conflicts with the formal Māori health curriculum (Jones et al., 2010). Undergraduate medical students at the University of Auckland have demonstrated both explicit and implicit bias in favour of Pākehā/NZ European New Zealanders (Harris et al., 2018), and Māori students in health professional and health science programs report experiences of racism (Curtis et al., 2012).
The main purpose of this study was to identify areas of incongruence between the University of Auckland’s Faculty of Medical and Health Sciences’ (FMHS) undergraduate medical, nursing, and pharmacy degree programme learning environments (i.e. a ‘hidden/informal,’ institutional curriculum) and the formal Hauora Māori curriculum. Although it has been reported that attitudes among students in health professional training programmes are sensitive to the values of their educational contexts (Howe, 2002), comparable group-level studies have not been conducted in other educational institutions.
This study employs the Stereotype Content Model (SCM) as an analytical tool to investigate student perceptions of ethnic group stereotype content pertaining to Māori in the University of Auckland’s health professional education programmes. The SCM synthesised research on interpersonal and intergroup perception processes with patterns of stereotype content, revealing that warmth and competence perceptions are fundamental and universal to the impressions people form when met with an “other” (Fiske, Cuddy, Glick, & Xu, 2002). “Others” who are perceived as having positive intentions toward the perceiver are evaluated as high in warmth. Perceived capability(ies) of an “other” to carry out her/his intentions correlate to perceptions of competence. According to Fiske et al. (2002), warmth and competence’s fundamental positioning is a result of humans’ innate concerns regarding status and competition. If the “other” is perceived as a competitive threat to one’s social status, they will be evaluated as low in warmth but highly competent. People(s) perceived as non-threatening are typically characterised as high in warmth, but low in competence. When applied to populations clear patterns emerge, hence the SCM theorises that socio-structural conditions shape intergroup relations, giving rise to patterns of warmth and competence perceptions (Cuddy, Fiske, & Glick, 2008). All social groups’ stereotype content profiles can be linked to their relative social positioning and the degree to which they are perceived as competing with the dominant group (Pākehā/NZ Europeans in the context of this study; Cuddy et al., 2008).
Stereotype content was identified as a salient construct for enquiry due to racial stereotypes’ role in creating and maintaining ethnic and racial disparities in health care (van Ryn et al., 2011). In healthcare settings, stereotypes impact the perceptions and behaviours of both patients and clinicians. Stereotype activation, an automatic process in which awareness of relevant stereotypes is triggered during an interpersonal interaction, has been identified as a principal component of provider-mediated unconscious bias (Williams & Mohammed, 2013).
When people receive interpersonal or environmental signals, both explicit and implicit, that aspects of their perceivable identity (e.g. skin colour) could trigger negative judgments or mistreatment, the resulting psychological state is defined as ‘stereotype threat’ (Aronson, Burgess, Phelan, & Juarez, 2013). In healthcare interactions, stereotype threat influences clinician and patient behaviour. Clinician behaviours may trigger stereotype threat, which is likely to impact patient behaviours, which then influences clinicians’ subsequent behaviours (Aronson et al., 2013). The endorsement of negative stereotypes is understood to result in discrimination (Dovidio & Fiske, 2012).
A range of common stereotypes about Māori exist in broader New Zealand society (Sibley et al., 2011), and among health care professionals (McCreanor & Nairn, 2002). For example, Penney, Barnes, and McCreanor (2011) revealed a commonplace practice of stereotyping Māori patients as ‘non-compliant,’ a label with significant implications for the patient-provider relationship. Health professional education and training programmes can reinforce stereotypes and influence racial and ethnic bias among learners (Jones et al., 2019; van Ryn et al., 2015). The aim of the present study was to explore student perceptions of stereotype content in the University of Auckland’s FMHS health professional education environments’ characterisations of Māori. The primary research question was, ‘How do undergraduate nursing, pharmacy and medical students perceive characterisations of Māori in their educational environments?’
II. METHODS
A. Participants
A purposive sample of undergraduate nursing, pharmacy and medical students (N = 628) in the University of Auckland’s FMHS were invited to participate.
B. Procedure
Ethics approval for the study was obtained from the University of Auckland Human Participants Ethics Committee. Students were sent an email invitation one week prior to data collection via paper survey. The principal researcher visited each of the five student cohorts’ lectures during Semester One of the 2014 Academic Year to conduct the cross-sectional survey.
C. Measures
1) Stereotype content in learning environments:The questionnaire was based on the SCM (Fiske et al., 2002) and a New Zealand-based study examining societal stereotypes of Māori, Pacific Nations, Pākehā/European and Asian New Zealanders (Sibley et al., 2011).
The questionnaire was organised into four sections: 1) Māori New Zealanders, 2) Pacific Nations New Zealanders, 3) Asian New Zealanders, and 4) Pākeha/European New Zealanders. For each section, students were asked to complete eight stereotype content ratings on a five-point Likert scale of 1 (not at all) to 5 (extremely) that were presented in the following question stem:
How …(warm, likeable, sincere, good-natured, tolerant, competent, intelligent, confident) is this group, as characterised in your learning environments?
The SCM surveys and Sibley et al.’s (2011) survey asked respondents “How… is this group, as viewed by society?” This research project modified the question stem in order to reflect the specific research question and aims.
2) Demographic information:The questionnaire included several items pertaining to participants’ programme of study and demographic characteristics: 1) Programme of study (nursing, pharmacy or medicine); 2) Year of programme; 3) Age in years; 4) Sex; 5) Ethnicity. For data analysis purposes, five participant ethnicity groups were categorised: Māori, Pacific Nations, Asian, Pākehā/NZ European, and Other. It is important to note that the categories Pacific Nations, Asian, and Other are not ethnic groups in themselves, but aggregations of a number of ethnic identities.
 Table 1. Study design
Table 1. Study design
D. Data Analysis
First, the response rate (n/N) and participants’ demographic characteristics were presented with descriptive statistics. The internal reliability of the five items measuring warmth and the three items measuring competence, respectively, were assessed using Cronbach’s alpha. Measures of central tendency in reference to Māori, Pacific Nations, Asian and Pākehā/European New Zealanders’ relative warmth and competence characterisations were determined. In accordance with the study design (Table 1), a 4 (racial/ethnic group: Māori, Pacific Nations, Asian, Pākehā/Europeans) x 2 (stereotype dimension: warmth, competence) repeated measures analysis of variance (ANOVA) was conducted. Post hoc analyses were conducted to examine the extent to which ethnic group characterisations were viewed consistently among participants from each student cohort, various ethnic identities, age group, and sex.
III. RESULTS
A. Response Rate and Participant Data
A total of 444 (response rate = 71%) student surveys were completed and analysed. The nursing, pharmacy and medical student cohorts each contributed approximately one-third of all responses (nnursing= 160, 36%; npharmacy= 149, 34%; nmedicine= 135, 30%). A majority of participants were 24 years old or younger (n = 389, 88%). A majority of the participants identified themselves as female (n = 318, 72%). Participants who identified as belonging to Asian ethnicities comprised 44% (n = 197) of the total sample. Pākehā/NZ European participants were the second most represented ethnic group at 34% (n = 150). Māori participants comprised 7% (n = 31) of all respondents. 5% (n = 22) of participants identified as Pacific Nations peoples, and 10% of participants made up the ‘Other’ category, which included Middle Eastern and African ethnicities. The sample was representative of the student population that was invited to participate. The 71% response rate and sample representativeness indicate that non-response bias was effectively minimised.
B. Internal Consistency Measures
The Cronbach’s alpha (α) internal reliability coefficients for the items assessing warmth-related characterisations of Māori (α = .86), Pacific Nations peoples (α = .90), Asian peoples (α = .87) and Pākehā/European (α = .86), were acceptable (Field, 2005). Internal reliability coefficients for the items assessing competence-related characterisations were generally acceptable, with coefficients of Māori (α = .76), Pacific Nations peoples (α = .83), Asians peoples (α = .65) and Pākehā/European (α = .79). The coefficient for Asian New Zealanders was lower than the recommended .7 cut-off score.
C. Warmth and Competence Characterisations
The 4 (target ethnic group: Māori; Pacific Nations; Asian; Pākehā/European) x 2 (stereotype dimension: warmth, competence) repeated measures ANOVA generated some significant findings. An overall significant interaction was observed, Wilks’ Lambda = .47, F(3,441) = 168.40, p < .001.
| Target Ethnic Group | Warmth | Competence | ||
| Mean | SD | Mean | SD | |
| Māori | 3.55 | .64 | 3.31 | .72 |
| Pacific Nations | 3.73 | .69 | 3.32 | .73 |
| Asian | 3.28 | .71 | 3.90 | .65 |
| Pākehā/European | 3.57 | .61 | 4.02 | .57 |
Note: The mean score reflects participants’ ratings on a 5-point Likert scale.
Table 2. Mean and standard deviation (SD) ratings for the variables warmth and competence by target ethnic group
(N = 444)
Two one-way ANOVAs were conducted to assess perceptions of warmth and competence characterisations by target ethnic group separately. The overall Wilks’ Lambda tests of significance yielded several significant findings. First, differences in mean levels of perceived competence characterisations by target ethnic group were significant, Wilks’ Lambda = .52,F(3,441) = 135.25, p < .001. Second, mean levels of perceived warmth characterisations for each ethnic group were significantly different, Wilks’ Lambda = .77, F(3,441) = 42.91, p < .001. The mean warmth and competence ratings are presented in Table 2.
Using Bonferroni-adjusted alpha levels of .008 (.05/6) to minimise type I error, paired-samples t-tests were conducted and are presented in Table 3 (Bland & Altman, 1995).
D. Influence of Participant Demographic Variables
1) Programmes of study: Multivariate analyses (MANOVA) indicated that students within different programmes of study made different warmth and competence (domains) attributions across the questionnaire’s four target ethnic groups (sections). The overall multivariate analysis results showed significant main effects for sections, F(3,439) = 50.16, p < .001 and domains, F(1,441) = 41.46, p < .001. Two-way significant interaction effects were noted for sections and course of study, F(6,878) = 5.61, p < .001, domains and course of study, F(2,441) = 5.54, p < .01 and domains and sections, F(3,439) = 172.30, p < .001. A three-way significant interaction effect was noted for sections, domains, and course of study, F(6,878) = 2.43, p < .05.
2) Ethnicity:Overall the results showed significant main effects for sections, F(3,437) = 21.02, p < .001 and domains, F(1,439) = 31.25, p < .001. Two-way significant interaction effects were noted for sections and student ethnicity, F(12,1156) = 6.56, p < .001, domains and student ethnicity, F(4,439) = 2.56, p < .05 and domains and sections, F(3,437) = 108.77, p < .001. A three-way significant interaction effect was noted for sections, domains and student ethnicity, F(12,1156) = 2.01, p < .05. The findings suggest that participant ethnicity affected perceptions of warmth and competence ratings across the four sections. The descriptive data for Māori warmth and competence ratings by participant ethnicity are illustrated in Table 4.
The descriptive statistics (Table 4) indicated that characterisations of Māori were perceived differently among students from different ethnic groups. Māori students rated characterisations of Māori warmth lower than students belonging to Pacific Nations, Pākeha/NZ European and Other ethnicities. Māori students rated characterisations of Māori competence as lower than those of the four other participant groups. Students who self-identified as belonging to Pacific Nations ethnicities rated warmth and competence characterisations of Pacific Nations peoples higher than characterisations of Māori. Students belonging to Asian ethnicities rated characterisations of Māori warmth higher than characterisations of Asian peoples, but rated characterisations of Asian peoples’ competence higher than Māori. Pākehā/NZ European students rated characterisations of Māori warmth and Pākeha warmth similarly, but rated Pākehā/NZ European competence characterisations higher than those of Māori.
| Paired Differences | |||||||
| Mean | SD |
95% Confidence Interval of the Difference |
|||||
| Lower | Upper | t | df | ||||
| Competence | Māori vs. Asian* | -0.59 | 0.86 | -0.67 | -0.51 | -14.46 | 443 |
| Māori vs. Pākehā/NZ European* | -0.71 | 0.78 | -0.78 | -0.63 | -19.03 | 443 | |
| Māori vs. Pacific Nations | -0.01 | 0.52 | -0.06 | 0.04 | -0.37 | 443 | |
| Asian vs. Pākehā/NZ European* | -0.12 | 0.73 | -0.18 | -0.05 | -3.40 | 443 | |
| Asian vs. Pacific Nations* | 0.58 | 0.89 | 0.50 | 0.66 | 13.76 | 443 | |
| Pākehā/NZ European vs. Pacific Nations* | 0.70 | 0.80 | 0.62 | 0.77 | 18.28 | 443 | |
| Warmth | Māori vs. Asian* | 0.27 | 0.83 | 0.19 | 0.34 | 6.75 | 443 |
| Māori vs Pākehā/ NZ European | -0.02 | 0.75 | -0.09 | 0.05 | -0.68 | 443 | |
| Māori vs. Pacific Nations* | -0.18 | 0.57 | -0.24 | -0.13 | -6.78 | 443 | |
| Asian vs. Pākehā/NZ European* | -0.29 | 0.81 | -0.37 | -0.21 | -7.54 | 443 | |
| Asian vs. Pacific Nations* | 0.45 | 0.90 | 0.37 | 0.53 | 10.58 | 443 | |
| Pākehā/NZ European vs. Pacific Nations* | 0.16 | 0.84 | 0.08 | 0.24 | 4.01 | 443 | |
Note: *p < .008
Table 3. Paired-samples t-test: Differences in and ratings among target ethnic groups
| Participant Ethnicity | |||||
| Domains | Māori | Pacific Nations | Asian | Pākehā/NZ European | Other |
| Māori Warmth | 3.48 (.66) | 3.62 (.63) | 3.45 (.60) | 3.67 (.64) | 3.60 (.67) |
| Māori Competence | 3.04 (.81) | 3.61 (.83) | 3.25 (.63) | 3.39 (.75) | 3.38 (.75) |
| Pacific Nations Warmth | 3.67 (.59) | 4.08 (.64) | 3.50 (.72) | 3.97 (.59) | 3.80 (.63) |
| Pacific Nations Competence | 3.00 (.80) | 3.65 (.93) | 3.21 (.68) | 3.46 (.72) | 3.40 (.72) |
| Asian Warmth | 3.01 (.72) | 3.52 (.83) | 3.41 (.65) | 3.17 (.72) | 3.17 (.72) |
| Asian Competence | 3.87 (.69) | 4.32 (.67) | 3.94 (.60) | 3.79 (.69) | 3.92 (.61) |
| Pākehā/ NZ European Warmth | 3.48 (.60) | 3.53 (.63) | 3.57 (.61) | 3.67 (.60) | 3.34 (.54) |
| Pākehā/ NZ European Competence | 4.05 (.51) | 4.11 (.58) | 4.04 (.59) | 4.01 (.55) | 3.89 (.55) |
Table 4. Target ethnic group mean (SD) ratings for warmth and competence by participant ethnicity
IV. DISCUSSION
A. Main Finding
This study’s main finding is that undergraduate nursing, pharmacy and medical students perceived unequal warmth and competence characterisations (stereotype content) based on target ethnicity (Māori, Pacific Nations, Asian and Pākehā/European) in their learning environments. Curtis et al. (2012) reported Māori students’ perspectives on the University of Auckland’s FMHS, and negative stereotypical caricatures were one aspect. This study’s main finding expands this point, demonstrating that a broad sample of students, both Māori and non-Māori, detect differential stereotype content pertaining to Māori in their FMHS learning environments. This finding is significant and has implications for three interrelated aspects of medical and health sciences education at the University of Auckland: 1) students’ Hauora Māori educational outcomes, 2) graduates’ subsequent clinical practice and their capacity to provide equitable care, and 3) Māori student recruitment, retention and impacts on the Māori health workforce.
First, an educational environment that expresses low to moderate warmth and competence characterisations of Māori in formal instruction sites (e.g. lecture theatres) or tacitly endorses these attitudes in more informal learning sites (e.g. conversations in student study groups) is fundamentally incongruent with the (formal) Hauora Māori curriculum, a core component of health professional education programmes (Jones, 2011). One curricular objective at the University of Auckland is that all FMHS graduates will actively challenge racism (Jones, 2011). If the University’s learning spaces are complicit in the maintenance of racist ideologies, students and graduates will be less well equipped to challenge racism.
An educational environment that conveys low to moderate warmth and competence among Māori may influence future healthcare providers’ expectations and subsequent behaviours/actions during clinical encounters. Moskowitz, Stone and Childs (2012, p. 997) advise that stereotypes “arm” healthcare providers with expectations about patients and that unconscious stereotype activation has been demonstrated to influence perception, judgement, evaluation and behaviour. Harris et al.’s (2018) recent study indicates that it is yet unclear the degree to which formal and informal learning inform students’ conscious and unconscious racial bias and clinical decision making with respect to Māori, however further investigations are necessary.
Third, the University of Auckland has made commitments to increase recruitment and training of Māori health professionals (Curtis et al., 2014). The presence of negative racial stereotypes in tertiary education has a direct impact on the experiences and performance of students and faculty belonging to marginalised racial and ethnic populations (Diggs, Garrison-Wade, Estrada, & Galindo, 2009; Massey & Fischer, 2005; Mayeda, Keil, Dutton, & Ofamo¢Oni, 2014; Rankin & Reason, 2005).
B. Comparison to National Stereotype Content Study
Sibley et al. (2011) applied the SCM to the New Zealand racial and ethnic context. Sibley et al.’s (2011) results aligned with SCM-derived hypotheses. When the national study results are compared to the present study, two divergent findings are evident, indicating that student perceptions of stereotype content in the University of Auckland’s FMHS learning environments differ from the wider New Zealand context.
The SCM predicts that society’s dominant social groups are portrayed as highly warm and competent compared to traditionally marginalised populations (Fiske et al., 2002). Student perceptions of Māori warmth (as characterised in FMHS learning environments) were not significantly different from perceptions of Pākehā/NZ European warmth. When this study’s relative warmth ratings (based on perceptions of characterisations) are viewed by participant ethnicity, Māori and Pākehā/NZ European participants’ ratings of Māori and Pākehā/NZ European New Zealanders are equivalent. This indicates that Māori and Pākehā/NZ European students perceive that characterisations of Māori warmth and Pākehā warmth in their learning environments are the same. Further investigations are required before inferences or conclusions may be drawn with respect to this finding.
Participants’ comparable ratings of Māori and Pacific Nations competence characterisations are also noteworthy in view of the national study results and SCM predictions that Māori competence would be rated as higher than Pacific Nations competence (Sibley et al., 2011). This finding may be connected to frequent referrals in New Zealand health literature to ‘Māori and Pacific’ as a pair. The pairing is reiterated within the University of Auckland’s FMHS with respect to the Māori and Pacific Admission Scheme (MAPAS), the restorative justice programme initiated in the 1970s that aims to increase the Māori and Pacific Nations health workforce (Curtis et al., 2014). ‘MAPAS’ is used as an adjective on campus to describe both individuals (e.g. MAPAS coordinator) and groups (e.g. MAPAS students; The University of Auckland, 2018). While Curtis et al. (2014) clarify a historically and culturally contextualised rationale for discussing Māori and Pacific Nations peoples’ health together, an unintended consequence of the repetitive pairing may be the conflation or homogenisation of Māori and Pacific Nations peoples and priorities.
Literature pertaining to unconscious bias in health care argues that clinicians’ capacity to perceive and connect with patients as unique individuals, rather than group members, is key to combating discriminatory practices (Burgess, van Ryn, Dovidio, & Saha, 2007). A repeated conflation or homogenisation of Māori and Pacific Nations peoples, when discussing population health and racial disparities in health/health care, may be at odds with developing students’ skills for overcoming personal bias and reducing discrimination during interpersonal clinical encounters. This tension is interesting because educators delivering health equity curricula to medical and health science students state that it is important for students to understand the structural and social determinants of population health disparities (Betancourt, 2006), determinants that cause similar vulnerabilities among Māori and Pacific Nations peoples.
C. Māori Student Perspectives
Māori students were the only participant group to rate warmth and competence characterisations of their own identity group lower (on average) than members of other groups. Acute awareness among Māori students of the presence of negative attitudes in their learning environments may account for this result. This finding aligns with several articles that identify New Zealand universities as spaces with institutional norms and values that reflect the Pākehā/NZ European hegemony and marginalise Māori (Mayeda et al., 2014; Santamaría, Lee, & Harker, 2014).
V. CONCLUSION
Jones et al. (2019) articulate clear directives for medical education institutions to enact “indigenised,” decolonised, anti-racist health professional education, training and health system transformation. Developing localised knowledge of institutions’ ‘informal’ and ‘hidden’ curricula and the ways in which they function in opposition to formal Indigenous health curricula is key to developing an aligned institutional curriculum. In addition to Jones et al.’s (2019) recommendation that structured frameworks such as the Critical Reflection Tool be used to facilitate institutional reflexivity, criticality and reform, investigations into student perceptions of stereotype content could serve as an educational tool to aid students in recognising and taking responsibility for the ways in which colonisation, racism and privilege function in their educational environments.
The study’s sample size (n = 444) and response rate (71%) were strengths of the study. The cross-sectional survey design was both a strength and limitation of the study. The design’s strength lay in the anonymous questionnaire’s capacity to minimise social desirability bias while capturing a broad range of student perspectives. A limitation of the design was that data collection occurred during a distinct moment in time. Students participated in the study during the first few weeks of Semester One, 2014. If students had been surveyed following longer periods of exposure to the language and attitudes of their learning environments, the results may have been quite different. Another limitation of the study is its inability to ascertain whether students’ choices on the quantitative questionnaire items were influenced most by formal learning environments or students’ experiences in other settings.
In summary, our study demonstrated that undergraduate nursing, pharmacy, and medical students in the University of Auckland’s FMHS perceive unequal characterisations of warmth and competence across four target ethnic groups in their learning environments. Student perceptions of characterisations of Māori indicate the presence of negative stereotyping, which is incongruent with the formal Hauora Māori curriculum. Our inventory of stereotype content in health professional learning environments, as perceived by students, provides empirical evidence for important aspects of hidden/informal curricula. Future studies should attempt to identify the sources of student perceptions.
Notes on Contributors
Caitlin Harrison was a successful postgraduate student whose thesis was submitted as part of the degree of Master of Public Health at the University of Auckland, New Zealand.
Rhys Jones is a Senior Lecturer in Te Kupenga Hauora Māori (the Department of Māori Health) at the University of Auckland, New Zealand.
Marcus A. Henning is an Associate Professor in the Centre for Medical and Health Sciences Education at the University of Auckland, New Zealand.
Ethical Approval
Approval was obtained by the University of Auckland Human Participants Ethics Committee, reference number 010926.
Acknowledgements
We would like to acknowledge the University of Auckland, Faculty of Medical and Health Sciences and the study participants for making this project possible.
Funding
This is an unfunded study.
Declaration of Interest
All authors have no potential conflicts of interest.
References
Aronson, J., Burgess, D., Phelan, S. M., & Juarez, L. (2013). Unhealthy interactions: The role of stereotype threat in health disparities. American Journal of Public Health, 103(1), 50-56.
Betancourt, J. R. (2006). Eliminating racial and ethnic disparities in health care: What is the role of academic medicine? Academic Medicine, 81(9), 788-792.
Bland, J. M., & Altman, D. G. (1995). Multiple significance tests: The Bonferroni method. British Medical Journal, 310(6973), 170.
Burgess, D., van Ryn, M., Dovidio, J., & Saha, S. (2007). Reducing racial bias among health care providers: Lessons from social-cognitive psychology. Journal of General Internal Medicine, 22(6), 882-887.
Cuddy, A. J. C., Fiske, S. T., & Glick, P. (2008). Warmth and competence as universal dimensions of social perception: The stereotype content model and the BIAS map. Advances in Experimental Social Psychology, 40, 61-149.
Curtis, E., Reid, P., & Jones, R. (2014). Decolonising the academy: The process of re-presenting indigenous health in tertiary teaching and learning. Diversity in Higher Education, 15, 147-165.
Curtis, E. T., Wikaire, E., Lualua-Aati, T., Kool, B., Nepia, W., Ruka, M., … Poole, P. (2012). Tātou tātou/Success for all: Improving Māori student success. Retrieved from https://ako.ac.nz/assets/Knowledge-centre/NPF-08-002-Tatou-Tatou-Success-for-all-Improving-Maori-student-success/52178cfd54/RESEARCH-REPORT-Tatou-Tatou-Success-For-All-Improving-Maori-Student-Success.pdf
Diggs, G. A., Garrison-Wade, D. F., Estrada, D. E., & Galindo, R. (2009). Smiling faces and colored spaces: The experiences of faculty of color pursing tenure in the academy. The Urban Review, 41(4), 312-333.
Dovidio, J. F., & Fiske, S. T. (2012). Under the radar: How unexamined biases in decision-making processes in clinical interactions can contribute to health care disparities. American Journal of Public Health, 102(5), 945-952.
Field, A. P. (2005). Discovering statistics using SPSS: And sex, drugs and rock’n’roll(2nd ed.). London, England: SAGE Publications.
Fiske, S. T., Cuddy, A. J. C., Glick, P., & Xu, J. (2002). A model of (often mixed) stereotype content: Competence and warmth respectively follow from perceived status and competition. Journal of Personality and Social Psychology, 82(6), 878-902. https://doi.org/10.1037/0022-3514.82.6.878
Hafferty, F. W. (1998). Beyond curriculum reform: Confronting medicine’s hidden curriculum. Academic Medicine, 73(4), 403-407.
Harris, R., Cormack, D., Stanley, J., Curtis, E., Jones, R., & Lacey, C. (2018). Ethnic bias and clinical decision-making among New Zealand medical students: An observational study. BioMed Central Medical Education, 18(1), 18-29.
Harris, R., Cormack, D., Tobias, M., Yeh, L., Talamaivao, N., Minster, J., & Timutimu, R. (2012). The pervasive effects of racism: Experiences of racial discrimination in New Zealand over time and associations with multiple health domains. Social Science & Medicine, 74(3), 408-415.
Hill, S., Sarfati, D., Robson, B., & Blakely, T. (2013). Indigenous inequalities in cancer: What role for health care? ANZ Journal of Surgery, 83(1-2), 36-41. https://doi.org/10.1111/ans.12041
Howe, A. (2002). Professional development in undergraduate medical curricula – The key to the door of a new culture? Medical Education, 36(4), 353-359.
Jansen, P., & Jansen, D. (2013). Māori and health. In I. St George (Ed.), Cole’s medical practice in New Zealand(12th ed., pp. 52-65). Wellington, New Zealand: Medical Council of New Zealand.
Jones, R. (2011). Te Ara: A pathway to excellence in Indigenous health teaching and learning. Focus on Health Professional Education, 13(1), 23-34.
Jones, R., Crowshoe, L., Reid, P., Calam, B., Curtis, E., Green, M., … Ewen, S. (2019). Educating for indigenous health equity: An international consensus statement. Academic Medicine, 94(4), 512-519.
Jones, R., Pitama, S., Huria, T., Poole, P., McKimm, J., Pinnock, R., & Reid, P. (2010). Medical education to improve Māori health. The New Zealand Medical Journal, 123(1316), 113-122.
Massey, D. S., & Fischer, M. J. (2005). Stereotype threat and academic performance: New findings from a racially diverse sample of college freshmen. Du Bois Review: Social Science Research on Race, 2(1), 45-67.
Mayeda, D. T., Keil, M., Dutton, H. D., & Ofamo¢Oni, I. (2014). “You’ve gotta set a precedent”: Māori and Pacific voices on student success in higher education. AlterNative: An International Journal of Indigenous Peoples, 10(2), 165-179.
McCreanor, T., & Nairn, R. (2002). Tauiwi general practitioners’ explanations of Māori health: Colonial relations in primary healthcare in Aotearoa/New Zealand. Journal of Health Psychology, 7(5), 509-518.
Ministry of Health. (2015, November 13). Mortality and demographic data 2012. Retrieved from https://www.health.govt.nz/publication/mortality-and-demographic-data-2012
Moskowitz, G. B., Stone, J., & Childs, A. (2012). Implicit stereotyping and medical decisions: Unconscious stereotype activation in practitioners’ thoughts about African Americans. American Journal of Public Health, 102(5), 996-1001.
Paul, D., Ewen, S. C., & Jones, R. (2014). Cultural competence in medical education: Aligning the formal, informal and hidden curricula. Advances in Health Science Education, 19(5), 751-758.
Penney, L., Barnes, H. M., & McCreanor, T. (2011). The blame game: Constructions of Māori medical compliance.AlterNative: An International Journal of Indigenous Peoples, 7(2), 73-86. https://doi.org/10.1177/117718011100700201
Rankin, S. R., & Reason, R. D. (2005). Differing perceptions: How students of color and white students perceive campus climate for underrepresented groups. Journal of College Student Development, 46(1), 43-61.
Santamaría, L. J., Lee, J. B. J., & Harker, N. (2014). Optimising Māori academic achievement (OMAA): An indigenous-led, international, inter-institutional higher education initiative. In Māori and Pasifika higher educationhorizons (Volume 15). Emerald Group Publishing Limited, pp. 201-220. https://doi.org/10.1108/S1479-364420140000015018
Sibley, C. G., Stewart, K., Houkamau, C., Manuela, S., Perry, R., Wootton, L. W., … Asbrock, F. (2011). Ethnic group stereotypes in New Zealand. New Zealand Journal of Psychology, 40(2), 25-36.
Stats NZ Tatauranga Aotearoa. (2015, May 8). New Zealand period life tables: 2012-14. Retrieved from https://www.stats.govt.nz/information-releases/new-zealand-period-life-tables-201214
The University of Auckland. (2018). About MAPAS. Retrieved from https://www.auckland.ac.nz/en/fmhs/study-with-us/maori-and-pacific-at-the-faculty/maori-and-pacific-admission-schemes.html
van Ryn, M., Burgess, D. J., Dovidio, J. F., Phelan, S. M., Saha, S., Malat, J., … Perry, S. (2011). The impact of racism on clinician cognition, behavior, and clinical decision making. Du Bois Review: Social Science Research on Race, 8(1), 199-218.
van Ryn, M., Hardeman, R., Phelan, S. M., Burgess, D. J., Dovidio, J. F., Herrin, J., … Przedworski, J. M. (2015). Medical school experiences associated with change in implicit racial bias among 3547 students: A medical student CHANGES study report. Journal of General Internal Medicine, 30(12), 1748-1756.
Williams, D. R., & Mohammed, S. A. (2013). Racism and health II: A needed research agenda for effective interventions. American Behavioral Scientist, 57(8), 1200-1226.
Wilson, D., & Barton, P. (2012). Indigenous hospital experiences: A New Zealand case study. Journal of Clinical Nursing, 21(15-16), 2316-2326.
*Caitlin Harrison
155 North Road, St Andrews,
Bristol BS6 5AH, United Kingdom
E-mail: ctlnharrison@gmail.com
Published online: 3 September, TAPS 2019, 4(3), 79-90
DOI: https://doi.org/10.29060/TAPS.2019-4-3/OA2088
Ardi Findyartini1, Justin Bilszta2, Jayne Lysk2& Diantha Soemantri1
1Faculty of Medicine, Universitas Indonesia, Indonesia; 2Melbourne Medical School, University of Melbourne, Australia
Abstract
Introduction: Transnational faculty development initiatives (FDIs) constitute a strategy to improve the quality of the teaching staff in medical schools. This study evaluates feedback from participants of an FDI designed as part of a collaborative transnational partnership between researchers of an Australian and an Indonesian medical school.
Methods: The FDI was a three-day program that explored four major topics: effective clinical teaching, methods of teaching and supervising in clinical settings, assessment of clinical learners and clinical education in practice. These topics were identified through comprehensive needs analysis and curriculum blueprinting exercises. Each participant (n= 27) submitted one piece of reflective writing and one critical appraisal or teaching/assessment assignment on each topic. Using a thematic analysis approach, two researchers independently reviewed each participant’s written assignments to identify emerging themes.
Results: Five core themes were identified. Most revolved around the benefits of the training, especially the learning issues that the participants identified during the FDI and how they could be applied to their local contexts. Additional themes covered participants’ views on the delivery of the FDI and cross-cultural implications. Peer observation of teaching, qualitative assessment and feedback provision were also significant issues raised by the participants.
Conclusions: This study presents important lessons for cross-cultural adaptation of best practices in the development and delivery of transnational FDIs.
Keywords: Faculty Development, Transnational, Collaboration, Cross-cultural, Clinical Teacher
Practice Highlights
- Cross-cultural factors need to be considered when developing transnational collaborative FDIs.
- Methods of delivery in transnational FDIs should be interactive, collaborative and allow participants’ active engagement and participation.
- Transnational collaborative FDIs enrich participants’ contextual understanding of best teaching practices.
I. INTRODUCTION
Faculty development initiatives (FDIs) refer to any systematic process(es) launched by an educational institution to develop the capabilities and capacities of their staff in all areas of their role: teaching, education, research and scholarship, and leadership (Steinert, 2014). FDIs can be informal or formal learning opportunities and can involve individuals and/or groups of academic staff. All forms of FDI are deemed vital, and the approach can be tailored according to institutional and/or individual needs (Steinert, 2010, 2011, 2014).
Clinical teachers are expected to possess adequate and up-to-date medical knowledge and clinical skills, develop positive relationships with students, foster supportive learning environments, practice good communication skills and show enthusiasm (Sutkin, Wagner, Harris, & Schiffer, 2008). Good clinical teachers should provide sufficient support, allow students to think for themselves, provide feedback that stimulates reflection and identify areas of improvement or development (Kikukawa et al., 2013). A systematic review by Steinert et al. (2016) on FDIs highlighted the importance of training clinical teachers in many settings. Although most institutions agree on the attributes of good clinical teachers, different institutions have different priorities. For example, Kikukawa et al. (2013) explained that medical knowledge and clinical skills attributes are less emphasised for clinical teachers in Japan than those in a western setting.
Much research has been undertaken on the development and implementation of the education curricula for transnational medical and health professions (e.g. Castelo-Branco et al., 2016; Waterval, Frambach, Driessen, Muijtjens, & Scherpbier, 2018) and FDIs (Burdick, Amaral, Campos, & Norcini, 2011; Burdick et al., 2010; Yoon et al., 2016). These studies have identified interesting aspects such as the relevance of FDI content, the variation in teaching and learning expectations and methods and the appropriateness of the FDI design given participants’ needs, culture and context (Steinert et al., 2016). Scholars have confirmed that it is critical to consider cross-cultural and contextual issues when conducting FDIs and for translating the lessons learned into practice (Altbach, 2013, Chapter 24; Hodges, Maniate, Martimianakis, Alsuwaidan, & Segouin, 2009).
In 2015, a formal collaboration (Partnerships in Clinical Education) was established between the Faculty of Medicine, Universitas Indonesia (FMUI) and the University of Melbourne (UoM) Medical School’s Excellence in Clinical Teaching (EXCITE) programme; it is described elsewhere (see Bilszta, Lysk, Findyartini, & Soemantri, in press). One of the outcomes of this collaboration was the development of a high-quality FDI for clinical teachers from FMUI. Further, this new FDI was delivered to a group of invited clinical teachers so that experienced facilitators could observe the process and model the delivery of the new academic content along the same lines.
While FDIs in various and pertinent forms are necessary for clinical teachers, transnational collaboration in developing and conducting FDIs (as reported in the present study) is expected to strengthen the contextual best practices of such programmes. However, previous studies on transnational FDIs (e.g. Burdick et al., 2011; Burdick et al., 2010; Yoon et al., 2016) have not explored the cultural issues in clinical education or in FDI methods despite arguments that favour adapting globalised practices in medical education to the local culture and context (Gosselin, Norris, & Ho, 2015). The aim of this study, therefore, is to evaluate the experiences of the clinical education leaders who completed a transnational FDI and identify the relevant cross-cultural issues in the content of the FDI and its delivery method. Accordingly, in the current study, the participants were asked to reflect on their teaching skills during the training and explore whether certain teaching approaches in clinical education could be translated into their settings. In discussing best practices of clinical education, the participants were encouraged to consider potential cultural issues that might influence the implementation of the FDI. The results of this study are expected to add to the understanding of collaborative clinical teacher FDIs.
II. METHODS
A. Context
A long-standing relationship between UoM and FMUI and the need for FMUI to advance the skills and professionalism of its clinical teachers led to this partnership in clinical education. The collaborative FDI project began with a needs-analysis exercise and the development of a training curriculum blueprint, as described by Bilszta et al. (in press). The needs analysis and curriculum blueprinting resulted in the identification of four major topics: effective clinical teaching, methods of teaching and supervising in clinical settings, assessment of clinical learners and clinical education in practice.
The resultant FDI was delivered via a workshop, titled the 1st Advanced Clinical Teacher Training and Training on Trainers Workshop, to a group of invited clinical education leaders. Short interactive lectures, small group discussions based on a collaborative learning approach, role-plays (for peer observation of teaching [PoT]) and individual and group reflections were conducted during the 3-day workshop in Jakarta in November 2016. The workshop was facilitated by the EXCITE teaching staff in collaboration with local medical education experts. The workshop schedule is described in Table 1. Twenty-seven FMUI clinical teachers (9 male, 18 female; 8 from surgery and 19 from medicine) participated in the workshop. These participants were invited because they had already completed a basic clinical teacher course (CTC) delivered by the FMUI and had served as instructors/tutors or resource persons in the CTC. Despite the small sample of clinical teachers involved, the distribution of the sample was representative in terms of gender and department of origin (medicine and surgery). These participants were selectively invited because they had been identified as possible education leaders.
B. Data Collection
On completion of the workshop, each participant was required to submit eight written assignments through an e-learning platform. Participants were asked to submit two assignments on each of the four major topics: one in-class assignment and one out-of-class assignment (Instructions for each assignment are given in Figures 1 and 2). For the in-class assignment, participants were asked to reflect on the topics being discussed (i.e. what new insights and awareness did they gain from the session; what questions triggered these learnings; how can they use the information to improve their own lesson plans and quality of teaching). For the out-of-class assignment, participants were required to either develop a critical appraisal of a journal article relevant to the topic or develop a learning or assessment activity.
C. Data Analysis
In line with the objectives of the study, participants’ assignments were reviewed not only to detect the cross-cultural issues identified by the participants but also to examine the lessons they learned about teaching, assessment practices and their contextual application. A thematic analysis approach was used to synthesise the qualitative data (Patton, 2002). Each assignment was anonymised so that the reviewers could not identify to whom the assignment belonged. Two of the authors (DS and AF) reviewed the assignments to identify specific patterns and generate a coding system. The codes were translated into appropriate subthemes and grouped into relevant themes. To capture the significance of each theme, the number of mentions of each theme was counted.
DS and AF are medical education experts from Indonesia and have been involved in the FMUI CTC for the past 10 years. Indonesia, in general, is considered to have a hierarchical culture in which the opinions or thoughts of seniors or experts are highly valued. Further, it has been a collectivist culture in which relationships with others and maintaining harmony within the group is considered critical (Hofstede, 2001). In FMUI and its teaching hospitals, where the clinical teachers and the authors work, this culture is, to some extent, still reflected in daily practice. The authors were aware of this ‘lens’ as they reviewed the participants’ assignments in this study.
| Day 1 | ||
| Session 1 – Effective clinical teaching | ||
| 15 minutes | Ice breaker | Organiser |
| 30 minutes | Interactive lecture 1: Various principles of teaching and learning in a clinical setting | Resource person 1 (UoM) |
| 60 minutes | Group discussion 1: Reflection on various principles of teaching and learning in a clinical setting | Tutors (UoM and FMUI) |
| 60 minutes | Plenary: Various principles of teaching and learning in a clinical setting | Resource person (UoM) |
| Session 2 – Methods of teaching and supervising in clinical settings (the clinical supervisor) | ||
| 30 minutes | Interactive lecture 2: Supervising students in clinical practice | Resource person 2 (UoM) |
| 60 minutes | Group discussion 2: Students’ supervision and mentoring | Tutors (UoM and FMUI) |
| 30 minutes | Closing of day 1 | |
| Day 2 | ||
| Session 3 – Clinical education in practice (peer observation & peer assessment) | ||
| 30 minutes | Interactive lecture 3: Principles of peer observation and the use of peer feedback | Resource person 1 (UoM) |
| 60 minutes | Group discussion 3: Role-play (peer observation and peer feedback) | Tutors (UoM and FMUI) |
| 60 minutes | Group discussion 4: Peer assessment plan, training module development | Tutors (UoM and FMUI) |
| Session 4 – Methods of teaching and supervising in clinical settings (assessing clinical learners) | ||
| 60 minutes | Interactive lecture 4: Principles of competency-based assessment | Resource person 3 (UoM) |
| 60 minutes | Group discussion 5: Appraisal of various assessment instruments | Tutors (UoM and FMUI) |
| 60 minutes | Plenary: Competency-based assessments and various assessment instruments | Resource person 3 (UoM) |
| Day 3 | ||
| Session 5 – Clinical education in practice (peer observation & peer assessment) | ||
| 60 minutes | Group discussion 6: Item development and review (MCQ and OSCE) | Tutors (UoM and FMUI) |
| 60 minutes | Group discussion 7: Assessors’ standard setting (using video) | Tutors (UoM and FMUI) |
| 60 minutes | Plenary: Workplace-based assessment | Resource person 3 (UoM) |
| Session 6 – Reflection and action plan | ||
| 60 minutes | Group discussion 8: Reflection and action plan on the topics being discussed | Tutors (UoM and FMUI) |
| 60 minutes | Plenary: Reflection and action plan on the topics being discussed | Tutors (UoM and FMUI) |
| 60 minutes | Closing and explanation of assignment | Organiser |
Table 1. The 3-day workshop programme
| In-class assessment:
For each topic area, participants are required to generate ‘artefacts’ that have been developed during the interactive lecture or group discussions, and this can include social media posts (e.g. Facebook, Snapchat or Twitter). Using these artefacts, participants must reflect on the key learnings from each topic area and how they will use these to modify/develop their clinical teaching practice. EXAMPLE: As a group, participants might develop agreed criteria to define effective clinical supervision. Using the agreed criteria to define effective clinical supervision, a participant may comment/reflect on how they might apply these criteria to their own supervisory practice. EXAMPLE: Each participant generates an MCQ and gets feedback from a colleague about the question and response options. Using this MCQ, a participant may comment/reflect on the development of their question and justify any changes made. EXAMPLE: On completion of the microteaching session, a participant could take a photo which represents what they learnt from completing this activity, post this to Facebook or Snapchat and comment on how they might use this activity in their work place. EXAMPLE: A participant might develop an action plan outlining how they intend to collect peer feedback on a teaching and learning activity they deliver regularly and reflect on the areas within their teaching they want feedback on and why they want feedback in these areas. EXAMPLE: A participant might comment/reflect on Facebook or Snapchat post made by a colleague about an activity completed during one of the teaching sessions. Time will be provided at the end of each interactive lecture and group discussion for the development of these reflections. Reflection prompts will include the following questions: · What new insights or awareness arose for me in this session · What questions or puzzlements did this session trigger for me? · How can we use this information to improve/critique own practice? · How can we use this information to scale up the quality of teaching? · How can we use this information to understand or to direct our own lesson planning and design? |
Figure 1. Instruction for in-class assignment
| Out-of-class assessment:
Each participant is expected to: · Effective clinical teaching o Appraise and develop at least 500 – 1000 words summary based on at least 1 article discussing about effective teaching methods in clinical setting (the article is published in the past 5 years). The appraisal should be concluded by why and how the participant would implement the method in his/her setting. (The topic can be on undergraduate and postgraduate clinical education and according to clinical setting in which the participant has been involved). · Effective clinical supervision o Develop a summary of participant’s experience in dealing with struggling students and how the participant will supervise and mentor the student(s). The participant should reflect on how he/she would supervise and mentor the student: the strengths, the weaknesses and actions for improvement. The participant should add at least 1 reference (published within 5 years) to support the reflection. · Principles of clinical assessment Participant may choose one of the following assignment for this topic: o Appraise and develop at least 500 – 1000 words summary based on at least 1 article discussing assessment in a clinical setting (the article is published in the past 5 years). The appraisal should be concluded by why and how the participant would implement the method in his/her setting. o Develop 1 rubric of assessment explaining aspects/criteria to be assessed, the description of each aspect/criterion, and the scoring and its description. Please elaborate the justification (around 500 words) that the instrument developed by the participant has fulfilled principles and relevant criteria for each assessment method. Relevant reference(s) can be used to support the justification. o Develop 3 MCQs fulfilling criteria of good MCQs or 1 station OSCE and its scoring sheet. Please elaborate the justification (around 500 words) that the instrument developed by the participant has fulfilled principles and relevant criteria for each assessment method. Relevant reference(s) can be used to support the justification. · Clinical education in practice: peer observation and peer assessment o Record his/her teaching session at the clinical setting. The participant will need to reflect on his/her teaching and seek feedback from the paired participant where possible. |
Figure 2. Instruction for out-of-class assignment
III. RESULTS
The following five core themes, each with its own subthemes, were identified from the thematic analysis: lessons learned and teaching beliefs in relation to clinical teaching; cross-cultural issues in collaborative FDI; contextual education practice; methods of delivery used in the FDI; and cultural issues in supervision of clinical practice (see Table 2). Both reviewers reached consensus on the themes in one iteration of analysis. Minor disagreements in coding were resolved through discussion.
| Theme | Subtheme | Number of comments for each theme |
| Lessons learned and teaching beliefs in relation to clinical teaching | 82 | |
| Assessment for learning and of learning | ||
| Feedback in clinical supervision | ||
| Effective clinical teaching | ||
| Successful PoT | ||
| Importance of valid and reliable assessment | ||
| Cross-cultural issues in collaborative FDI | 15 | |
| Cross-cultural application of teaching and assessment approaches | ||
| Hierarchical barriers in cross-cultural application of PoT | ||
| Language limitations in cross-cultural FDI | ||
| Contextual education practice | 15 | |
| Lack of feedback culture | ||
| Limited ability to provide specific qualitative data in assessment | ||
| Contextual application of teaching and assessment methods | ||
| Cultural issues in supervision of clinical practice | 5 | |
| Influences of cultural issues in clinical practice on teaching | ||
| Teaching cultural issues in the clinical setting | ||
| Methods of delivery used in the FDI | 8 | |
| Peer discussion within collaborative learning | ||
| Role-playing through micro-teaching activity |
Table 2. List of themes and subthemes identified
A. Lessons Learned and Teaching Beliefs in Relation to Clinical Teaching
Participants indicated that they benefited from the training in many ways, and they mentioned the lessons learned in their assignments. More than half of the subthemes fell under this category. The subthemes ranged from effective clinical teaching to the importance of valid and reliable assessment.
This core theme had four main subthemes, and participants identified the important lessons learned under each subtheme. For example, under the subtheme of successful PoT, participants reflected on the importance of self-reflection, a partnership between the observer and the observe, and a supportive, respectful environment.
“From peer observation, the clinical teacher can reflect their teaching, set a clearer learning goals for the student, could improve their own teaching skills after peer feedback and repeated observation.”
(IC-PO-06)
“I learned that peer observation is quite a complex process, involving partnership and trust among the observer and observee; the judgement was based on a set of agreed criteria.”
(IC-PO-09)
On the subtheme of assessment, participants reported a growth in their understanding of assessment purposes, especially the difference between assessment for learning and assessment of learning. The FDI also increased their awareness of the importance of valid and reliable assessment.
“We also learnt that assessment consisted of assessment for learning (formative) where there is rich of feedback and assessment of learning (summative) that is characterised of limited feedback.”
(IC-Ass-08)
“From my experience with the OSCE in psychiatric clinical skills, we have developed the checklist but in my opinion it still difficult to make it objective… I learn from the session, that we could improve the objectivity by listing the behaviour that we want to observe.”
(IC-Ass-15)
The importance of student-centred feedback was a frequently cited subtheme in the lessons learned in relation to clinical supervision. On the subtheme of effective clinical teaching, participants discussed some influencing factors such as understanding the learning process, understanding medical teachers’ competencies as well as students’ background, and the importance of preparation before teaching.
“Teaching is facilitating students’ construction of knowledge… The teacher is responsible for recalling prior information as the foundation of learning and give feedback to refine the knowledge that has been constructed.”
(CT-I-03)
“The ideal educators should have competent medical/clinical knowledge, capable of clinical and technical skills competence, conducting clinical reasoning, having positive relationships with students and supportive learning environment, communication skills and enthusiasm.”
(CT-I-15)
“In every teaching process in the clinical setting, the target of teaching and competencies to be achieved need to be determined first, also the teaching methods should be adjusted according to the limited time available…”
(CT-I-10)
B. Cross-cultural Issues in Collaborative FDI
Interestingly, though the assignment instructions did not ask participants to comment specifically on cross-cultural issues, these issues were still raised. An example of a cross-cultural issue that was identified pertained to language. It is summarised in the following comment.
“[When we have to mark a Melbourne medical student in a video conducting history taking], for us as the Indonesian teachers, [we] thought that the clinical reasoning and the communication of the Melbourne student is already good or excellent. Maybe this is because we, Indonesian, are not English native speaker…”
(IC-Ass-16)
The other cross-cultural issue was related to the application of certain concepts or practices of teacher development. Questions were raised about transposing activities from an Australian context directly into an Indonesian context. Most comments under this theme discussed whether PoT, which is regularly exercised in Australia, was suitable for Indonesia. PoT has been defined as a means to assure the quality of teaching and learning process in higher education which involves teachers as observers who provide feedback to their peer teachers on teaching and learning practice (Hammersley-Fletcher & Orsmond, 2004; Shortland, 2004). Some of the identified barriers were hierarchical; that is, the participants noted that because of the cultural boundaries between the senior and junior staff, providing feedback to someone older may be seen as impolite or unusual.
“At the beginning, I thought this practice would be very difficult in the implementation, since it is not so commonly used in our institution and even we are quite afraid to comment on our colleague’s style of teaching. I was thinking it may lead to a feeling of being evaluated or judged and it may not so comfortable for certain people, in particular for colleagues who are more superior (senior).”
(IC-PO-14)
“The Indonesian culture does not seem to allow teaching staff to critique each other… Critique, or more precisely, feedback is commonly misinterpreted as an ‘insult’ and can result in lack of harmony between each member of staff.”
(IC-PO-23)
Cross-cultural issues seemed to influence not only PoT but also the models of teaching and assessing students’ performance. One participant highlighted the differences in scoring between the FMUI clinical teacher and one from UoM’s in the following words.
“Our group during the session discussed the difference of the scores given for the student. I was more stringent in giving the score, although at the end I knew that my scoring was more in line with the standards of Melbourne Medical School for students at that particular level…”
(IC-Ass-04)
C. Contextual Education Practice
While the participants learned many lessons, they had questions about how the theory and concepts learned could be applied in real educational settings, specifically in Indonesia. Contextual issues were identified in the application of teaching and assessment methods appropriate to an Indonesian setting.
“I think those theories need to be understood contextually. I also think that the most important thing is to be able to implement them adaptively according to teaching learning situations.”
(CT-I-01)
“This is a significant challenge for Faculty of Medicine Universitas Indonesia in implementing programmatic assessment, since the school has limited number of available faculty members.”
(OC-Ass-04)
Applying theory, concepts or best practices from Australia called for careful consideration of the local context and cultural issues in an Indonesian clinical setting. Participants also acknowledged the lack of feedback culture in their institution and their inability to provide qualitative data during assessment.
“Most assessments rely on numbers… The greater challenge, I think, would [be]… in encouraging the clinical teachers to write down their comments or feedback on the evaluation sheet. Our experience with the use of Mini-CEX (Mini Clinical Evaluation Exercise) shows that most assessors would only provide general feedback such as ‘excellent’, ‘good’ or ‘needs further improvement’ without further written deliberation on the Mini-CEX form due to time constraints.”
(OC-Ass-01)
D. Cultural Issues in Supervision of Clinical Practice
Certain culture issues in the clinical practice environment influence how teaching and supervision are delivered. Clinical teachers should be aware of such matters in order to provide targeted teaching and feedback. Further, clinical teachers should teach or stimulate discussions on the sociocultural aspects of patient problems.
“In sexual transmitted infection clinic… students are often uncomfortable examining patients… During clinical supervision, this condition can be ‘read’ by the clinical supervisor. This situation becomes material for feedback from teachers to students. Some students do not like these patients because they consider high-risk sexual behaviour as intolerable sin.”
(CS-I-25)
“For example, in the discussion, the patient and partner sexual behaviours will be discussed. How can the student maintain confidentiality of the patient’s disease, when [at the same time] the student has to treat patient’s sexual partner too?”
(OC-Ass-08)
E. Methods of Delivery Used in the FDI
A major focus for the FDI participants was observing the delivery of FDI content by experienced facilitators in order to model their delivery process. The methods used in delivering the materials included approaches such as collaborative learning, role-playing and micro-teaching. The participants found those approaches to enhance their learning; moreover, the approaches also encouraged the participants to engage in peer discussion and visualise the application of training materials in real situations of teaching. Participants felt that they may apply the delivery methods used in the FDI when teaching medical students.
“This micro-teaching activity gave the real situation on how we should prepare in a short time for teaching effectively: plan-teach (in short time)-feedback-debrief and reflect.”
(CT-I-07)
“We were given a group work in the form of jigsaw activity. The materials delivered through collaborative methods encouraged us to learn together and share with each other. A very useful method to train ourselves in giving opinions, although they may differ, they can be collated or formulated to reach a consensus.”
(IC-PO-05)
IV. DISCUSSION
This present study aims to evaluate the experiences of the clinical education leaders who completed the transnational FDI between FMUI and UoM. A thematic analysis of the written reflections by the FDI participants highlighted five key themes: lessons learned and teaching beliefs in relation to clinical teaching, cross-cultural issues in collaborative FDI, contextual education practice, methods of delivery used in the FDI and cultural issues in supervision of clinical practice.
According to the faculty development model, the FMUI-UoM FDI training program can be categorised as a formal programme involving workshops and reflections on the participants’ experience (Steinert, 2010, 2011, 2014). The development and implementation of the FDI was based on comprehensive needs analysis and curriculum blueprinting activities, which ensured the appropriateness of the content and the teaching methods. Such needs analysis is deemed necessary to ensure congruence between the content and mode of delivery in the FDI programmes, on the one hand, and the needs of clinical teachers, on the other hand, who generally tend to be very busy and work in either community-based or hospital-based settings (Behar-Horenstein, Garvan, Catalanotto, & Hudson-Vassel, 2014; Damp et al., 2016; Houston et al., 2004).
The participants of this study identified many relevant lessons from each of the four FDI topics. While describing the lessons learned in their written assignments, they also explored their teaching beliefs, particularly in relation to the materials delivered in the FDI. Teaching beliefs are known to significantly influence teachers’ behaviour in the classroom (Samuelowicz & Bain, 2001; Taylor, 2003). Reflecting on their teaching beliefs is also known to help clinical teachers understand the information discussed in the training program and contextualise it according to the levels of experience and competence of the students and the clinical practice context (Taylor, Tisdell, & Gusic, 2007).
The participants of the FDI appreciated the variety of the delivery methods used. They also noted that delivery methods such as collaborative learning and micro-teaching were used appropriately, and they contributed to enhancing their learning and positive attitude towards peer discussion. It is likely that the participants could relate more with these methods because they have been already implemented in the clinical teacher training at FMUI. As programme developers, the present authors were aware of the importance of engaging participants in the training as much as possible. Since this was an advanced training programme in which participants were expected to share their deeper understanding of the given topics, collaborative learning and peer discussion were used. These methods are known to strengthen the experiential learning process and initiate the development of a community of practice among participants (Steinert, 2010). Peer discussion during the training also enabled group reflection, which is acknowledged as a critical process for clinical teachers seeking to actively improve their teaching (van Lierop, de Jonge, Metsemakers, & Dolmans, 2018).
While findings on teaching beliefs and methods of delivery in FDI have been reported extensively, the other three themes – cross-cultural issues in conducting FDI, contextual education practice and cultural issues pertinent to supervision in clinical education – represent the salient factors of this study, which highlight the importance of cultural awareness in collaborative FDI. When discussing cross-cultural issues in conducting FDI, participants pointed to the language issues in the training. Nonetheless, they still found the training to be engaging and relevant to their needs. Collaborative teacher training involving resource persons and participants from different countries should seriously consider and address the language problem (Yoon et al., 2016). Other related issues found in this study pertained to communication and the cultural competence of resource persons and participants in the FDI programme. Interaction between resource persons and participants and among participants from different cultural backgrounds calls for an understanding of how important messages in an FDI can be delivered, discussed and received. For example, Slootweg et al. (2016) found that some cultural factors may influence how clinical teachers speak up in team meetings in a postgraduate training setting. They noted that meetings can be more fruitful if they have clear aims, a flexible structure and a positive environment to express ideas and provide feedback (Slootweg et al., 2016). These suggestions are also relevant to the FDI environment in which participants may need to ask questions and express ideas openly, and resource persons may need to identify and discuss certain ideas further. Given the hierarchical and collectivist culture in Indonesia (Hofstede, 2001), promoting such interactions during FDIs is an important mechanism, whereby resource persons (considered the experts with ‘power’) can encourage open discussions, and participants can freely present their views, without being judged by other fellow participants. To facilitate the process, in this study, the FDI was deliberately designed to include local medical education experts. They were exposed to various methods of learning, which enabled them to revisit their understanding, ask questions and share arguments in a friendly and positive environment.
Peer-teaching observation was viewed as a new concept by most participants in the training. The FDI participants highlighted that implementing PoT in an Indonesian setting could be a challenge. PoT can be broadly categorised into three models: evaluation, developmental and peer-review (Gosling, 2002). When PoT is used as part of a teaching audit, a teacher as the observer and the observee may feel threatened. On the other hand, a more friendly and constructive process occurs when PoT focuses on teachers’ development. The development model of PoT (i.e. teaching-observation-reflection-feedback), involving peer teachers and education experts, is reported to increase critical reflection and applied feedback among the teachers involved, which are highly relevant to improving the quality of teaching practice (Yiend, Weller, & Kinchin, 2014). Sullivan, Buckle, Nicky and Atkinson (2012) noted that positive feedback from clinical teachers involved in PoT in an undergraduate paediatric teaching was viewed as non-threatening and valuable for promoting insights and reflection.
In the present study, PoT was considered an evaluative process by the participants. They noted that providing feedback especially to senior colleagues could be very challenging given the hierarchical culture in Indonesia. The authors of this study suggest that the implementation of PoT in an Indonesian clinical education setting should aim to support the development of fellow clinical teachers’ teaching quality instead of evaluating their performance. This is in line with the best practices of PoT, which aim at supporting the effective development of teachers by encouraging reflection on teaching and a conceptual understanding of teaching in various settings (Bell & Mladenovic, 2015). Both senior and junior colleagues engaged in an FDI can agree on the agenda of development and accordingly build an action plan after the observation. This will help strike a balance between collegiality and the autonomy of teachers (Bell & Thomson, 2018). In addition, senior colleagues can be involved as role models and champions in conducting the PoT focused on teaching development. This way, the best practices of PoT may be implemented while still respecting the local culture.
Another important lesson learned by the participants was on the implementation of clinical assessment. Participants of the FDI understood the principles of assessment and the various methods of clinical assessment (Epstein & Hundert, 2002). They also learned that clinical assessment requires observation, and the purpose of assessment can be both formative and summative. They also realised, however, that the current clinical setting is often challenging, and clinical teachers do not always have the time to observe students and provide feedback. These are actually global challenges of clinical education (Ramani & Leinster, 2008). Most participants of the FDI felt that the feedback culture had not been effectively integrated into clinical training. A study by Suhoyo et al. (2017) underlined the hierarchical or power distance (Hofstede, 2001) issues in a clinical setting where students value feedback from the experts, but seeking feedback is not considered the common practice. In cultures marked by hierarchy, high uncertainty avoidance and collectivism, as in Indonesia (Hofstede, 2001), feedback is usually sought indirectly from peers or subordinates to avoid embarrassment (de Luque & Sommer, 2000). This FDI has addressed this issue and equipped the clinical teachers for providing constructive feedback to the students. Considering the cultural context in Indonesia and busy clinical settings, clinical teachers as experts in their area should be allowed by the system (i.e. healthcare and clinical education systems) to have formal multiple, short, valid observations of student performance at the workplace before providing constructive feedback to students. Similarly, students’ feedback-seeking behaviour can be encouraged by creating a safe environment that fosters a reciprocal relationship between the students and credible clinical teachers. In such an environment, both positive and negative feedback will be considered constructive to the students’ development (Oktaria & Soemantri, 2018).
The participants of the FDI also reported that providing qualitative data during an assessment posed a challenge. Since assessments can be formative in nature, detailed narratives on the student’s performance quality may actually help clinical teachers and students identify and document the gap in skill and the actions for future improvement (Hanson, Rosenberg, & Lane, 2013). Such qualitative assessment calls for the articulation of the performance of individual students and judgement expertise on the part of the assessor (van der Vleuten et al., 2012). In addition, to ensure rigour in judgement, the assessor should conduct valid observations of student performance over multiple occasions (Cook, Ayelet, Hatala, & Ghinsburg, 2016). This study revealed that most clinical assessments still relied on numbers and that the written feedback provided in workplace-based assessment forms (e.g. Mini-CEXs) was generic. Such feedback failed to indicate the aspects that are necessary for a student’s future improvement. The present authors argue that the lack of ability to provide qualitative assessment data, in addition to other factors such as poor feedback provision skills, a weak clinical education system and low quality of observation, may also be explained by one of the cultural dimensions: the tendency of uncertainty avoidance (Hofstede, 2001). Clinical educators may be wary of proving individualised feedback because narratives or qualitative comments cannot be standardised.
Finally, while exploring concepts in clinical teaching, clinical supervision, clinical assessment and PoT, the participants discussed how the translation of these aspects into teaching practice in an Indonesian setting should depend on the local context. Some participants noted how cultural issues in a clinical practice environment, such as interactions with patients about special conditions (e.g. sexually transmitted diseases), highlight the need for a contextualised approach. This presents an interesting point because clinical practice and the educational environment depend on the health and education systems, the cultural and social norms and the public needs in a certain country (Altbach, 2013, Chapter 24; Hodges et al., 2009). Cultural issues can be woven into the FDI content, and clinical educators can translate best practices into the local context in two ways: (1) by reflecting on the current clinical education environment, expected outcomes, and students’ characteristics and (2) by considering the healthcare system and the patients’ characteristics. Ideally, clinical educators should be aware of the cultural diversity influencing their relationships with the students, patients and healthcare environment and should be able to adjust their mentoring and supervision approaches accordingly (Wong, Wong, & Ishiyama, 2013).
Best practices in medical education should attempt to balance the influence of globalisation and local culture. As suggested by Gosselin et al. (2015), highlighting cultural distinctions, addressing local needs and contexts and presenting local case studies and innovations are needed to contextualise the best practices. This also applies in the current collaborative FDI where attempts to enhance the quality and meet global standards have been accompanied by the incorporation of local values and wisdom. These attempts were beneficial because the participants succeeded not only in grasping the main concepts and best practices of the clinical teaching shared by the Australian research team but also in considering the local cultural context while applying them. Learning can thus become more contextual and relevant, and this in turn can enhance the value of such training.
The limitations of the present study are as follows. First, the participants involved in the study were few and from the same institution. However, they belonged to different clinical departments and had experience in teaching and learning in clinical settings. This allowed for a better contextual understanding and richer perspectives on the FDI topics. Second, the participants were selected from those who had already completed basic clinical teacher training. Therefore, their active engagement in the various FDI activities reflected their desire to challenge their ideas about teaching and learning and explore new approaches to their teaching behaviour. Given the aim of the study, this active engagement was beneficial because they could explore the lessons learned while still considering the best practices and contextual implementation.
V. CONCLUSION
The findings of this study highlight the several important considerations for developing and delivering an FDI designed as part of a collaborative transnational partnership. These include the methods for delivering the teaching and learning activities, participants’ interaction with the ideas and concepts introduced and the application of new knowledge and teaching behaviours in the participants’ own clinical environment. FDI developers should be aware of the interaction of these elements to promote cross-cultural adaptation of best practices in faculty development in general and in clinical teacher training in particular.
Notes on Contributors
Dr Ardi Findyartini is a Senior Lecturer in Medical Education and currently the Head of Department of Medical Education and Head of Medical Education Unit, Faculty of Medicine, Universitas Indonesia.
Dr Justin Bilszta is a Senior Lecturer in Medical Education, Department of Medical Education, Melbourne Medical School University of Melbourne.
Dr Jayne Lysk is a Lecturer in Clinical Education, Department of Medical Education, Melbourne Medical School University of Melbourne.
Dr Diantha Soemantri is a Senior Lecturer in the Department of Medical Education, currently the Vice Director, Medical Education of the Indonesian Medical Education and Research Institute (IMERI), Faculty of Medicine, Universitas Indonesia.
Ethical Approval
This research was approved by the FMUI Research Ethics Committee (Number 0720/UN2.F1/ETIK/2018).
Acknowledgements
The authors would like to thank all Advanced Clinical Teacher Training participants at the Faculty of Medicine, Universitas Indonesia. The authors would like to also thank the Faculty of Medicine, Universitas Indonesia and the Department of Medical Education, Melbourne Medical School, University of Melbourne for supporting this collaboration.
We would like to thank Editage (www.editage.jp) for English language editing.
Funding
This project was supported by the Commonwealth of Australia through the Australia-Indonesia Institute of the Department of Foreign Affairs and Trade (Application No: AII00004 of AII Grant Round 1 2014). Generous in-kind support was provided by Faculty of Medicine, Universitas Indonesia and the Department of Medical Education, Melbourne Medical School, University of Melbourne.
Declaration of Interest
The authors declare that they have no conflict of interest.
References
Altbach, P. (2013). The international imperative in higher education. Rotterdam, The Netherlands: Sense Publishers.
Behar-Horenstein, L. S., Garvan, C. W., Catalanotto, F. A., & Hudson-Vassel, C. N. (2014). The role of needs assessment for faculty development initiatives. The Journal of Faculty Development, 28(2), 75-86.
Bell, A., & Mladenovic, R. (2015). Situated learning, reflective practice and conceptual expansion: Effective peer observation for tutor development. Teaching in Higher Education, 20(1), 24-36. https://doi.org/10.1080/13562517.2014.945163
Bell, A., & Thomson, K. (2018). Supporting peer observation of teaching: Collegiality, conversations, and autonomy. Innovations in Education and Teaching International, 55(3), 276-284. https://doi.org/10.1080/14703297.2016.1212725
Bilszta, J., Lysk, J., Findyartini, A., & Soemantri, D. (in press). Establishing and sustaining transnational clinical teacher faculty development initiative. The Asia Pacific Scholar.
Burdick, W. P., Amaral, E., Campos, H., & Norcini, J. J. (2011). A model for linkage between health professions education and health: FAIMER international faculty development initiatives. Medical Teacher, 33(8), 632-637. https://doi.org/10.3109/0142159X.2011.590250
Burdick, W. P., Diserens, D., Friedman, S. R., Morahan, P. S., Kalishman, S., Eklund, M. A., … Norcini, J. J. (2010). Measuring the effects of an international health profession’s faculty development fellowship: The FAIMER Institute. Medical Teacher, 32(5), 414-421. https://doi.org/10.3109/01421590903394587
Castelo-Branco, L., Finucane, P., Marvão, P., McCrorie, P., Ponte, J., & Worley, P. (2016). Global sharing, local innovation: Four schools, four countries, one curriculum. Medical Teacher, 38(12), 1204-1208. https://doi.org/10.1080/0142159X.2016.1181731
Cook, D. A., Ayelet, K., Hatala, R., & Ghinsburg, S. (2016). When assessment data are words: Validity evidence for qualitative educational assessment. Academic Medicine, 91(10), 1359-1369. https://doi.org/10.1097/ACM.0000000000001175
Damp, J. B., Dewey, C. M., Wells, Q., Horn, I., Kroop, S. F., & Mendes, L. (2016). Faculty development on clinical teaching skills: An effective model for the busy clinician. Journal of Medical Education and Curricular Development, 3, 187-191.https://doi.org/10.4137/JMECD.S40798
de Luque, M. F. S., & Sommer, S. M. (2000). The impact of culture on feedback-seeking behavior: An integrated model and propositions. Academy of Management Review, 25(4), 829-849. https://doi.org/10.2307/259209
Epstein, R. M., & Hundert, E. M. (2002). Defining and assessing professional competence. JAMA, 287(2), 226-235.
Gosling, D. (2002). Models of peer observation of teaching. Retrieved from
https://www.researchgate.net/profile/David_Gosling/publication/267687499_Models_of_Peer_Observation_of_Teach
ing/links/545b64810cf249070a7955d3.pdf
Gosselin, K., Norris, J. L., & Ho, M. J. (2015). Beyond homogenization discourse: Reconsidering the cultural consequences of globalized medical education. Medical Teacher, 38(7), 691-699. https://doi.org/10.3109/0142159X.2015.1105941
Hammersley-Fletcher, L., & Orsmond, P. (2004). Evaluating our peers: Is peer observation a meaningful process? Studies in Higher Education, 29(4), 489-503.https://doi.org/10.1080/0307507042000236380
Hanson, J. L., Rosenberg, A. A., & Lane, J. L. (2013). Narrative descriptions should replace grades and numerical ratings for clinical performance in medical education in the United States. Frontiers in Psychology, 4, 668. https://doi.org/10.3389/fpsyg.2013.00668
Hodges, B. D., Maniate, J. M., Martimianakis, M. A., Alsuwaidan, M., & Segouin, C. (2009). Cracks and crevices: Globalization discourse and medical education. Medical Teacher, 31(10), 910-917. https://doi.org/10.3109/01421590802534932
Hofstede, G. (2001). Culture’s consequences: Comparing values, behaviors, institutions and organisations across nations(2nd ed.). Thousand Oaks, CA: Sage Publications.
Houston, T. K., Ferenchick, G. S., Clark, J. M., Bowen, J. L., Branch, W. T., Alguire, P., … Kern, D. E. (2004). Faculty development needs: Comparing community-based and hospital-based internal medicine teachers. Journal of General Internal Medicine, 19(4), 375-379. https://doi.org/10.1111/j.1525-1497.2004.30619.x
Kikukawa, M., Nabeta, H., Ono, M., Emura, S., Oda, Y., Koizumi, S., & Sakemi, T. (2013). The characteristics of a good clinical teacher as perceived by resident physicians in Japan: A qualitative study. BMC Medical Education, 13, 100. https://doi.org/10.1186/1472-6920-13-100
Oktaria, D., & Soemantri, D. (2018). Undergraduate medical students’ perceptions on feedback-seeking behaviour. Malaysian Journal of Medical Sciences, 25(1), 75-83.
Patton, M. Q. (2002). Qualitative research & evaluation methods (3rd Ed.). Thousand Oaks, CA: Sage Publications.
Ramani, S., & Leinster, S. (2008). AMEE Guide no. 34: Teaching in the clinical environment. Medical Teacher, 30(4), 347-364. https://doi.org/10.1080/01421590802061613
Samuelowicz, K., & Bain, J. D. (2001). Revisiting academic beliefs about teaching and learning. Higher Education, 41(3), 299-325.
Shortland, S. (2004). Observing teaching in HE: A case study of classroom observation within peer observation. International Journal of Management Education, 4(2), 3-15.
Slootweg, I. A., Scherpbier, A., van der Leeuw, R., Heineman, M. J., van der Vleuten, C., & Lombarts, K. M. J. H. (2016). Team communication amongst clinical teachers in a formal meeting of post graduate medical training. Advances in Health Sciences Education, 21(1), 207-219. https://doi.org/10.1007/s10459-015-9627-8
Steinert, Y. (2010). Faculty development: From workshops to communities of practice. Medical Teacher, 32(5), 425-428. https://doi.org/10.3109/01421591003677897
Steinert, Y. (2011). Commentary: Faculty development: The road less traveled. Academic Medicine, 86(4), 409-411. https://doi.org/10.1097/ACM.0b013e31820c6fd3
Steinert, Y. (2014). Faculty development: Core concepts and principles. In Y. Steinert (Ed.), Faculty development in the health professions: A focus on research and practice(pp. 3-25). Dordrecht, The Netherlands: Springer Netherlands.
Steinert, Y., Mann, K., Anderson, B., Barnett, B. M., Centeno, A., Naismith, L., … Dolmans, D. (2016). A systematic review of faculty development initiatives designed to enhance teaching effectiveness: A 10-year update: BEME Guide No. 40. Medical Teacher, 38(8), 769-786. https://doi.org/10.1080/0142159X.2016.1181851
Suhoyo, Y., Van Hell, E. A., Kerdijk, W., Emilia, O., Schönrock-Adema, J., Kuks, J. B. M., & Cohen-Schotanus, J. (2017). Influence of feedback characteristics on perceived learning value of feedback in clerkships: Does culture matter? BMC Medical Education, 17, 69. https://doi.org/10.1186/s12909-017-0904-5
Sullivan, P. B., Buckle, A., Nicky, G., & Atkinson, S. H. (2012). Peer observation of teaching as a faculty development tool. BMC Medical Education, 12, 26. https://doi.org/0.1186/1472-6920-12-26
Sutkin, G., Wagner, E., Harris, I., & Schiffer, R. (2008). What makes a good clinical teacher in medicine? A review of the literature. Academic Medicine, 83(5), 452-466. https://doi.org/10.1097/ACM.0b013e31816bee61
Taylor, E. W. (2003). The relationship between the prior school lives of adult educators’ and their beliefs about teaching adults. International Journal of Lifelong Learning, 22(1), 59-77.
Taylor, E. W., Tisdell, E. J., & Gusic, M. E. (2007). Teaching beliefs of medical educators: Perspectives on clinical teaching in paediatrics. Medical Teacher, 29(4), 371-376.
van der Vleuten, C. P. M., Schuwirth, L. W. T., Driessen, E. W., Dijkstra, J., Tigelaar, D., Baartman, L. K. J., & van Tartwijk, J. (2012). A model for programmatic assessment fit for purpose. Medical Teacher, 34(3), 205-214. https://doi.org/10.3109/0142159X.2012.652239
van Lierop, M., de Jonge, L., Metsemakers, J., & Dolmans, D. (2018). Peer group reflection on student ratings stimulates clinical teachers to generate plans to improve their teaching. Medical Teacher, 40(3), 302-309. https://doi.org/10.1080/0142159X.2017.1406903
Waterval, D. G. J., Frambach, J. M., Driessen, E. W., Muijtjens, A., & Scherpbier, A. J. J. A. (2018). Connected, attracted, and concerned: A Q study on medical crossborder curriculum partnerships. Medical Teacher, 40(12), 1293-1299. https://doi.org/
10.1080/0142159X.2018.1431618
Wong, L. C. J., Wong, P. T. P., & Ishiyama, F. I. (2013). What helps and what hinders in cross-cultural clinical supervision: A critical incident study. The Counseling Psychologist, 41(1), 66-85. https://doi.org/10.1177/0011000012442652
Yiend, J., Weller, S. I., & Kinchin, I. (2014). Peer observation of teaching: The interaction between peer review and developmental models of practice. Journal of Further and Higher Education, 38(4), 465-484. https://doi.org/10.1080/0309877X.2012.726967
Yoon, H. B., Shin, J. S., Lee, S. H., Kim, D. H., Sung, M., Amgalan, N., & Chinzorig, T. (2016). Transnational collaboration for faculty development in health professions education in Mongolia. Korean Journal of Medical Education, 28(4), 381-390. https://doi.org/10.3946/kjme.2016.43
*Diantha Soemantri
Department of Medical Education
Faculty of Medicine, Universitas Indonesia,
Jalan Salemba Raya No. 6, Jakarta 10430, Indonesia
Email: diantha.soemantri@ui.ac.id, dianthasoemantri@yahoo.com
Published online: 3 September, TAPS 2019, 4(3), 33-47
DOI: https://doi.org/10.29060/TAPS.2019-4-3/OA2083
Katharine D. Thomas1& Susie Schofield2
1Department of Family Medicine, Sackler Faculty of Medicine, Tel Aviv University, Israel; 2Centre for Medical Education, University of Dundee, United Kingdom
Abstract
Context: In the twentieth century “cultural” courses in medical education focused on imparting knowledge about ethnic and racial minorities. A new consensus has developed that emphasises a broader definition of culture: education should promote generalisable skills enabling effective interactions with all patients in our culturally complex world. In New Zealand, cultural competency is frequently taught within courses on the indigenous Māori people. This study evaluated whether a generalisable cultural competency intervention was acceptable and effective in this setting.
Methods: A generalisable cultural competency workshop was run for 17 general practitioners. A self-assessment questionnaire was completed by attendees and by a control group of 19 GPs. Participants provided feedback during the seminar and through standardised evaluation forms. Four medical education professionals were interviewed to explore their views on cultural competency education. The interviews were transcribed and thematically analysed.
Results: The questionnaires showed a non-significant, post-seminar increase in total cultural competency score by the seminar participants as compared with the control group (p= .33). Feedback was positive, with all respondents considering the seminar relevant to their needs. The interviewees supported generalisable cultural competency but lacked consensus around whether it should stand-alone or be embedded in ethnically-focused education.
Conclusions: This pilot study shows that participants found generalisable cultural competency education acceptable and that they perceived an improvement in their skills. Medical educators disputed the role of generalisable cultural competency. Further research is needed into how it can be utilised in New Zealand.
Keywords: Medical Education, Cultural Competency, Physicians
Practice Highlights
- Generalisable cultural competency aims to enable successful interactions with all patients.
- It was acceptable to learners more familiar with ethnically focused cultural education.
- There was a lack of consensus as to whether generalisable cultural competency should be taught as a stand-alone subject.
I. INTRODUCTION
Towards the end of the last century, it began to be accepted that culture and health are interrelated (Helman, 1984; Kleinman, Eisenberg, & Good, 1978). As a result, many medical institutions began including what can be broadly described as “cultural competency” in the curriculum (Beach et al., 2005). The ethnic focus of many of these early courses has been criticised for potentially promoting stereotypes and ethnocentricism, the belief that the predominant culture is superior (Kai, Bridgewater, & Spencer, 2001; Núñez, 2000). Many experts suggest that cultural competency education should focus on more generalisable skills such as self-reflection and negotiation to enable physicians to interact effectively with all patients in culturally, socially and linguistically diverse settings (Gregg, & Saha, 2006;Sorensen et al., 2017). “Physicians need a practical set of tools and skills that will enable them to provide quality care to patients everywhere, from anywhere, with whatever differences in background may exist” (Betancourt, 2006, p. 499).
New Zealand has a unique history in terms of its indigenous Māori people as well as in cultural competency education. Legislation passed in 2000 and 2003 required that the principles of the Treaty of Waitangi, an agreement signed in 1840 between the British Crown and Māori leaders, be incorporated into health care policy, education and practice, and that health care practitioners be “culturally competent”. These requirements have led to cultural competency guidelines and programmes that focus on Māori language, customs and health inequalities (Jones et al., 2010; Smith, & Jansen, 2006; The Royal New Zealand College of General Practitioners [RNZGP], 2007) and to partnerships with Māori professionals in producing cultural competency programming (Medical Council of New Zealand [MCNZ], 2017). Whilst additional educational programmes have been introduced which focus on ethnic immigrants to New Zealand, particularly Pacific Islanders (Camplin-Welch, 2007), at the time of writing no generalisable cultural competency programmes exist in New Zealand.
An educational intervention was designed by the authors that focused on the generalisable skills of cultural competency. As a pilot project for future interventions, it also articulates the process and complexities of implementing such programs for medical professionals. This study aimed to evaluate both its effectiveness and its acceptability for participants, and it considered the acceptability of generalisable cultural competency from a broader perspective of its situation in the New Zealand context where cultural competency education is predominantly ethnically and Māori focused.
II. METHODS
A. Educational Intervention
The first author (KT) devised and facilitated a small group, active learning workshop that combined established principles of medical education with a focus on generalisable cultural competency. Prior to it being run, the researcher discussed its content with the Primary Health Organisation (PHO) Director of Māori Health. It was also evaluated and endorsed by the New Zealand Royal College of General Practitioners as appropriate for continuing professional development accreditation.
A small group, informal setting was created to allow what may be sensitive or divisive issues to be discussed and to give all members of the group the opportunity to participate. The three and a half hour workshop included viewing a video of a meeting between a doctor and a patient from ethnically different backgrounds; an exercise to promote self-reflection on the meaning of culture and identity; a twenty minute lecture which included definitions of culture and cultural competency, a review of ethnic diversity in New Zealand and a case study highlighting the importance of generalisable cultural competency in a clinical context; smaller groups of three or four participants reviewed cases studies and allied exercises taken from the website of Cross Cultural Health Care – Case Studies(Horky, 2009).This was followed by a role play in which participants played both the doctor and the patient in several cross-cultural scenarios.
In order to maintain the small group structure, the number of participants per session was limited and it was run on two separate days in identical format.
B. Cultural Competency Questionnaire Development
The Cultural Competency Assessment Tool (CCAT; Kutob, Senf, & Harris Jr, 2009), a self-assessment questionnaire, was adapted for this study. The CCAT questionnaire was chosen because it was designed specifically for family physicians and its validity and reliability had been adequately demonstrated.
Several questions relating to particular ethnic or racial groups were removed or modified and a new question was inserted regarding patients’ socioeconomic situation. Additionally, the focus on diabetes management in the original questionnaire was reduced. The questionnaire was re-validated by gaining input from several general practitioners (GPs), followed by piloting with 19 GPs not in the study.
Reliability was re-evaluated using Cronbach alpha analysis (α = 0.82; Canty, & Ripley, 2012; Falissard, 2012). No changes were made to the questionnaire after piloting. The revalidated version contains 22 Likert questions with a maximum possible score of 88 (refer to Appendix A).
Co-variance analysis of the questionnaire results for the workshop and control groups was used to assess whether the differences in scores on the questionnaires carried out before and after the educational intervention were of statistical significance. Only those who completed the questionnaire twice were included. A second analysis with “last observation carried forward” considered the effects of the lower rate of return of the second round of questionnaires.
C. Workshop Participants and Control Group
All 230 GPs and GP registrars whose clinics are affiliated to a PHO in the Wellington area were offered the opportunity to attend a cultural competency workshop as part of their Continuing Professional Development (CPD) programme. The same group of 230 GPs was invited alternatively to be part of the control group who would not attend the workshop but would fill in the cultural competency questionnaire, nineteen responded. Seventeen GPs attended the workshop, nine at the first seminar and eight at the second.
D. Workshop Evaluation
Effectiveness and acceptability of the workshop were evaluated in several ways: 1) the cultural competency self-assessment questionnaire was used to evaluate the workshop’s effect on participants’ perceived cultural competency. It was completed by workshop participants prior to and one month after the workshop. One month was chosen as a time scale during which participants could have time to reflect but would not have been affected by other interventions; 2) workshop participants provided verbal feedback to the researcher directly at the end of the teaching session; 3) several participants emailed feedback to the researcher or wrote it on their questionnaires; and 4) at the end of the workshop participants completed a standard CPD evaluation form provided by the PHO.
Data were coded on the self-assessment questionnaires and entered for computer analysis using EPI-INFO version 3.5.3 software. For statistical analysis, proportions were compared using the chi-square statistic. Significance was set at P< .05 and means of continuous variables were compared using the Student’s t-test.
E. Interviews
Whilst workshop participants contributed to the assessment of the acceptability of generalisable cultural competency for individuals, they also raised questions as to its acceptability in the broader context of New Zealand medical education.
During the second workshop one participant, Dr KR who at the time was Tumuaki Māori/Māori Director, of the Royal New Zealand College of General Practitioners provided feedback on elements of the session and their relationship to Māori culture and health education. The author was struck by the strength of her comments and felt that a greater comprehension of her views could contribute to the consideration of the place and acceptability of generalisable cultural competency within New Zealand’s medical education system. KR agreed to be interviewed for this study. A semi-structured interview was carried out with questions considering the seminar’s acceptability, the role of cultural competency and ethnically specific education in New Zealand as well as the acceptability of generalisable cultural competency in this setting. The one and a half hour interview was audio recorded and transcribed by KT.
The richness of the data led to three other medical educators being invited to be interviewed in order to further explore the role of generalisable cultural competency in the New Zealand context. Two (Dr BG and Dr SM were Pakeha [New Zealanders of European origin]) GPs, who had attended the seminars and are active in student and GP trainee education. They both work in urban practices with patients from many different ethnic backgrounds. The other (MM) was Māori, and Director of Māori Health for the PHO, who had discussed the workshop with the lead author prior to its being conducted. She has a background of many years working in health care as a nursing and mental health clinical leader as well as a number of roles relating specifically to Māori service provision and health. The interviewees were chosen as they were both familiar with the workshop and with health care provision in New Zealand as well as being involved in New Zealand medical education. All interviewees have agreed to be identified.
The structure and content of the three subsequent interviews were based on the interview with KR, and are shown in Appendix B.
III. RESULTS
A. Cultural Competency Questionnaires
Sixteen of the seventeen (94%) GPs who attended the workshops completed questionnaires prior to the sessions. Fifteen (88%) completed the second round of questionnaires one month later. Of the control group, 19 completed the questionnaire at the same time as the intervention group, and 10 (53%) completed the questionnaire a second time, one month later.
Table 1 summarises the demographic details of the workshop and control groups. The total questionnaire scores increased amongst the group of doctors who attended the seminars from a mean of 62.7 prior to the seminar to 64.3 one month later. In the control group, the total questionnaire score went down in the second round of questionnaires from a mean of 62.9 to 61.9 (Table 2).
| Seminar Group
no. (% of total) |
Control Group
no. (% of total) |
|
| Mean age (years) | 52 | 47 |
| Completed vocational training in New Zealand | 10 (62.5) | 14 (73.7) |
| Completed vocational training elsewhere | 5 (31.5) | 4 (21.5) |
| Gender, Female | 11 (68.8) | 13 (68.4) |
| Born in New Zealand | 8 (50.0) | 15 (78.9) |
| Ethnic Group, New Zealand European | 7 (43.8) | 15 (78.9) |
| Ethnic Group, Māori | 1 ( 6.3) | 0 (0) |
| Other Ethnic Group, self-defined: Sri Lankan, UK/Australian, Hungarian parents, Indian, European, Anglo/Irish, Irish, Chinese, Mother of Māori child | 8 (50.0) | 4 (21.1) |
Table 1. Demographic details of workshop participants N= 16, control group N= 19 (one participant did not provide demographic details)
| Participants pre seminar | Participants post seminar | Control first round |
Control second round | |
| CULTURE | 17.7 | 18.1 | 19.3 | 17.9 |
| EMPOWER | 12.1 | 13.0 | 11.9 | 11.9 |
| EXPLAN | 16.2 | 16.5 | 15.8 | 15.9 |
| JUDGE | 16.7 | 16.6 | 15.8 | 16.2 |
| Total | 62.7 | 64.3 | 62.9 | 61.9 |
Note: CULTURE = Cultural Self-Awareness domain, EXPLAN = Explanatory Model Elicitation domain,
JUDGE = Non-judgemental domain, EMPOWER = Cultural Empowerment/Medical knowledge transmission skills
Table 2. Mean questionnaire scores, domains and total from 16 workshop participants and 19 control group members
In both sets of co-variance calculations, there was an increase in total and domain scores for the workshop group as compared with the control group (Total score increase p= .33, with last observation carried forward p= .27). However, this increase was not statistically significant.
The pre-intervention scores of the workshop and control groups (35 questionnaires) were also reviewed to see whether demographic factors affected cultural competency scores. Total scores did not differ significantly for gender (t-statistic = 0.6167, p= .5417), age (Pearson’s coefficient correlation r= .17, p= .3704), or for whether a doctor was born in New Zealand (t-statistic = 1.3190, p= .1963). There was however a significant difference for the total scores when prior cultural competency training was considered (p= .03).
B. CPD Evaluation Form
CPD evaluation results were overwhelmingly positive both in terms of the workshop’s content and its relevance to participants. Table 3 shows the results in full from 15 completed forms, ten from the first workshop (100% of participants including one non-physician) and five from the second workshop (62.5% of participants).
| Strongly disagree (1) | Disagree (2) | Agree
(3) |
Strongly agree (4) | Mean
± SD |
|
| Contained no commercial or professional bias in the educational content | 6.7 | 93.3 | 3.9 ± 0.25 | ||
| Presented new information | 6.6 | 60 | 33.3 | 3.3 ± 0.57 | |
| Was appropriate for local conditions and requirements | 60 | 40 | 3.4 ± 0.49 | ||
| Was well administered in terms of course information, registration and certification | 40 | 60 | 3.6 ± 0.49 | ||
| Please comment on the suitability of the format of the delivery | 46.7 | 53.3 | 3.5 ± 0.5 | ||
| Was it primary health care focused and driven | 46.7 | 53.3 | 3.5 ± 0.5 | ||
| Provided a stimulating learning environment | 53.3 | 46.7 | 3.5 ± 0.5 | ||
| Conveyed relevant information | 60 | 40 | 3.4 ± 0.49 | ||
| Updated my knowledge in this area | 6.6 | 60 | 33.3 | 3.3 ± 0.57 | |
| Gave ample opportunity for participant input, feedback and evaluation | 20 | 80 | 3.8 ± 0.4 | ||
| Was well advertised with clearly stated course information | 60 | 40 | 3.4 ± 0.49 |
Table 3. CPD evaluation form results (in %), N= 15
C. Feedback
All comments relating to the workshop as a whole were positive. It was described as “interesting and very helpful”, “fun and enlightening”, “fun and interesting”.
One participant, however, was uncomfortable with role play in which participants played genders and ethnicities different from their own. This led to a discussion during the workshop in which a second participant agreed that role players should maintain their own gender and ethnic identity. Other workshop participants felt that playing “different” roles was a beneficial part of role play, pertinent to cultural competency, and should be done.
D. Interviews
Several themes were identified from the interviews some of which showed common ground between all the interviewees, others revealed conflicting views (Appendix B). Those that relate particularly to the acceptability of cultural competency are considered below. Whilst the interviewees have agreed to be identified in this article, their responses have been anonymised, and are identified as IP1 and IP2 (Pakeha) and IM1 and IM2 (Māori).
1) Equality and social justice:All the interviewees expressed similar ideas regarding the importance of equality and social justice in their work.
“We should work in a socially accountable way and that those who suffer the greatest disparities are those for whom the greatest health gains are available if we provide our skills for them.”
(IP1)
“What can I do to help this person get a better deal?”
(IP2)
“It’s not just about being humble about other people’s cultures and being interested in them and having an enquiring mind and being patient-centred but it’s more than that; It’s actually about doing it for a reason to improve the inequalities that we’ve got.”
(IM1)
2) Māori health education versus cultural competency education:There was unanimous support for teaching generalisable cultural competency. They were similarly in agreement that, in New Zealand, education on Māori is of key importance. There was, however, no consensus as to whether interventions on generalisable skills should continue to be combined with, and to a certain degree secondary to, education about Māori health issues.
IM1 argued that cultural competency education should be taught under the framework of Māori health education and feared that stand-alone education on generalisable skills could distract from the central need of addressing Māori health inequalities:
“If Māori is not explicit in your training or in any training around cultural competency, are we educating to maintain disparity?”
(IM1)
IM1 argued that skills learnt as part of education about Māori can be applied to other situations and that this removes the need for additional cultural competency education:
“I think if they can learn to work with Māori, at least they’ve got that skill under their belt and then some of those skills are going to be transferrable.”
(IM1)
The other interviewees expressed some unease about the current practice in New Zealand of amalgamating cultural competency education with courses on Māori health. IP2 argued that they were two distinct and vital subjects that required separate educational approaches:
“I think there should be Māori health training and then there should be cultural competency… The Māori health stuff needs to almost probably stand alone because it’s a big factor and a big issue.”
(IP2)
IM2 suggested that under the current situation, generalisable skills tended to be overshadowed by education on Māori health:
“When you say cultural competency, people automatically think that you’re talking about engaging with Māori.”
(IM2)
IP1 worried that it was currently difficult for educators to effectively teach generalisable skills when they were required to focus on Māori health issues. He believed that this requirement was particularly difficult for Māori educators.
“Some Māori who are teaching cultural competency are actually disabled from doing the culture general stuff very well because of the extent of their own agenda being needing to know about Māori culture.”
(IP1)
IP1 and IP2 suggested that in present-day New Zealand, with its large number of ethnic groups, the current focus on only one or a limited number of ethnic groups may be inappropriate.
“I am concerned more about how we can improve things for the vast diversity of cultural backgrounds.”
(IP1)
“We are more diverse and it’s that whole sense of diversity that we need to deal with and we need have some keys to being culturally competent for that.”
(IP2)
3) Difficulties for Māori and Pakeha health professionals in discussing cultural competency education with each other:There was a consensus that interviews suggested that these issues are politically sensitive and that communication difficulties impede open discussion about cultural competency education. IM2 suggested the need to develop relationships between Māori and non-Māori doctors:
“So people feel safe enough to say what they’re thinking.”
(IM2)
IP1 argued that,
“All the issues around racism and colonisation…They are part of the difficulty in communicating… the power differential between the stereotypical white and stereotypical Māori is unbalanced.”
(IP1)
IP2 also noted a sense of division between Māori and non-Māori doctors,
“There is a divide but I don’t think it’s deliberately set up but I think there a few protagonists who [would] perpetuate it if they possibly could.”
(IP2)
IV. DISCUSSION
This study considered the efficacy and acceptability of generalisable cultural competency to GPs in a New Zealand setting of familiarity with ethnically focused cultural education. The non-significant increase in self-assessment scores for the physicians attending the workshop suggests an improvement in their cultural competency. Feedback from participants showed that they considered the workshop to be acceptable and appropriate to their needs. However, interviews with medical educators revealed the complexities and potential difficulties of introducing generalisable cultural competency to curricula in which specific ethnic education exists.
This research is relevant to the particular situation in New Zealand but also to medical education worldwide where cultural competency training often continues to be ethnically or racially focused (Beach et al., 2005; Horvat, Horey, Romios, & Kis-Rigo, 2014). This study also contributes to the wider base of cultural competency research, a field where adequate evaluation of educational programmes and appropriate assessment tools are lacking (Dogra, & Karnik, 2004; Jernigan, Hearod, Tran, Norris, & Buchwald, 2016; Lie, Lee-Rey, Gomez, Bereknyei, & Braddock, 2010). Furthermore, it participates in the discussion as to the place of medical education in improving ethnic minority and indigenous peoples’ health and in reducing disparities between population groups (Brach & Fraser, 2000; Durie, 2003).
A limitation of this study is the low number of GPs who chose to attend the workshop, which can be explained in part by its setting: the workshop being offered as part of non-compulsory CPD programming with many options. In addition, as “Cultural Competency” advisory standards appear in the Medical Council of New Zealand guidelines (MCNZ, 2016) and in The Royal New Zealand College of General Practitioners guidelines (RNZGP, 2007) it may be that their ubiquitous presence makes physicians feel that they do not need further instruction.
The study failed to show a significant increase in CCAT scores one month after the workshop. While this may be due to the small total number of participants it is also possible that those choosing to participate in cultural competency education already possess an interest in the subject and a higher degree of competency (Godkin & Savageau, 2001) and thus, have less potential for improvement. The study did, however, reveal that the only demographic significantly linked to higher questionnaire scores was previous cultural competency training. The need for self-reflection, an element of the workshop, may have led participants to take a stronger critical stance when completing the second round of questionnaires, consequently producing lower scores (Chun, Jackson, Lin, & Park, 2010). It is also possible that the mere act of completing the questionnaire contributed to increased self-awareness of the complexities of cultural competency. The slight decrease for the control group suggests this was not the case.
In this study, the acceptability of generalisable cultural competency was evident in the positive written and face-to-face feedback as well as in the CPD evaluation forms. However, the workshop participants were not asked to compare this teaching session with other ethnically focused cultural competency education that they may have experienced previously. Thus, while it is possible to conclude from their feedback that participants considered the workshop to be relevant and appropriate to their needs, it is not possible to conclude that they found it more appropriate or more relevant than ethnically focused education. Additionally, the presence of only one Māori participant may mean that the Māori perspective is under-represented in the feedback from the workshop although the diversity of participants’ own ethnic backgrounds does reflect the make-up of New Zealand’s current doctor workforce. Generalisable cultural competency’s acceptability from a broader perspective of medical education in New Zealand cannot be concluded from this study, with the interviewees suggesting diverse possibilities for cultural competency education: from a standalone generalisable subject to Māori focused education.
The question of how generalisable cultural competency should fit into current educational curricula, and whether it should be taught as a standalone subject or within the rubric of education about minority groups, remains a complex and fraught one (Gray, 2007; Jones et al., 2010). Whilst a majority of medical educators propose cultural competency as a generalisable subject (Betancourt, 2006; Gregg & Saha, 2006; Sorensen et al., 2017), the necessity of ethnic groups having their own specific cultural needs addressed in medical education is also supported (Eiser & Ellis, 2007; Jones et al., 2010). In addition, in New Zealand, the Treaty of Waitangi makes an obligation towards Māori to right past injustices and by implication, reduce health discrepancies. Māori groups have become increasingly involved in education on Māori health and cultural competency in an attempt to meet these obligations (McPherson, Harwood, & McNaughton, 2003).
It was apparent from the preparatory stages of this research when the seminar content was reviewed with colleagues, through to the seminars and the interviews that these are sensitive and potentially politically charged issues, not easily discussed. In particular, the interviewees suggested that open discussion about cultural issues, between educators from different ethnic backgrounds was difficult.
It may be that, in order to adequately address the acceptability of generalisable cultural competency in New Zealand, the apparent communication difficulties between Pakeha and Māori medical professionals also need to be tackled. Creating separate focus groups of Māori and non-Māori physicians could allow maximum freedom of expression with regards to cultural competency education. The issues raised could then form the basis of workshop content and mediation. The role of advocate medical professionals in promoting the needs of specific groups and creating an academic agenda is seen worldwide and is likely to be accompanied by similar difficulties to those found in New Zealand (Australian Indigenous Doctors Association, n.d.; Marcy, 2011).
This study adds to the body of work in which cultural competency has been delivered in workshops (Carter et al., 2006; Genao, Bussey-Jones, St. George, & Corbie-Smith, 2009; Ho, Yao, Lee, Beach, & Green, 2008; Khanna, Cheyney, & Engle, 2009; Ross et al., 2010). Some of these studies were able to demonstrate improvements in participants’ cultural competency following educational interventions (Carter et al., 2006; Genao et al., 2009; Ho et al., 2008) although measures of patients’ health outcomes were unaffected (Khanna et al., 2009). This research also confirms that cultural competency education based on generalisable skills, rather than on specific ethnic or racial groups, can be effective (Khanna et al., 2009; Thom, Tirado, Woon, & McBride, 2006; Webb & Sergison, 2003).
Further research is now needed into how cultural competency interventions can best improve the skills and abilities of health care professionals in today’s multi-cultural world. For instance, no attempt has been made to compare the acceptability or impact of specific and generalisable cultural competency interventions. There is also a need for further evaluation of how best to deliver generalisable cultural competency itself. Particularly, in the case of post-graduate physicians, there is a lack of research into the effectiveness of interventions. Further investigation is needed into the most effective way to improve the cultural competency of a large number of physicians who have never been exposed to the subject. A number of questions remain unanswered. Are short workshops as effective as long ones? Is attendance on a single occasion sufficient or is regular reinforcement required? Is the teaching of multi-disciplinary groups useful or is it preferable to teach professionals with their peers?
The dilemmas raised in this research, while specific to the situation in New Zealand, are likely to be echoed globally in medical education. These include the need to improve dialogue between advocates of ethnic minorities and educators and amongst physicians themselves, and the need to marry an acknowledgement of the needs of specific groups in society with the realisation that the cultural identity of doctors and patients is often highly complex, varied and multi-faceted. It is vital to dispel fears that generalisable education will decrease attention on health disparities suffered by specific ethnic and racial groups. It needs to be demonstrated that generalisable cultural competency can exist alongside, and supplement interventions relating to disadvantaged groups, rather than replace them.
The authors suggest that cultural competency medical education be generalisable and integrated both vertically and horizontally through pre- and post-graduate medical studies, and in the case of New Zealand be separate and distinct from the subject of Māori health. We advocate that generalisable cultural skills training should be a distinct part of medical education and taught separately from courses regarding the health and culture of specific ethnic groups.
V. CONCLUSION
Notwithstanding the small number of participants, this study demonstrates the acceptability of a generalisable cultural competency workshop for participants already familiar with ethnically focused cultural education. Self-assessment scores suggest an increase in cultural competency for seminar participants. The study interviews confirm the acceptability of generalisable cultural competency as a subject but also illustrate the complexity of its potential insertion into medical curricula. It appears that while generalisable cultural competency is widely acceptable to both educators and learners its place in medical curricula is, like culture itself, a complex and disputed subject.
Notes on Contributors
The authors would like to emphasise that the views expressed in the submitted article are those of the authors alone and not an official position of their institutions. All contributors consented to be named.
KT designed and carried out the research. SS made substantial contributions to the conception and design of the study as well as to the drafting the manuscript. Both authors have given approval to this final version and are accountable to all aspects of the work.
Ethical Approval
Prior to carrying out this research, its details were reviewed by the National Ethics Committee of the New Zealand Ministry of Health and a response received that that it was unnecessary to apply for formal ethical approval.
Funding
All authors declare no financial support from or relationship with any organisation which might have an interest in the submitted work.
Declaration of Interest
Authors declared that there was no conflict of interest involved in this paper.
References
Australian Indigenous Doctors Association. (n.d.). Cultural safety. Retrieved from https://www.aida.org.au/our-work/cultural-safety
Beach, M. C., Price, E. G., Gary, T. L., Robinson, K. A., Gozu, A., Palacio, A., … Cooper, L. A. (2005). Cultural competence: A systematic review of health care provider educational interventions. Medical Care, 43(4), 356-373.
Betancourt, J. R. (2006). Cultural competence and medical education: Many names, many perspectives, one goal.Academic Medicine,84(6), 499-501.
Brach, C., & Fraser, I. (2000). Can cultural competency reduce ethnic and racial health disparities? A review and conceptual model. Medical Care Research and Review, 57(Suppl 1), 181-217.
Camplin-Welch, V. (2007). Cross-cultural resource for health practitioners working with culturally and linguistically diverse (CALD) clients.Wellington, New Zealand: Waitemata District Health Board and Refugees as Survivors New Zealand Trust.
Canty, A., & Ripley, B. (2012). Boot: Bootstrap (S-Plus) Functions. R package version 1.3-4.
Carter, M. M., Lewis, E. L., Sbrocco, T., Tanenbaum, R., Oswald, J. C., Sykora, W., … Hill, L. D. (2006). Cultural competency training for third year clerkship students: Effects of an interactive workshop on student attitudes. Journal of the National Medical Association,98(11), 1772-1778.
Chun, M. B. J., Jackson, D. S., Lin, S. Y., & Park, E. R. (2010). A comparison of surgery and family medicine residents’ perceptions of cross-cultural care training. Hawai’i Medical Journal, 69(12), 289-293.
Dogra, N., & Karnik, N. (2004). Teaching cultural diversity to medical students. Medical Teacher,26(8), 677-680.
Durie, M. H. (2003). The health of indigenous peoples: Depends on genetics, politics, and socioeconomic factors. BMJ, 326(7388), 510-511.
Eiser, A. R., & Ellis, G. (2007). Cultural competence and the African American experience with health care: The case for specific content in cross-cultural education. Academic Medicine, 82(2), 176-183.
Falissard, B. (2012). Various methods used in psychometry [PDF File]. Retrieved from http://cran.r-project.org/web/packages/psy/psy.pdf
Genao, I., Bussey-Jones,J., St. George, D. M., & Corbie-Smith, G. (2009). Empowering students with cultural competence knowledge: Randomized controlled trial of a cultural competence curriculum for medical students. Journal of the National Medical Association, 101(12), 1241-1246.
Godkin, M. A., & Savageau, J. A. (2001). The effect of a global multiculturalism track on cultural competence of preclinical medical students. Family Medicine,33(3), 178-186.
Gray, B. (2007). English language difficulties at general practices in Auckland, New Zealand. A major limitation to good practice. The New Zealand Medical Journal,120(1264),10-12.
Gregg, J., & Saha,S. (2006) Losing culture on the way to competence: The use and misuse of culture in medical education. Academic Medicine, 81(6), 542-547.
Helman, C. (1984). Culture, health and illness. London, England: Butterworth-Heinemann.
Ho, M. J., Yao, G., Lee, K. L., Beach, M. C., & Green, A. R. (2008). Cross-cultural medical education: Can patient-centered cultural competency training be effective in non-Western countries? Medical Teacher, 30(7), 719-721.
Horky, S. (2009). Cross cultural health care – Case studies.
Retrieved from https://support.mchtraining.net/national_ccce/index.html
Horvat, L., Horey, D., Romios, P., & Kis-Rigo, J. (2014). Cultural competence education for health professionals. Cochrane Database of Systematic Reviews, 2014(5), CD009405. https://doi.org/10.1002/14651858.CD009405.pub2
Jernigan, V. B. B., Hearod, J. B., Tran, K., Norris, K. C., & Buchwald, D. (2016). An examination of cultural competence training in US medical education guided by the tool for assessing cultural competence training. Journal of Health Disparities Research and Practice, 9(3), 150-167.
Jones, R., Pitama, S., Huria, T., Poole, P., McKimm, J., Pinnock, R., & Reid, P.(2010). Medical education to improve Maori health. The New Zealand Medical Journal, 123(1316), 113-122.
Kai, J., Bridgewater, R., & Spencer, J. (2001). ‘Just think of TB and Asians, that’s all I ever hear’: Medical learners’ views about training to work in ethnically diverse society. Medical Education, 35(3), 250-256.
Khanna, S. K., Cheyney, M., & Engle, M.(2009).Cultural competency in health care: Evaluating the outcomes of a cultural competency training among health care professionals. Journal of the National Medical Association,101(9), 886-892.
Kleinman, A., Eisenberg, L., & Good, B. (1978). Culture illness and care: Clinical lessons from anthropologic and cross-cultural research. Annals of Internal Medicine, 88(2), 251-258.
Kutob, R. N., Senf, J. H., & Harris, J. M. (2009). Teaching culturally effective diabetes care: Results of a randomized controlled trial. Family Medicine, 41(3), 167-174.
Lie, D. A., Lee-Rey, E., Gomez, A., Bereknyei, S., & Braddock, C. H. (2010). Does cultural competency training of health professionals improve patient outcomes? A systemic review and proposed algorithm for future research.Journal of General Internal Medicine, 26(3), 317-325.
Marcy, J. (2011, November 3). Advocates: Don’t scrap minority health training programmes. Kaiser Health News. Retrieved from https://khn.org
McPherson, K. M., Harwood, M., & McNaughton, H. K. (2003). Ethnicity, equity and quality: Lessons from New Zealand. British Medical Journal, 327(7412), 443-444.
Medical Council of New Zealand. (2016). Good medical practice. Wellington, New Zealand: Author.
Medical Council of New Zealand. (2017, June 9). Strengthening the cultural competence of our doctors [Media release]. Retrieved from https://www.mcnz.org.nz/news-and-publications/media-releases/strengthening-the-cultural-competence-of-our-doctors
Núñez, A. E. (2000). Transforming cultural competency into cross-cultural efficacy in women’s health education. Academic Medicine, 75(11), 1071-1080.
Ross, P. T., Cené, C. W., Bussey-Jones, J., Brown, A. F., Blackman, D., Fernández, A., … Lypson, M. L. (2010). A strategy for improving health disparities education in medicine. Journal of General Internal Medicine, 25(Suppl 2), 160-163.
Smith, K., & Jansen, C. (2006). A report on cultural competency training provided for two PHOs. New Zealand Family Physician,33(5), 310-312.
Sorensen, J., Norredam, M., Dogra, N., Essink-Bot, M. L., Suurmond, J., & Krasnik, A. (2017). Enhancing cultural competence in medical education. International Journal of Medical Education, 8, 28-30.
The Royal New Zealand College of General Practitioners. (2007). Cultural competence: Advice for GPs to create and maintain culturally competent practices.Wellington, New Zealand: Author.
Thom, D. H., Tirado, M. D., Woon, T. L., & McBride, M. R. (2006). Development and evaluation of a cultural competency training curriculum. BMC Medical Education,6, 38.
Webb, E., & Sergison, M. (2003). Evaluation of cultural competence and antiracism training in child health services. Archives of Disease in Childhood,88(4), 291-294.
*Katharine Thomas
Department of Family Medicine,
Tel Aviv-Yafo and Dan Petach Tikva DistrictsClalit,
Health Services and Department of Family Medicine,
Tel Aviv University,
Ramat Aviv PO Box 39040, Tel Aviv 6997801
Tel: 00972 54929 3441
Email: marshykd@gmail.com
Published online: 3 September, TAPS 2019, 4(3), 48-56
DOI: https://doi.org/10.29060/TAPS.2019-4-3/OA2090
Thilanka Seneviratne1, Kosala Somaratne2, Deelaka Bandara1, Vindya Alahakoon1, Dilan Bandara1, Randima Munasinghe1, Nabil Ilyas3, Thilini Subasingha4& P. V. R. Kumarasiri5
1Department of Pharmacology, Faculty of Medicine, University of Peradeniya, Sri Lanka; 2Base Hospital, Rikillagaskada, Sri Lanka; 3Teaching Hospital, Peradeniya, Sri Lanka; 4Lady Ridgeway Hospital, Colombo, Sri Lanka; 5Department of Community Medicine, Faculty of Medicine, University of Peradeniya, Sri Lanka
Abstract
Introduction: English is the medium of instruction in the medical faculties in Sri Lanka, although the majority of the students who admit to the medical faculties completed their secondary school education with Sinhala as their first language. This disparity presents a potential barrier to their assimilation of knowledge in medical education.
Objective: To assess the medical students’ perception of the medium of instruction in medical education.
Method: The medical students of the Faculty of Medicine, University of Peradeniya, Sri Lanka, enrolled from 2013 to 2017, whose first language is Sinhala were included in the study. Perceptions about the medium of instruction in medical education were assessed through an anonymous self-administered questionnaire, which used a five-point Likert scale for responses.
Results: From the total of 837 medical students, 665 (79.5%) participants had studied the General Certificate of Education – Ordinary Level (GCE O/L) in Sinhala and 172 (20.5%) in English. Eighty-eight percent (87.8%) had obtained an “A” grade for English Language in the GCE O/L examination. Over half (53.4%) of students responded that if medical textbooks were available in Sinhala, it would have increased their understanding of medical concepts. Nearly two-thirds (61%) responded that they perceived their performance in clinical examinations would have improved if those were carried out in Sinhala.
Conclusion: The findings reveal the positive perception of students towards using their first language in medical education. Specifically, students feel that concepts of medicine would be better understood if medical textbooks were available in Sinhala and that they could have performed better if examinations were done in Sinhala, their first language.
Keywords: Mother Tongue, Native Language, First Language, Sinhala, English, Medical Education
Practice Highlights
- Students perceive that learning will be easier if medical textbooks were in Sinhala.
- Students opined that they can perform better if examinations are done in Sinhala.
- Learning medicine would be easier if medical teaching is supported in Sinhala.
I. INTRODUCTION
The medium of instruction used in different levels of education in Sri Lanka varies, with the main languages used being Sinhala (the native or first language or ‘mother tongue’) and English (the second or additional language for most Sri Lankans). Though Sinhala is used in primary education in all the government schools, certain schools offer secondary education in English, as a medium of instruction. At the secondary level, a small percentage of students select the English medium up to General Certificate of Education – Ordinary Level (GCE O/L) exam; while a lesser number of students select the English medium for General Certificate of Education – Advanced Level (GCE A/L) studies. Whilst English has been the official medium of instruction in undergraduate medical education since its inception, most of the students who enter the medical faculty had completed both their primary and secondary education in the Sinhala medium, yet have to switch over to the medium of English at the university level.
This change of the medium of instruction at the university level hinders some students from performing well in their university studies (Nyika, 2015). For students whose first language is not English, English language proficiency is shown to be one of the most important predictors of academic success (Ahmed, Ahmed, & Al-Jouhari, 1988; Al-Mously, Salem, & Al-Hamdan, 2013; Ariyasinghe & Pallegama, 2013; Lucas et al., 1997).
A study carried out by Ellili-Cherifand Alkhateeb (2015) in which medicine was taught in both English and in the students’ first language, identified the students’ positive perception in learning through their first language. Dutcher and Tucker (2012) and Laguarda and Woodward (2013) found that using learner’s first language in teaching helps them to acquire knowledge and skills with ease. However, Sri Lankan students are deprived of the benefits of learning medicine through Sinhala, as the medical schools in Sri Lanka have never tried teaching medicine in the native language.
It is interesting to note that, medical education in the majority of high-income countries is carried out in their respective native language. The practice of using a language other than the native language is particularly seen in some countries of South/South East Asia, Middle East and Africa (Kirkpatrick, 2014; Narayan, 2013; Telmesani, Zaini, & Ghazi, 2011).
Students’ perceptions of the impact of the medium of instruction, on teaching and learning medicine, have not been sought so far in Sri Lanka. Thus, we thought of probing into this important aspect of medical education.
Our objective of this study was to assess the student perception of the medium of instruction in undergraduate medical education, among the medical students whose mother tongue is Sinhala. Also to assess the effect of medium of study in school education, level of English proficiency, stage of clinical education (clinical vs pre-clinical), on the student perception of the medium of instruction.
II. METHODS
A. Study Design and Setting
A descriptive study was conducted at the Faculty of Medicine, University of Peradeniya during June 2018.
B. Inclusion Criteria
All medical undergraduates enrolled at the Faculty of Medicine, Peradeniya from 2013 to 2017 were included in the study.
C. Exclusion Criteria
Students whose first language is not Sinhala were excluded.
D. Study Sample
The sample size was calculated to be 422 using the formula given below. Statistically, precision was set at 5% and power at 95%.
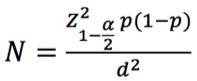
(Lwanga & Lemeshow, 1991)
d = .5
Since one of the objectives was to compare the perceptions according to the stage of learning, 422 students were selected from pre-clinical and clinical stages each by simple random sampling (so in total 844 students).
E. Variables and Data Collection Tool
Data were collected using a self-administered, anonymous questionnaire. The first part of the questionnaire asked for demographic details of the participants.
The second part sought information about the medium of instruction at school education (GCE O/L and GCE/AL) and the grade obtained for the English language in school exams (GCE O/L and GCE A/L).
The third part of the questionnaire asked about their perception of the medium of instruction. A questionnaire was adapted from the study carried out by Ellili-Cherif and Alkhateeb (2015) and pre-tested. The questionnaire consists of 15 items on student perception of the medium of instruction, measured using a five-point Likert scale, whereby ‘1’ indicates strongly agree and ‘5’ indicates strongly disagree.
F. Implementation
844 eligible students were invited to participate in the study who were all approached on the same day and time. The students were briefed about the study by the researchers and questionnaires were distributed with a copy of the information sheet and the consent forms. Participation was anonymous and voluntary. Written consent was obtained from the students who volunteered to participate. Researchers were there in person to clarify any doubts raised by the students. They were given 30 to 45 minutes to complete the questionnaire under the supervision of the researchers. The completed questionnaires were then collected by the researchers from the students.
G. Statistical Analysis
Results were entered into an Excel spreadsheet and then transferred into SPSS (version 23) for descriptive analysis. Initial descriptive details were calculated for demographic data. The percentage of students in the categories of strongly agreed, agreed, undecided, disagreed, and strongly disagreed with the statements was calculated. Their perceptions were analysed with regard to the following differences using chi-square test (P < .05),
1) Clinical vs preclinical stages of medical education;
2) School education (GCE O/L) in the Sinhala medium (Sinhala medium school education [SM]) vs school education (GCE O/L) in English medium (English medium school education [EM]); and
3) The grade for the English language in GCE O/L examination – grade ‘A’ vs other grades (B, C and S).
The GCE A/L examination in Sri Lanka is a competitive examination for selection to university. Marks gained by students for the GCE A/L English are not taken into consideration when scores are calculated. Therefore, students tend to neglect the English language during their A/L studies. Students do however pay attention to GCE O/L English language because the grade for English is sometimes considered by employers and for admission to certain courses of higher studies. Therefore, the grade for English for GCE O/L is a better representative of English proficiency of particular students than that of A/L. Thus, for this study, English grade for GCE O/L was taken as a representative figure of student’s English proficiency.
Percentage of students who agreed (agree + strongly agree), disagreed (disagree + strongly disagree) and undecided was used when doing the chi-square analysis.
H. Ethical Issues
Data were collected anonymously. No sensitive questions were included in the questionnaire. Ethical approval for the study was obtained from the Ethical Review Committee of Faculty of Medicine, Peradeniya, Sri Lanka.
III. RESULTS
A. Participants’ Demographics
A total of 837 medical students (65.03% of the total students in the faculty) volunteered for the study. 416 of them were from the pre-clinical stage (66.14% of the total pre-clinical students) while 421 were from the clinical stage (64.08% of the total clinical students). In our study sample, 60.93% of the participants were female and 39.07% were male (In the study population 58.28% were females and 41.72% were males). The mean age of the participant students was 24.4 (± 1.83). Refer to Table 1.
| Items | N (no. of students) | % |
| Age Groups
21-24 25-28 |
436
401 |
52.09 47.91 |
| Gender
Male Female |
327 510 |
39.07 60.93 |
| Batch
Pre-clinical Clinical |
416 421 |
49.7 50.3 |
Table 1. Demographic characteristics of the study participants
B. Level of English Proficiency and the Medium of Instruction in School
For GCE O/L, 79.5% had studied in Sinhala and 20.5 % in English. As for GCE A/L, 94.7% had studied in Sinhala while only 5.3% had studied in English. For GCE O/L English language, 87.8% of participants had obtained an ‘A’ grade while 12.2% had obtained other grades. For GCE A/L English language, 40.7% had scored an ‘A’ grade while 59.3% had scored other grades.
C. Perception of the Medium of Instruction
1) Acquisition of knowledge in medicine:More than half the students (53.4%) responded that if medical textbooks were available in Sinhala, it could have led to a better understanding of concepts of medicine. Regarding classroom teaching, 44.9% of students responded that the classroom atmosphere would be more conducive for learning if the teacher taught in Sinhala rather than English. Nearly two-thirds of students (61%) were of the opinion that they could perform better if clinical examinations were done in Sinhala.
2) Adopting students’ first language in medical education:One quarter (25.3%) of the students agreed with adopting Sinhala as the medium of teaching in medical education and 16.5% agreed with using Sinhala in postgraduate education.
3) Use of both Sinhala and English in lessons:The majority of students (73.2%) felt that using both English and Sinhala within the same lesson can facilitate learning.
The summary of the responses for the 15 item questionnaire on the perception of the medium of instruction is set out in Table 2.
| Item No. | Item | Percentage of Responses % | ||||
| 1 | 2 | 3 | 4 | 5 | ||
| 1 | All the developed countries in the world use mother tongue* as the medium of higher education. It may be a sensible practice to be adopted in Sri Lanka as well | 11.9 | 20.4 | 18.5 | 31.8 | 17.4 |
| 2 | I can obtain higher marks answering examination questions in Sinhala | 24.3 | 26.4 | 23.7 | 16.1 | 9.5 |
| 3 | I feel that I can write better in Sinhala than in English | 30.2 | 31.5 | 15.2 | 14.1 | 8.1 |
| 4 | I can express ideas better if clinical examinations were to be conducted in Sinhala | 30.6 | 30.4 | 21.1 | 12.8 | 5.1 |
| 5 | Teaching should use Sinhala as the main medium of instruction at the beginning of the term, gradually increasing the use of English as a medium of instruction, so that students can get used to studying in English step by step | 17.6 | 29.5 | 23.9 | 19.2 | 9.3 |
| 6 | I believe my parents would like me to study all subjects in English | 16.2 | 34.3 | 34.7 | 10.0 | 4.7 |
| 7 | I think the greatest difficulty in using English to study is learning a great many new words | 13.7 | 44.8 | 19.0 | 19.0 | 3.4 |
| 8 | If medical textbooks were available in Sinhala, it could have saved a lot of study time | 13.8 | 26.0 | 24.5 | 23.7 | 12.0 |
| 9 | If medical textbooks were available in Sinhala, it could have led to a better understanding of the concept of medicine | 17.6 | 35.8 | 20.1 | 17.7 | 8.7 |
| 10 | Problems of learning are created if Sinhala is the instructional language in the primary school while English is the instructional language in the university | 29.5 | 39.7 | 21.5 | 7.5 | 1.7 |
| 11 | I support adopting mother-tongue education in the Medical Faculty | 5.8 | 19.5 | 34.3 | 26.8 | 13.7 |
| 12 | I support adopting mother-tongue education for postgraduate students as well | 4.8 | 11.7 | 33.3 | 31.0 | 19.3 |
| 13 | I feel that teachers using both English and Sinhala within the same lesson can facilitate students to study medical subjects | 25.2 | 48.0 | 15.1 | 8.7 | 3.1 |
| 14 | If the teacher teaches in Sinhala, the classroom atmosphere would be more helpful for learning | 12.0 | 32.9 | 37.1 | 13.9 | 4.1 |
| 15 | I feel that it will be more useful if medical terminology related to English classes/courses are introduced under the Medical Faculty English Language Teaching Unit (ELTU) | 33.5 | 38.9 | 14.8 | 7.2 | 5.6 |
Note: 1 – Strongly Agree, 2 – Agree, 3 – Undecided, 4 – Disagree, 5 – Strongly Disagree.
*The term ‘mother tongue’ was used in the adapted questionnaire as this is the term typically used for the first or native language in Sri Lanka.
Table 2. Percentage distribution of overall student responses on the medium of instruction
D. Comparison of Responses Between Pre-clinical and Clinical Students
A significantly higher percentage of students in the clinical years agreed with the statements that they would obtain higher marks answering examination questions in Sinhala (55.8% vs 45.5%, p= .01) and that medical concepts would be better understood if students were provided with textbooks in Sinhala (55.6% vs 51.2%, p = .01), see Table 3.
E. Comparison of Responses of SM Students with EM Students
Of the students who studied O/L in SM, 67.8% opined that it would be better if examinations were held in Sinhala. Among EM students 34.3% agreed with this, while 31.3% were undecided.
Among SM students 51.2% felt that concepts of medicine could be better understood if textbooks were available in Sinhala, among EM students this percentage was 33.7%, the difference was significant (p < .001).
Table 4 summarises the student responses for selected items on the medium of instruction according to their O/L medium.
F. Comparison of Responses of Students Who Obtained ‘A’ Grade for English in GCE O/L, with Those Who Obtained Other Grades
A significantly higher percentage of students with other grades in English opined that exams would be better performed in Sinhala (81.8% vs 58.1%, p< .001) and that medical concepts would be better understood if textbooks were available in Sinhala (70.1% vs 51.2%, p= .001).
It is interesting to note that more than half of the students who got “A” grades for English had also opted for “Exams in Sinhala” and “Textbooks in Sinhala”, 58.1% and 51.2% respectively.
Table 5 summarises distribution of student responses for selected items on the medium of instruction according to their English competency at GCE O/L examination.
| Item No. | Batch | Agree | Undecided | Disagree | Total | ||||
| N | % | N | % | N | % | ||||
| 2 | Pre-Clinical | 188 | 45.5 | 105 | 25.4 | 120 | 29.1 | 413 | χ2 = 9.252 |
| Clinical | 234 | 55.8 | 92 | 22.0 | 93 | 22.2 | 419 | df = 2 | |
| Total | 422 | 50.7 | 197 | 23.7 | 213 | 25.6 | 832 | p = .01 | |
| 4 | Pre-Clinical | 233 | 57.0 | 81 | 19.8 | 95 | 23.2 | 409 | χ2 = 15.585 |
| Clinical | 267 | 65.0 | 92 | 22.4 | 52 | 12.7 | 411 | df = 2 | |
| Total | 500 | 61.0 | 173 | 21.1 | 147 | 17.9 | 820 | p = .000 | |
| 7 | Pre-Clinical | 198 | 48.9 | 94 | 23.2 | 113 | 27.9 | 405 | χ2 = 30.855 |
| Clinical | 279 | 68.0 | 61 | 14.9 | 70 | 17.1 | 410 | df = 2 | |
| Total | 477 | 58.5 | 155 | 19.0 | 183 | 22.5 | 815 | p < .001 | |
| 9 | Pre-Clinical | 210 | 51.2 | 73 | 17.8 | 127 | 31.0 | 410 | χ2 = 9.244 |
| Clinical | 230 | 55.6 | 93 | 22.5 | 91 | 22 | 414 | df = 2 | |
| Total | 440 | 53.4 | 166 | 20.1 | 218 | 26.5 | 824 | p = .01 | |
| 15 | Pre-Clinical | 279 | 67.9 | 67 | 16.3 | 65 | 15.8 | 411 | χ2 = 9.404 |
| Clinical | 314 | 77.0 | 54 | 13.2 | 40 | 9.8 | 408 | df = 2 | |
| Total | 593 | 72.4 | 121 | 14.8 | 105 | 12.8 | 819 | p = .009 |
Table 3. Distribution of student responses for selected items on the medium of instruction according to their stage of clinical training
| Item No. | Medium | Agree | Undecided | Disagree | Total | ||||
| n | % | n | % | n | % | ||||
| 1 | Sinhala | 226 | 34.5 | 128 | 19.5 | 301 | 46.0 | 655 | χ2 = 14.409 |
| English | 38 | 22.8 | 25 | 15.0 | 104 | 62.3 | 167 | df = 2 | |
| Total | 264 | 32.1 | 153 | 18.6 | 405 | 49.3 | 822 | p = .001 | |
| 2 | Sinhala | 396 | 60.0 | 147 | 22.3 | 117 | 17.7 | 660 | χ2 = 140.831 |
| English | 22 | 13.2 | 50 | 29.9 | 95 | 56.9 | 167 | df = 2 | |
| Total | 418 | 50.5 | 197 | 23.8 | 212 | 25.6 | 827 | p < .001 | |
| 4 | Sinhala | 440 | 67.8 | 120 | 18.5 | 89 | 13.7 | 649 | χ2 = 65.973 |
| English | 57 | 34.3 | 52 | 31.3 | 57 | 34.3 | 166 | df = 2 | |
| Total | 497 | 61.0 | 172 | 21.1 | 146 | 17.9 | 815 | p < .001 | |
| 5 | Sinhala | 334 | 50.9 | 160 | 24.4 | 162 | 24.7 | 656 | χ2 = 26.756 |
| English | 54 | 32.5 | 39 | 23.5 | 73 | 44.0 | 166 | df = 2 | |
| Total | 388 | 47.2 | 199 | 24.2 | 235 | 28.6 | 822 | p < .001 | |
| 7 | Sinhala | 406 | 62.4 | 106 | 16.4 | 134 | 20.7 | 646 | χ 2 = 27.467 |
| English | 67 | 40.9 | 49 | 29.9 | 48 | 29.3 | 164 | df = 2 | |
| Total | 473 | 54.4 | 155 | 19.1 | 182 | 22.5 | 810 | p < .001 | |
| 8 | Sinhala | 287 | 44.5 | 163 | 25.2 | 195 | 30.3 | 645 | χ2 = 45.825 |
| English | 35 | 21.1 | 36 | 21.7 | 95 | 57.2 | 166 | df = 2 | |
| Total | 322 | 39.7 | 199 | 24.5 | 290 | 35.8 | 811 | p < .001 | |
| 9 | Sinhala | 380 | 51.2 | 120 | 18.4 | 153 | 23.4 | 653 | χ2 = 31.987 |
| English | 56 | 33.7 | 46 | 27.7 | 64 | 38.6 | 166 | df = 2 | |
| Total | 436 | 53.2 | 166 | 20.3 | 217 | 26.5 | 819 | p < .001 | |
| 11 | Sinhala | 178 | 27.7 | 230 | 35.8 | 235 | 36.5 | 643 | χ2 = 21.245 |
| English | 25 | 15.2 | 48 | 29.3 | 91 | 55.5 | 164 | df = 2 | |
| Total | 203 | 25.2 | 278 | 34.4 | 326 | 40.4 | 807 | p < .001 | |
| 13 | Sinhala | 479 | 74.5 | 96 | 14.9 | 68 | 10.6 | 643 | χ2 = 4.515 |
| English | 113 | 67.7 | 27 | 16.2 | 27 | 16.2 | 167 | df = 2 | |
| Total | 592 | 73.1 | 123 | 15.2 | 95 | 11.7 | 810 | p = .105 | |
| 15 | Sinhala | 463 | 71.6 | 98 | 15.5 | 86 | 13.3 | 647 | χ2 = 1.102 |
| English | 126 | 75.4 | 23 | 13.8 | 18 | 10.8 | 167 | df = 2 | |
| Total | 589 | 72.4 | 121 | 14.9 | 104 | 12.8 | 814 | p = .576 | |
Table 4. Distribution of student responses for selected items on the medium of instruction according to their O/L medium
| Item No. | Grade | Agree | Undecided | Disagree | Total | ||||
| n | % | n | % | n | % | n | |||
| “A” Grade | 224 | 30.9 | 136 | 18.8 | 365 | 50.3 | 725 | χ2 = 5.251 | |
| 1 | Other Grades | 43 | 42.2 | 17 | 16.6 | 42 | 41.2 | 102 | df = 2 |
| Total | 267 | 32.3 | 153 | 18.5 | 407 | 49.2 | 827 | p = .072 | |
| 2 | “A” Grade | 341 | 46.7 | 183 | 25.1 | 206 | 28.2 | 730 | χ2 = 41.553 |
| Other Grades | 81 | 80.2 | 14 | 13.9 | 6 | 5.9 | 101 | df = 2 | |
| Total | 422 | 50.8 | 197 | 23.7 | 212 | 25.5 | 831 | p < .001 | |
| 4 | “A” Grade | 418 | 58.1 | 163 | 22.6 | 143 | 19.3 | 720 | χ2 = 20.625 |
| Other Grades | 81 | 81.8 | 10 | 10.1 | 8 | 8.1 | 99 | df = 2 | |
| Total | 499 | 60.9 | 173 | 21.1 | 147 | 17.9 | 819 | p < .001 | |
| 5 | “A” Grade | 335 | 46.2 | 173 | 23.9 | 217 | 29.9 | 725 | χ2 = 4.854 |
| Other Grades | 56 | 54.9 | 26 | 25.5 | 20 | 19.6 | 102 | df = 2 | |
| Total | 391 | 47.3 | 199 | 24.1 | 237 | 27.6 | 827 | p = .088 | |
| 7 | “A” Grade | 416 | 57.8 | 134 | 18.6 | 170 | 23.6 | 720 | χ2 = 40815 |
| Other Grades | 61 | 64.2 | 21 | 22.2 | 13 | 13.6 | 95 | df = 2 | |
| Total | 477 | 58.5 | 155 | 19.0 | 183 | 22.5 | 815 | p = .09 | |
| 8 | “A” Grade | 265 | 36.8 | 176 | 24.4 | 279 | 38.8 | 720 | χ2 = 30.652 |
| Other Grades | 60 | 63.2 | 23 | 24.2 | 12 | 12.6 | 95 | df = 2 | |
| Total | 325 | 39.9 | 199 | 24.4 | 291 | 35.7 | 815 | p < .001 | |
| 9 | “A” Grade | 372 | 51.2 | 148 | 20.4 | 206 | 28.4 | 726 | χ2=14.318 |
| Other Grades | 68 | 70.1 | 17 | 17.5 | 12 | 12.4 | 97 | df = 2 | |
| Total | 440 | 53.5 | 165 | 20 | 218 | 26.5 | 823 | p = .001 | |
| 11 | “A” Grade | 169 | 23.6 | 238 | 33.3 | 308 | 43.1 | 715 | χ2 = 18.260 |
| Other Grades | 36 | 37.9 | 39 | 41.1 | 20 | 21.1 | 95 | df = 2 | |
| Total | 205 | 25.3 | 277 | 34.2 | 328 | 40.5 | 810 | p < .001 | |
| 13 | “A” Grade | 517 | 72.2 | 109 | 15.2 | 90 | 12.6 | 716 | χ2 = 4.091 |
| Other Grades | 79 | 80.6 | 13 | 13.3 | 6 | 6.1 | 98 | df = 2 | |
| Total | 596 | 73.2 | 122 | 15 | 96 | 11.8 | 814 | p = .129 | |
| 15 | “A” Grade | 525 | 73 | 105 | 14.6 | 89 | 12.4 | 719 | χ2 = 1.456 |
| Other Grades | 67 | 67.7 | 16 | 16.2 | 16 | 16.2 | 99 | df = 2 | |
| Total | 592 | 72.4 | 121 | 14.8 | 105 | 12.8 | 818 | p = .483 | |
Table 5. Distribution of student responses for selected items on the medium of instruction according to their English competency at GCE O/L examination
IV. DISCUSSION
The main objective of this study was to assess the students’ perceptions of the medium of instruction in medical education. It is interesting to note the positive perception shown by the medical undergraduates towards using their native language in the studies.
The majority (more than 90%) of the students entering Peradeniya Medical School are those who performed the best in their GCEA/L examination (University Grants Commission, 2017). Most of these students had studied their ordinary level and advanced level subjects in Sinhala as the medium of instruction (79.5% at GCE O/L and 94.7% at GCE A/L).
Hence, it is not surprising that the change in the instructional language from Sinhala to English in medical school is perceived as a barrier for more than two-thirds of the students (69.2%). This finding is supported by the studies done by Lucas et al. (1997) and Mandal et al. (2012).
A. Acquisition of Knowledge in Medicine
Various studies note a positive correlation between the use of the learner’s first language as a medium of instruction in education and learners’ conceptual development and academic performance in science (Nomlomo, 2007). The use of textbooks for learning medicine is an integral part of the medical curriculum. A study done by Al-Sebaee found that students saved 50% of their time when reading medical textbooks in their first language (as cited in Farhat, 2012).Lucas et al. (1997) found that the English language was a barrier to the acquisition of anatomical knowledge among Hong Kong university students. These studies support the view that the use of students’ first language as the medium of instruction in university education is advantageous for the students in understanding the facts and principles of a subject. How we should use these previous research findings and our own findings need to be explored further so we can support our students to learn more effectively and efficiently.
More than 50% of the students in our study felt that if medical textbooks were available in Sinhala, it would have led to a better understanding of the concepts in medicine. Clinical students felt more strongly about this than the pre-clinical students (p= 0.01, see Table 3). This could possibly be due to the fact that students in the clinical years (having completed at least three years of medical training) are more conversant with the problems encountered when using textbooks written in a language other than their first language. It is also noteworthy that more than 50% of the students who scored an ‘A’ grade for English (GCE O/L) also agreed with this.
The majority of high-income countries in the world use their native language as the medium of instruction in medical education (e.g. UK, US, Germany, France, Japan, Spain, Scandinavian countries; Kozu, 2006; Murray & Dingwall, 2001; Taavitsainen & Pahta, 2003). Furthermore, textbooks and other study materials in medicine are made amply available in their native languages. However, none of the medical textbooks is available in Sinhala, in Sri Lanka. Preparing medical textbooks in Sinhala would require a lot of input from experts in the translation of medical and scientific terms to Sinhala. In this matter the option of adopting English terms “as it is” could be considered, taking example from using Latin terms “as it is” in English and other European medical literature, which should make the task of translation much easier. However it should be noted, students in this study expressed their need to have medical textbooks in their first language. This should not be disregarded or neglected, as this basic educational facility is enjoyed by their counterparts in many other countries.
B. Performance in Examinations
Performances of medical students at medical school depend on many factors (Mandal et al., 2012). The study carried out by Ellili-Cherif and Alkhateeb (2015) indicates that using students’ first language as the medium of instruction positively affects student performance. In our study, more than 50% of students responded that they felt they could obtain higher marks answering examination questions in Sinhala (the first language). The findings are more significant when considering clinical examinations, with 61.0% of all the students responding that they felt they could express their ideas better if the clinical examinations were done in Sinhala. When students with higher English proficiency were analysed separately, it is interesting to note that even among them, 58.1% also agreed with the statement. In Sri Lanka, students have to examine native language speaking patients and gather information using the native language even though the examination is performed in English. Similar issues were raised in the study by Ellili-Cherif and Alkhateeb (2015) where Kuwait university students encountered difficulties when taking examinations in English.
Low level of comprehension of the language of instruction can negatively affect the grasping of the underlying concepts. This may drive students to memorise and regurgitate information, resulting in poor performance in examinations and sub-standard decision making in actual clinical practice, which requires analytical skills based on comprehension of basic concepts (Nyika, 2015).
C. Adopting Sinhala in Medical Education and Integration of Sri Lankan Trained Doctors to Globalised Medicine
English is the main career/business language in Sri Lanka and this is reflected in the fact that none of the medical faculties in Sri Lanka teaches medical sciences in Sinhala.
At this point, it may be pertinent to explore the medical education in Germany where the teaching is exclusively done in German language and the textbooks are in German as well (this is seen in Scandinavia and rest of the Western European mainland as well; Taavitsainen & Pahta, 2003). Yet, the German doctors are able to integrate amicably with the Anglophone scientific community (Simmgen, 2004). The same stands true for the Netherlands and the four Nordic nations (Norway, Sweden, Finland and Denmark) as well (Baker, 2018).
Taking these examples, it is anticipated that the integration of the Sri Lankan trained doctor in globalised medicine should not be a problem as long as their English language proficiency is good. An increasing number of postgraduate trainees in various specialities of medicine fail to go to Anglophone destinations (UK, Australia and New Zealand) for their overseas training as they are unable to achieve the required score in the English language testing systems (e.g. IELTS; Raheem, Medawattegedara, & Miththapala, 2007). This happens irrespective of the fact that they undertook their undergraduate and post-graduate medical education in English. This phenomenon exemplifies the fact that having the English language as the medium of instruction in the medical school and possessing an acceptable level of English language proficiency are entirely two different matters. Thus, learning medicine through first language efficiently, having a good grasp of the principles of medicine, and learning English as a language for communication may be a better way to handle the globalised medicine.
It is also of note that many overseas doctors trained in their first language, practice in Anglophone countries and making excellent career progressions (Simmgen, 2004). This raises questions for medical schools which want to produce ‘global’ doctors, whether the medium of instruction needs to be an ‘international’ language to achieve this purpose. Rather the learning could be in students’ first language, and doctors who want to work internationally could master the language of their chosen destination country.
D. Limitations of the Study
This study describes the experience from a single medical faculty in Sri Lanka (though the majority of those students come through merit basis and represents a wide geographic area of the country). Their English proficiency is at a higher level as well.
The study is confined to students whose first language is Sinhala, yet it represents the large majority of the country.
The present study describes the perceptions of the students. Further studies to look into the actual objective difficulties in learning through a second language are suggested.
V. CONCLUSION
The primary need for successful medical education is to make the students understand key principles and essential facts in medicine. For this to happen smoothly, what is taught should be in a language which the student can comprehend without much additional effort. Thus, strong consideration should be made to utilise the first language in medical education, so that the student of medicine gain the maximum benefit from the education.
This includes having medical textbooks and materials in students’ first language in order to acquire a clear understanding of the basic concepts in medicine.
Notes on Contributors
Dr Thilanka Seneviratne, MD, MRCPCH, ia a consultant paediatrician and senior lecturer in the Department of Pharmacology of Faculty of Medicine, University of Peradeniya. She was involved in conception, design, acquisition of data, analysis, interpretation, drafting and revising the final paper.
Dr Kosala Somaratne, MD, MRCS, FAMS, ia a consultant surgeon working at the Base Hospital, Rikillagaskada. He was involved in conception, design, analysis, interpretation, drafting and critically revising the final version of the paper.
Vindya Alahakoon, BSc; Dilan Bandara, BSc; Deelaka Bandara, BSc; and Randima Munasinghe, BSc, are assistant lecturers at the Department of Pharmacology, Faculty of Medicine, Peradeniya. They were involved in the acquisition of data, analysis, and interpretation, drafting and revising the final paper.
Dr Nabil Ilyas, MBBS, is an intern Medical Officer working at the SBSCH, Peradeniya; Dr Thilini Subasingha, MBBS, is an intern Medical Officer working at the lady Ridgeway Hospital, Colombo. They were involved in the design, acquisition of data and analysis.
Professor P. V. R. Kumarasiri is a Professor in Community Medicine in the Department of Community Medicine, Faculty of Medicine, University of Peradeniya. He was involved in the design, statistical analysis, interpretation and critically revising the paper.
Ethical Approval
Ethical approval was taken from the Ethical Review Committee of Faculty of Medicine, Peradeniya, Sri Lanka (Approval No: 2018/EC/14).
Acknowledgements
Authors acknowledge Dr Abey Rathnayaka, Senior Lecturer in Department of Sociology, University of Peradeniya for his valuable support. Authors would also like to thank the staff of the Department of Pharmacology, Faculty of Medicine, University of Peradeniya.
Funding
There is no funding involved for this paper.
Declaration of Interest
Authors have no conflict of interest.
References
Ahmed, B., Ahmed, L. B., & Al-Jouhari, M. M. (1988). Factors determining the performance of medical students of the Faculty of Medicine, University of Kuwait. Medical Education, 22(6), 506-508.
Al-Mously, N., Salem, R., & Al-Hamdan, N. (2013). The impact of gender and English language on the academic performance of students: An experience from new Saudi medical school. Journal of Contemporary Medical Education, 1(3), 170-176.
Ariyasinghe, S., & Pallegama, R. (2013). Predictors of academic performance of first year dental undergraduates in Sri Lanka: A re-evaluation following curriculum changes. European Journal of Dental Education, 17(1), 57-62.
Baker, C. (2018). NHS staff from overseas: Statistics. Retrieved from http://researchbriefings.files.parliament.uk/documents/CBP-7783/CBP-7783.pdf
Dutcher, N., & Tucker, G. R. (2012).The use of first and second languages in education: A review of international experience.Sydney, Australia: The World Bank.
Ellili-Cherif, M., & Alkhateeb, H. (2015). College students’ attitude toward the medium of instruction: Arabic versus English dilemma. Universal Journal of Educational Research, 3(3), 207-213.
Farhat, D. (2012). Becoming a doctor in Syria: Learning and identity in English for specific purposes at a Syrian university(Doctoral dissertation). Retrieved from http://hdl.handle.net/
10036/3633
Kirkpatrick, A. (2014). English as a medium of instruction in East and Southeast Asian universities. In N. Murray & A. Scarino (Eds.), Dynamic ecologies: A relational perspective on languages education in the Asia-Pacificregion (pp. 15-29). Dordrecht, The Netherlands: Springer.
Kozu, T. (2006). Medical education in Japan. Academic Medicine, 81(12), 1069-1075.
Laguarda, A. I., & Woodward, W. P. (2013). They own this: Mother tongue instruction for indigenous Kuku children in Southern Sudan. School Psychology International, 34(4), 453-469.
Lucas, P., Lenstrup, M., Prinz, J., Williamson, D., Yip, H., & Tipoe, G. (1997). Language as a barrier to the acquisition of anatomical knowledge.Medical Education, 31(2), 81-86.
Lwanga, S. K., & Lemeshow, S. (1991). Sample size determination in health studies: A practical manual. Geneva,Switzerland: World Health Organization.
Mandal, A., Ghosh, A., Sengupta, G., Bera, T., Das, N., & Mukherjee, S. (2012). Factors affecting the performance of undergraduate medical students: A perspective. Indian Journal of Community Medicine: Official Publication of Indian Association of Preventive & Social Medicine, 37(2), 126.
Murray, H., & Dingwall, S. (2001). The dominance of English at European universities: Switzerland and Sweden compared. In U. Ammon (Ed.), Contributions to the sociology of language(pp. 85-112). New York, NY: Mounton de Gruyter.
Narayan, L. (2013). Addressing language barriers to healthcare in India. National Medical Journal India, 26(4), 236-238.
Nomlomo, V. S. (2007). Science teaching and learning through the medium of English and IsiXhosa: A comparative study in two primary schools in the Western Cape(Doctoral dissertation). Retrieved from http://hdl.handle.net/10036/3633
Nyika, A. (2015). Mother tongue as the medium of instruction at developing country universities in a global context. South African Journal of Science, 111(1-2), 01-05.
Raheem, J. R., Medawattegedara, V., & Miththapala, G. (2007). International language assessment and local performance: The case of the Postgraduate Institute of Medicine. OUSL Journal, 4, 3-16.
Simmgen, M. (2004). Why German doctors enjoy British medicine. Clinical Medicine, 4(1), 57-59.
Taavitsainen, I., & Pahta, P. (2003). English in Finland: Globalisation, language awareness and questions of identity. English Today, 19(4), 3-15.
Telmesani, A., Zaini, R. G., & Ghazi, H. O. (2011). Medical education in Saudi Arabia: A review of recent developments and future challenges.Eastern Mediterranean Health Journal, 17(8), 703-707.
University Grants Commission. (2017). Sri Lanka university statistics 2017.Retrieved from https://www.ugc.ac.lk/downloads/
statistics/stat_2017/Chapter%202.pdf
*Thilanka Seneviratne
Department of Pharmacology, Faculty of Medicine,
University of Peradeniya, Sri Lanka 20400
Email: thilanka.medi@gmail.com
Published online: 3 September, TAPS 2019, 4(3), 24-32
DOI: https://doi.org/10.29060/TAPS.2019-4-3/OA2063
Hiroshi Nishigori1, Tomio Suzuki2, Tomoko Matsui3, Jamiu Busari4 & Tim Dornan5
1Centre for Medical Education, Nagoya University Graduate School of Medicine, Japan; 2Department of General Medicine, Osaka Medical College, Japan; 3Department of General Medicine, Nagoya University Graduate School of Medicine, Japan; 4Educational Development and Research Department, Faculty of Health, Medicine and Life Sciences, Maastricht University, The Netherlands; 5Centre for Medical Education, School of Medicine, Dentistry and Biomedical Sciences, Queen’s University Belfast, United Kingdom
Abstract
Introduction: Although retaining a healthy and motivated medical workforce is becoming an intractable problem, the intrinsic motivation that keeps doctors working for patients remains under-investigated. The 2011 Tōhoku earthquake and tsunami provided a unique opportunity for culturally situated research into doctors’ intrinsic motivation. The purpose of this study was to answer the research question: what motivates doctors to work for patients above and beyond expectations?
Methods: This paper reports a qualitative inquiry informed by semi-structured individual interviews with 15 Japanese doctors who had joined disaster relief activities, which uses the Bushidovirtue code as a conceptual framework. The authors read transcripts repeatedly and conducted a cross-case analysis to identify final themes and illustrative narratives.
Results: A young doctor wanted to learn by testing out his capabilities. A senior doctor yearned to be of value to others. Other participants told how identifying with victims motivated them. There were negative as well as positive motivations, exemplified by a participant whose sense that well-educated people had a duty to help was coupled with a wish to avoid being blamed by others.
Discussion: Volunteering met participants’ needs for self-esteem by restoring their relationships with patients to ones in which they had some measure of control. But avoiding being blamed or losing Meiyo(Honour) also motivated physicians to volunteer. Reinforcing the satisfaction of a job well done may help offset the lack of control, guilt, and shame that too easily results from the relentless pressures of workload and external accountability in today’s healthcare systems.
Keywords: Burnout, Bushido, Guilt, Intrinsic Motivation, Narrative Inquiry, Professionalism, Self-esteem
Practice Highlights
- Motivation is a two-edged sword. It both makes doctors work above and beyond expectations and burns them out.
- We clarified five distinct narratives of motivation for doctors to work for patients above and beyond expectations: learning by testing out personal capabilities; being of value to others; identifying with victims; fulfilling ‘the duty of the capable’; and feeling guilty or avoiding blame.
I. INTRODUCTION
Motivation is a two-edged sword. It both makes doctors work above and beyond expectations (Gillespie, Kelly, Duggan, & Dornan, 2017) and burns them out (Dyrbye et al., 2014; Shanafelt, Bradley, Wipf, & Back, 2002). Regulators have responded to high profile instances of unprofessional behaviour by imposing external motivators. These include mandatory continuing professional development, revalidation (Dornan, 2008), and rigorous investigation of alleged poor performance (General Medical Council, n.d.). Extrinsic motivators like these are necessarily negative because they prevent what doctors might do wrong rather than rewarding what doctors do right. Intrinsic motivation to care for patients brought many of today’s doctors into medicine (Ratanawongsa, Howell, & Wright, 2006). But now many of them are burning out and leaving medicine (Dyrbye et al., 2014;Lambert, Smith, & Goldacre, 2018; Shanafelt et al., 2002). Perhaps the burden of practice becomes intolerable when extrinsic, negative motivators dominate over intrinsic, positive ones. A clearer understanding of doctors’ intrinsic motivation could help retain a healthy medical workforce.
Motivation is defined as ‘the psychological feature that arouses you to action toward a desired goal; the reason for the action; that which give purpose and direction to behaviour’ (Princeton University, 2010). Researchers have investigated students’ and doctors’ motivation to learn using a number of psychological constructs. Achievement emotions motivate learners to higher levels of achievement (Artino, La Rochelle, & Durning, 2010; McConnell & Eva, 2012). Epistemic curiosity, self-determination, and self-efficacy motivate them to find answers to questions that arise from group discussion of clinical problems (Schmidt, 1993). Their motivation to work for patients has, however, been less thoroughly investigated than their motivation to learn. And more effort has been made to identify extrinsic than intrinsic motivators, particularly when it comes to retaining physicians in shortage specialties or underserved communities (Hancock, Steinbach, Nesbitt, Adler, & Auerswald, 2009; Larkins & Gupta, 2013; Rafiei, Arab, Rashidian, Mahmoudi, & Rahimi-Movaghar, 2015; Verma et al., 2016). It has been more or less taken for granted, since Hippocrates, that doctors are intrinsically motivated to care selflessly for patients. Research has shown that interacting with patients, rising to the challenge of medicine, and helping patients motivates residents (Mennin, Kalishman, Friedman, Pathak, & Snyder, 1996) but doctors’ intrinsic motivation is still an under-researched topic (Ratanawongsa et al., 2006). We are, as a result, ill-prepared to address doctors’ disillusionment.
One in two US residents (Dyrbye et al., 2014; Shanafelt et al., 2002) and a third of Japanese psychiatric trainees (Tateno et al., 2017) are reported to suffer burnout. Situational causes include long working hours, sleep deprivation, excessive workload, and inadequate support from allied health professionals. Personal causes include family conflicts, isolation, and money problems. Professional causes include information overload and heavy responsibilities for patient care and the supervision of others (Levey, 2001). Efforts have been made to reduce the impact of these extrinsic causes by, for example, restricting duty hours and providing stress management workshops or teaching meditation (West, Dyrbye, Erwin, & Shanafelt, 2016). These have not been uniformly effective (Busireddy et al., 2017). In the case of duty hours, research has shown how doctors’ intrinsic motivation to care for and learn from patients can override their wish to sleep, in which case duty hours restrictions frustrate and demotivate them (Taylor, Nisker, & Lingard, 2013; Taylor, Nisker, Teunissen, Dornan, & Lingard, 2016). Maintaining a motivated, healthy, medical professional workforce is an intractable problem.
Differences in national cultures shed valuable light on medical professionalism (Helmich, Yeh, Kalet, & Al-Eraky, 2017; Jha, Mclean, Gibbs, & Sandars, 2015; Zaidi et al., 2016;). Japan is known for its strong, shared social values and positive work ethic (Wolf, 2013). It has a traditional value system known as Bushido, whose seven principle virtues are shown in Table 1: rectitude (gi), courage (yu), benevolence (jin), politeness (rei), honesty (sei), honour (meiyo) and loyalty (chugi; Nishigori, Harrison, Busari, & Dornan, 2014; Nitobe, 2012). Among these, rectitude (the way of thinking, deciding, and behaving in accordance with reason without wavering), benevolence (encompassing the concepts of love, sympathy, and pity for others), and loyalty (placing the group’s needs above their own needs and interests) motivate doctors to work for others (Nishigori et al., 2014). Japan provides an appropriately rich cultural setting in which to research doctors’ motivation.
| Gi (Rectitude) | The way of thinking, deciding, and behaving in accordance with reason, without wavering it |
| Yu (Courage) | The spirit of daring and bearing
Doing what is right in the face of danger |
| Jin(Benevolence) | Encompasses the concepts of love, sympathy, and pity for others
Recognised as the highest of all the attributes of the human soul “Medicine is a benevolent art” |
| Rei(Politeness) | Respectful regard for the feeling of others |
| Sei (Honesty) | The Chinese character for honesty (sei) combines the characters for “word” and “perfect” |
| Meiyo(Honor) | Recognised as the ultimate pursuit of goodness |
| Chugi(Loyalty) | Placing the group’s needs above their own needs and interest
The interests of the family and the interests of its members are inseparable |
Table 1. Seven virtues in Bushido
On March 11, 2011, an earthquake measuring 9.0 on the Richter scale (the most powerful ever recorded in Japan) and subsequent tsunami devastated the Tōhoku area. This claimed more than 15,000 lives and caused damage to the Fukushima Daiichi Nuclear Power Plant stations, which was one of the greatest nuclear disasters in history. Health workers from all over (and outside) Japan volunteered in great numbers to support victims of the disaster at potential personal cost (Ministry of Health, Labour and Welfare, 2012). This behaviour was recognised within Japan as being motivated by Bushidovalues (Mochizuki, Sakamoto, & Henmi, 2016). The earthquake and tsunami, then, were an ‘experiment of nature’ which provided a unique opportunity to explore doctors’ intrinsic motivation in the context of twenty-first century medicine (Dickerson, 2012). The purpose of this study was to answer the following research question: what motivates doctors to work for patients above and beyond expectations?
II. METHODS
A. Ethical Approval
Ethical approval for all aspects of this study on all sites was granted by the Institutional Review Board at the two lead institutions—the University of Tokyo and Nagoya University Hospital.
B. Setting
After the earthquake and tsunami, more than 12,000 healthcare professionals in more than 2,500 teams went to the Tōhoku region and provided medical support in devastated areas (Ministry of Health, Labour and Welfare, 2012). The teams included ones from the University of Tokyo Hospital (UOTH), Saku Central Hospital of the Nagano Prefectural Federation of Agricultural Cooperatives for Health and Welfare (SAKU), the Primary Care for All Team (PCAT) of the Japan Primary Care Association (JPCA), and from Nagoya University Hospital (NUH). We recruited participants to this study from all four of those teams.
C. Methodology
We chose narrative inquiry as our methodology because we wanted to explore the human meaning of doctors’ motivations as expressed in their own words (Clandinin, Cave, & Berendonk, 2017). This was particularly appropriate in a country with such a strong narrative tradition as Japan, where Murasaki Shikibu wrote the world’s first novel in the 11th century – “The Tale of Genji” (Shikibu, 2006) – and there is a centuries-old tradition of developing so-called Katarimononarratives (Randel, 2003). Narrative inquiry, originating in hermeneutics and phenomenology, is a qualitative research methodology widely used in history, anthropology, and sociology (Bleakley, 2005; Liamputtong, 2013). It is ‘a way of inquiring into experience that attends to individuals’ lives but remains attentive to the larger context and relationships within which lives are nested’ (Clandinin et al., 2017). It generates data in the form of stories, interprets those stories, and represents them in narrative form (Schwandt, 1997). Through thinking not ‘about’ but ‘with’ stories, ‘it strives to preserve the complexity of what it means to be human and to locate these observations of people and phenomena in society, history and time’ (Bleakley, 2005; Josselson, 2006). Relying on the foundational work of philosophers such as Ricoeur, Heidegger, and Husserl (Wertz et al., 2011), narrative inquiry respects a multiplicity of ways of being in the world and the relative nature of truth (Clandinin, 2006). Consistent with this methodological choice, we took a constructivist stance towards the research.
D. Recruitment, Participants, and Data Collection
HN, TS and TM – Japanese general internists, who worked in three health provider organisations named above and teach professionalism – recruited and interviewed participants. One of them (HN) had participated in the Tōhoku disaster relief activities. They used a combination of face-to-face and email communication to invite doctors in organisations that had joined disaster relief activities to participate in the study. HN recruited four participants from the 117 doctors in UOTH who had contributed. TM recruited four participants from the 27 doctors in SAKU who had contributed. TS recruited two participants from the 66 doctors in NUH who had contributed. And, finally, HN and TM, who were members of the JPCA, asked members who had supported victims of the earthquake, of whom five agreed.
After being assured of anonymity and data security, participants gave written informed consent. Between May 2011 and April 2012, we conducted semi-structured individual interviews in the Japanese language with the 15 participants, whose attributes are shown in Table 2. They gave rich, individual accounts, which we judged to provide a sufficient sample for narrative analysis.
The main interview prompts were; 1) “Tell me what your disaster relief activities were like”, and 2) “Why did you provide medical support in Tōhoku?” The first (HN), second (TS), and third (TM) authors interviewed four, two, and 11 participants respectively (HN and TM interviewed two doctors together). They conducted the interviews, which lasted 30 to 90 min, in locations convenient to interviewees (e.g. in a university meeting room or cafe near a train station).
E. Data Analysis
The interviews were audio-recorded and transcribed verbatim immediately afterwards. Subsequently, all three interviewers read transcripts of the interviews they had conducted and performed a preliminary analysis of themes in participants’ narratives (stage 1; Riessman, 2007). Then the first author (HN) read all the transcripts repeatedly, identified themes, and chose an informative set of narratives (stage 2) as defined by these criteria:
- Described participants’ motivation to support earthquake victims.
- Narrated a participant’s individual motivation rather than a general one.
- Was associated with the virtues of Bushido, especially rectitude (Gi), benevolence (Jin), and loyalty (Chugi).
HN translated them into English language at this stage (stage 3) and then conducted a cross-case analysis to identify patterns, which overarched individual narratives (stage 4; Wertz et al., 2011). Then JB and TD (medical doctors and education researchers from two other countries) joined HN in discussing the findings, deconstructing, and reconstructing them (stage 5). The final text with themes and illustrative narratives presented in Results was agreed among the five authors (stage 6).
| Doctor | Postgraduate Year | Organisation* | Interviewer(s)** | Interview Month/Year | Sex | Specialty |
| A | 10 | UOTH | HN | 05/2011 | Female | Nephrology |
| B | 2 | SAKU | HN & TM | 08/2011 | Male | Junior Resident |
| C | 2 | SAKU | TM | 09/2011 | Male | Junior Resident |
| D | 3 | SAKU | TM | 09/2011 | Male | Senior Resident (General Practice) |
| E | 23 | UOTH | HN & TM | 10/2011 | Male | Nephrology |
| F | 18 | UOTH | HN | 10/2011 | Male | Nephrology |
| G | 11 | PCAT | TM | 10/2011 | Male | General Practice |
| H | 10 | PCAT | TM | 11/2011 | Female | Psychosomatic Internal Medicine |
| I | 7 | PCAT | TM | 11/2011 | Male | General Practice |
| J | 11 | UOTH | TM | 01/2012 | Male | Cardiology |
| K | 6 | PCAT | TM | 02/2012 | Male | General Practice |
| L | 4 | SAKU | TM | 02/2012 | Male | Senior Resident (General Practice) |
| M | 4 | PCAT | TM | 03/2012 | Male | Senior Resident (General Practice) |
| N | 18 | NUH | TS | 04/2012 | Male | Nephrology |
| O | 12 | NUH | TS | 04/2012 | Male |
Geriatrics |
*Organisation: UOTH–The University of Tokyo Hospital,
SAKU–Saku Central Hospital of the Nagano Prefectural Federation of
Agricultural Cooperatives for Health and Welfare,
PCAT–Primary Care for All Team by the Japan Primary Care Association,
NUH–Nagoya University Hospital
**Interviewer: HN–Hiroshi Nishigori, TM–Tomoko Matsui, TS–Tomio Suzuki
Table 2. Attributes of the interviewees
F. Reflexivity
Careful attention was paid to the positioning of and relationship between researchers and narrators (Wertz et al., 2011). While collecting the data and analysing them, HN, TM and TS met regularly, discussed, and reflected on their interpretation. They are both deeply versed in Bushidoand used this perspective, reflexively, to inform the selection and interpretation of narratives. They recognised how their positions and values as medical doctors and educators influenced the data analysis; for example, they tended to regard disaster-relief activities as ‘good’ or ‘desired’. When they observed preconceptions of that sort in one another’s interpretations, they drew attention to them. The two non-Japanese authors (JB and TD) helped HN be critically reflexive and explain how their understanding of Bushido informed the analysis.
III. RESULTS
There were five distinct narratives of motivation: learning by testing out personal capabilities; being of value to others; identifying with victims; fulfilling ‘the duty of the capable’; and feeling guilty or avoiding blame. We illustrate them with representative narratives.
Participants were so motivated to support victims that they competed to be team members. One doctor was very disappointed when she was not chosen as a rescue team member.
“[When I applied], I really really wanted to be selected as a team member. However, I turned out to fail… I struggled to find another way [to go to rescue people in Tōhoku]… Though lots of other doctors were also applying to be rescue team members…”
(Doctor A)
Another wanted to provide medical support despite having delivered her baby just before the earthquake occurred.
“At first, I gave up participating in a rescue team because at that time I was taking care of my baby. [So I thought I was not able to go] At least until stopping breast-feeding. So I really envied my colleagues [who were able to visit Tōhoku], when they reported their rescuing activities.”
(Doctor H)
A. Learning by Testing out Personal Capabilities
A positive motivation, particularly for younger doctors, was to find what they were capable of under exceptional circumstances. One participant used these words to explain how disaster relief challenged his personal capabilities:
“On this particular occasion, my involvement in disaster-relief activities was a rare and unusual opportunity to experience something that existed on a higher level… I am sorry to tell you that I went there not to rescue the victims… To be honest, I would like to find out how much I can do.”
(Doctor C)
Another young doctor expressed this positive motivation in terms of curiosity and an opportunity to enhance his clinical competencies.
“I think I went there out of my curiosity… I thought I could gain [various] experiences by visiting Tōhoku area to rescue people… Because I am still a senior resident, I tend to make an appeal, saying, “I can do this sort of thing” or “I acquired that sort of thing”. And I thought that [appeal] was really positive, not negative. This style may be different from that of senior doctors.”
(Doctor M)
B. Being of Value to Others
This is exemplified by the narrative of a senior doctor, who found the defensive style of clinical practice within the current Japanese healthcare system demotivating. Going to support victims of the disaster relieved the sense of stagnation he had in everyday work settings. His yearning for a sense of being of value to others motivated him to go to Tōhoku.
“In my daily clinical practice, the top priority is to avoid making any trouble and manage risk. It was totally different when I was a young resident. At that time, the more I worked for my patients, the more (positive) responses I had got from them… In this sense [as an opportunity to be thanked by patients], I was 100% positive about the idea of going [to the disaster zone]… Such an experience is very rare in our daily clinical activities as healthcare professionals. This could be a motive [for my decision to go to the disaster-struck area].”
(Doctor N)
Another mid-career doctor told how sacrificing himself in order to be of value to others was one of his virtues.
“When I was a high school student, I started thinking of becoming a doctor… Then, after I became a medical student, I believed that self-sacrifice was great.”
(Doctor M)
C. Identifying with Victims
Doctors who had links with the Tōhoku area (for example, those who had been medical students there) were motivated to participate in disaster-relief activities by a sense of identification with Tōhoku. One junior doctor who had graduated from Tōhoku University two years earlier went to rescue victims because his classmates were doing so in areas that he was emotionally attached to.
“I had a special feeling for many of the disaster-struck areas. In addition, about 60 to 70% of my classmates remained in the region, some of who were working at the Japanese Red Cross Ishinomaki Hospital, the Ishinomaki Municipal Hospital, or [hospitals located in] Kesennuma [which were the hub medical institutions around the affected areas]… I was given information on what they were doing [rescuing victims] through Twitter. So I also wanted to do something, which was the biggest motivation…”
(Doctor B)
Another senior doctor who had been to the Tōhoku area several times was motivated by physically feeling the shock-waves in Tokyo.
“Having such a disaster in a nearby location is certainly very different from hearing the news of the earthquake in Haiti [happened in 2010], for example… Even though the value of life does not differ, these two cases are entirely different in terms of their emotional impact [on myself]. [This time, also] At the University of Tokyo, I myself experienced the fierce shaking and many of my colleagues could not return to their homes [because almost all the trains in Tokyo were shut down]. Besides that, some distance away from us, towns I have visited quite a few times in the past were washed away by tsunamis. These invoked a great sense of being close, which, it seems, served as great motivation for me.”
(Doctor E)
D. Fulfilling ‘The Duty of the Capable’
A mid-career female doctor specialising in psychosomatic internal medicine felt obliged to provide medical support because she was competent to do so.
“[When we had the Great Hanshin Earthquake in 1995], I was just a first-year medical student… And many argued for the importance of mental healthcare. I got involved in volunteer activity, but I couldn’t do anything [related to mental healthcare] because I was incompetent, so I felt chagrined… On the other hand, [at the time of Tōhoku earthquake] I’d become a doctor, and had been working as an internist specialising in psychosomatic medicine for a long time. I knew I had expertise [to support people who needed mental healthcare]. So, to me, there’s no way that I wouldn’t go [to rescue victims].”
(Doctor H)
Another senior male doctor who was working at a prestigious Japanese university was driven by his sense that competent or well-educated people had a duty to help.
“To describe my motive in a positive manner, I would say that I had to repay society for the education I had received and the benefits I had enjoyed as a result of that education… It [disaster-relief activity] seemed really tough, but I wanted to go there. In addition, because I have two children, I wanted to show myself behaving honourably to them… I didn’t want to regret not having been there [as a rescue team member]. Also, as I was already not young, I thought I could not take the next opportunity [to go to affected areas to rescue victims of disaster].”
(Doctor E)
E. Feeling Guilty or Avoiding Blame
Doctor E–see immediately preceding–had a negative as well as a positive motivation. He wanted to avoid being blamed by others:
“To describe my motive in a negative manner, I would say that I did not want to be condemned for remaining inactive in spite of my capability to help or being degenerate. In reality, my motive was a combination of the two [the positive one and the negative one].”
(Doctor E)
A senior resident described how the atmosphere of his institution compelled residents to contribute to rescue efforts. Like Doctor E, he went to support victims to shake off feelings of guilt he would have had if he had done nothing.
“Excuse me if I am using improper terms, but there was a mood that condemned non-participating residents [those who did not volunteer to participate in the disaster-relief activities] as being unpatriotic. So I felt I had to respond to the message board [where many residents in Saku Central Hospital wrote on disaster-relief activities] and show my willingness to go [to Tōhoku]. This was my honest feeling… I thought it was too much of a bother. But I was told to be a member for real. I felt it was like a draft notice [when I received the order]. I felt I was being told to go to the front…”
(Doctor D)
IV. DISCUSSION
Narrative accounts of participants’ responses to appalling human suffering caused by the Tōhoku earthquake and tsunami elucidated physicians’ intrinsic motivations to work about and beyond expectations. There were several motivations. One was that disaster relief freed participants from the constraints of their normal working lives. It allowed residents to test their limits and perform beyond them. It allowed senior physicians to be of value to others, unconstrained by fear of litigation. Another motivation was identifying with victims. Physicians rescued sufferers because they were socially connected to the affected area. Another motivation was feeling morally obliged to help victims. The final motivating force is a particularly telling one. Whilst the preceding ones ‘pulled’ participants to volunteer, guilt and fear of blame evoked by an excessive sense of duty ‘pushed’ them to do so. Even outside their usual working situations, some participants were poised between positive and negative motivations.
The analogy between Bushidoand the guilt and fear of blame evoked by participants’ excessive sense of duty makes the final motivating force a telling one. To avoid blame and preserve Meiyo(Honour), ancient Samurai performed ‘Seppuku’, ritual suicide by disembowelment (Nitobe, 2012). Being blamed or losing Meiyo(Honour) may constitute ‘Haji(shame)’ in Japan (Benedict, 2006). Being seized by shame may have motivated doctors to support victims but it might also explain why doctors burn out. Individual psychology suggests we should warn doctors against self-destructive behaviour rather than condone it anticipated (Adler, 2010). One motivation to work for patients above and beyond expectations is wanting to be superior to, or even control other people (Singh, 1991). The earthquake created conditions where doctors were de facto superior to patients. This may have improved participants’ psychological health by meeting ‘esteem needs’ that were unmet in today’s practice (Shergill, 2010). These unmet esteem needs, we suggest, may take a psychological toll that results in doctors’ burnout, dropout, and worse.
An original feature of this study was its use of Bushidoas a theoretical framework. We purposively sampled the Japanese culture because it reconciles personal with communal values in informative ways (Cruess, Cruess, & Steinert, 2010; Ho, Yu, Hirsh, Huang, & Yang, 2011) but this also limits the transferability of our findings. Whilst doctors in any culture might seize opportunities to learn new skills, motivation to escape from the litigious climate of contemporary practice may be greater in developed than developing countries. Another limitation to the transferability of this research is that Bushido(Nitobe, 2012), which is embedded in the Japanese culture, is a virtue ethics code. Among its seven virtues, Chugi(Loyalty) was apparent in participants’ wish to help is a feature of victims with whom they identified. The moral imperative for people with wealth, power, and prestige to help less fortunate people reflects the Bushidovirtues of Gi(Rectitude) and Jin(Benevolence). We cannot assume these virtues transfer to all cultures, though there are parallels with the European code of ‘noblesse oblige’. Further studies in Asia and beyond using specific cultural lenses could clarify the wider applicability of our findings. Whilst the transferability of narrative inquiry to other cultures is also uncertain, this study provides evidence of its usefulness. Perhaps the greatest limitation of this research is that it was better able to clarify participants’ intrinsic motivations than their personal sacrifices. We surmise that rescuing earthquake victims was at a cost to their private lives and home institutions but our data give limited insight into the personal cost of participants’ usual practice.
We propose two themes for further research: 1) doctors’ guilty feelings, and 2) their esteem needs. We suggest that the first should be explored alongside their propensity to burnout and stress, workloads and motivation. Regarding the second, application of individual psychology to future research could give valuable insight into how doctors’ motivation stems from their needs for esteem. We hypothesise that such needs arise from the competitive nature of, for example, gaining entry to medical school. It is paradoxical that competing successfully should motivate doctors to care for others. It is plausible, though, because a competitive spirit might fuel doctors’ esteem needs and lead them to earn admiration from such vulnerable people as earthquake victims.
One implication for educational practice is that medical educators could use doctors’ narratives as a tool to help medical students and residents learn about altruism in medical professionalism. Our findings suggest that doctors from different generations and cultures could usefully explore similarities and differences in their work values and the core values of medicine that underlie them. Finally, we suggest that medical educators who cultivate doctors’ professionalism should think of doctors’ intrinsic motivation to work as a two-edged sword. It can promote altruism, but it can also be evoked by hurtful feelings of guilt that lead to burnout.
Motivation is a two-edged sword. It both makes doctors work above and beyond expectations and burns them out.
Notes on Contributors
Hiroshi Nishigori is a Professor, at the Center for Medical Education, Nagoya University Graduate School of Medicine, Japan.
Tomio Suzuki is a Professor, at the Department of General Medicine, Osaka Medical College, Japan.
Tomoko Matsui is a PhD candidate, at the Department of General Medicine, Nagoya University Graduate School of Medicine, Japan.
Jamiu Busari is an Associate Professor, at the Educational Development and Research Department, Faculty of Health, Medicine and Life Sciences, Maastricht University, The Netherlands.
Tim Dornan is a Professor, at the Centre for Medical Education, School of Medicine, Dentistry and Biomedical Sciences, Queen’s University Belfast, UK.
Ethical Approval
Ethical approval for all aspects of this study on all sites was granted by the Institutional Review Board at the two lead institutions—the University of Tokyo and Nagoya University Hospital.
Acknowledgements
The authors wish to offer their sincere condolences for those who lost their lives in the 2011 Tōhoku earthquake and tsunami. The authors wish to thank all the study participants for contributing to this work.
Funding
This research was supported through a Grand-in-Aid for Scientific Research (KAKENHI), #15H04750, by Japan Society for the Promotion of Science.
Declaration of Interest
The authors declare no conflict of interest.
References
Adler, A. (2010). What life should mean to you.Eastford, CT: Martino Fine Books.
Artino,A. R., La Rochelle, J. S., & Durning, S. J. (2010). Second-year medical students’ motivational beliefs, emotions, and achievement. Medical Education, 44(12), 1203-1212.
Benedict, R. (2006). The chrysanthemum and the sword: Patterns of Japanese culture.Boston, MA: Houghton Mifflin Harcourt.
Bleakley, A. (2005). Stories as data, data as stories: Making sense of narrative inquiry in clinical education. Medical Education, 39(5), 534-540.
Busireddy, K. R., Miller, J. A., Ellison, K., Ren, V., Qayyum, R., & Panda, M. (2017). Efficacy of interventions to reduce resident physician burnout: A systematic review. Journal of Graduate Medical Education, 9(3), 294-301.
Clandinin, D. J. (2006). Handbook of narrative inquiry: Mapping a methodology.London, England: SAGE Publications, Inc.
Clandinin, D. J., Cave, M. T., & Berendonk, C. (2017). Narrative inquiry: A relational research methodology for medical education. Medical Education, 51(1), 89-96.
Cruess, S. R., Cruess, R. L., & Steinert, Y. (2010). Linking the teaching of professionalism to the social contract: A call for cultural humility. Medical Teacher,32(5), 357-359.
Dickerson, P. (2012). Social psychology: Traditional and critical perspectives. Essex, England: Pearson Education Limited.
Dornan, T. (2008). Self-assessment in CPD: Lessons from the UK undergraduate and postgraduate education domains. The Journal of Continuing Education of Health Professions, 28(1), 32-37.
Dyrbye, L. N., West, C. P., Satele, D., Boone, S., Tan, L., Sloan, J., & Shanafelt, T. D. (2014). Burnout among U.S. medical students, residents, and early career physicians relative to the general U.S. population. Academic Medicine, 89(3), 443-451.
General Medical Council. (n.d.). Performance assessments. Retrieved from https://www.gmc-uk.org/concerns/doctors_under_investigation/performance_assessments.asp
Gillespie, H., Kelly, M., Duggan, S., & Dornan, T. (2017). How do patients experience caring? Scoping review. Patient Education and Counseling, 100(9), 1622-1633.
Hancock, C., Steinbach, A., Nesbitt, T. S., Adler, S. R., & Auerswald, C. L. (2009). Why doctors choose small towns: A developmental model of rural physician recruitment and retention. Social Science & Medicine, 69(9), 1368-1376.
Helmich, E., Yeh, H. M., Kalet, A., & Al-Eraky, M. (2017). Becoming a doctor in different cultures: Toward a cross-cultural approach to supporting professional identity formation in medicine. Academic Medicine, 92(1), 58-62.
Ho, M. J., Yu, K. H., Hirsh, D., Huang, T. S., & Yang, P. C. (2011). Does one size fit all? Building a framework for medical professionalism. Academic Medicine, 86(11), 1407-1414.
Jha, V., Mclean, M., Gibbs, T. J., & Sandars, J. (2015). Medical professionalism across cultures: A challenge for medicine and medical education. Medical Teacher, 37(1), 74-80.
Josselson, R. (2006). Narrative research and the challenge of accumulating knowledge. Narrative Inquiry, 16(1), 3-10.
Lambert, T. W., Smith, F., & Goldacre, M. J. (2018). Why doctors consider leaving UK medicine: Qualitative analysis of comments from questionnaire surveys three years after graduation. Journal of the Royal Society of Medicine, 111(1), 18-30.
Larkins, M. S., & Gupta, T. S. (2013). Recruitment and retention of general practitioners in rural Canada and Australia: A review of the literature. Canadian Journal of Rural Medicine, 18(1), 13-23.
Levey, R. E. (2001). Sources of stress for residents and recommendations for programs to assist them. Academic Medicine, 76(2), 142-150.
Liamputtong, P. (2013). Research methods in health. South Melbourne, Australia: Oxford University PressAustralia & New Zealand.
McConnell, M. M., & Eva, K. W. (2012). The role of emotion in the learning and transfer of clinical skills and knowledge. Academic Medicine, 87(10), 1316-1322.
Mennin, S. P., Kalishman, S., Friedman, M., Pathak, D., & Snyder, J. (1996). A survey of graduates in practice from the University of New Mexico’s conventional and community-oriented, problem-based tracks. Academic Medicine, 71(10), 1079-1089.
Ministry of Health, Labour and Welfare. (2012). 東日本大震災への医療面での対応について[Respond to the 2011 Tōhoku earthquake and tsunami]. Retrieved from
http://www.bousai.go.jp/kaigirep/kentokai/tamokutekisen/3/pdf/shiryou1.pdf
Mochizuki, I., Sakamoto, S., & Henmi, K. (2016, June). 医療人のあるべき姿[What healthcare professions should be]. Paper presented at the 66thCongress of Japan Hospital Association, Iwate.
Nishigori, H., Harrison, R., Busari, J., & Dornan, T. (2014). Bushido and medical professionalism in Japan. Academic Medicine, 89(4), 560-563.
Nitobe, I. (2012). Bushido: The soul of Japan. New York, NY: Kodansha International.
Princeton University. (2010). WordNet Search – 3.1 [Word search results]. Retrieved from http://wordnetweb.princeton.edu/perl/webwn?s=motivation
Rafiei, S., Arab, M., Rashidian, A., Mahmoudi, M., & Rahimi-Movaghar, V. (2015). Factors influencing neurosurgeons’ decision to retain in a work location: A qualitative study. Global Journal of Health Science, 7(5), 333-351.
Randel, D. M. (2003). The Harvard dictionary of music. Boston, MA: The Belknap Press of Harvard University Press.
Ratanawongsa, N., Howell, E. E., & Wright, S. M. (2006). What motivates physicians throughout their careers in medicine? Comprehensive Therapy, 32(4), 210-217.
Riessman, C. K. (2007). Narrative methods for the human sciences. London, England: SAGE Publications, Inc.
Schmidt, H. G. (1993). Foundation of problem-based learning: Some explanatory notes. Medical Education, 27(5), 422-432.
Schwandt, T. A. (1997). Qualitative inquiry: A dictionary of terms. London, England: SAGE Publications, Inc.
Shanafelt, T. D., Bradley, K. A., Wipf, J. E., & Back, A. L. (2002). Burnout and self-reported patient care in an internal medicine residency program. Annals of Internal Medicine, 136(5), 358-367.
Shergill, H. K. (2010). Psychology. Delhi, India: PHI Learning.
Shikibu, M. (2006). The tale of Genji. New York, NY: Penguin Classics.
Singh, A. K. (1991). The comprehensive history of psychology. New Delhi, India: Motilal Banarsidass.
Tateno, M., Jovanović, N., Beezhold, J., Uehara-Aoyama, K., Umene-Nakano, W., Nakamae, T., … Kato, T. A. (2017). Suicidal ideation and burnout among psychiatric trainees in Japan. Early Intervention in Psychiatry, 12(5), 935-937.
Taylor, T. S., Nisker, J., & Lingard, L. (2013). To stay or not to stay? A grounded theory study of residents’ postcall behaviors and their rationalizations for those behaviors. Academic Medicine, 88(10), 1529-1533.
Taylor, T. S., Nisker, J., Teunissen, P. W., Dornan, T., & Lingard, L. (2016). Recovery of sleep or recovery of self? A grounded theory study of residents’ decision making regarding how to spend their nonclinical postcall time. Academic Medicine, 91(3), 395-400.
Verma, P., Ford, J. A., Stuart, A., Howe, A., Everington, S., & Steel, N. (2016). A systematic review of strategies to recruit and retain primary care doctors. BMC Health Services Research, 16(1), 126.
Wertz, F. J., Charmaz, K., McMullen, L. M., Josselson, R., Anderson, R., & McSpadden, E. (2011). Five ways of doing qualitative analysis:Phenomenological psychology, grounded theory, discourse analysis, narrative research, and intuitive inquiry. New York, NY: Guilford Press.
West, C. P., Dyrbye, L. N., Erwin, P. J., & Shanafelt, T. D. (2016). Interventions to prevent and reduce physician burnout: A systematic review and meta-analysis. The Lancet, 388(10057), 2272-2281.
Wolf, R. (2013). Management relations in the work culture in Japan as compared to that of the West. Innovative Journal of Business and Management, 2(5), 116-122.
Zaidi, Z., Verstegen, D., Vyas, R., Hamed, O., Dornan, T., & Morahan, P. (2016). Cultural hegemony? Educators’ perspectives on facilitating cross-cultural dialogue. Medical Education Online, 21(1), 33145.
*Hiroshi Nishigori
Centre for Medical Education,
Nagoya University Graduate School of Medicine,
65 Tsurumai-cho, Showa-ku, Nagoya 466-8550, Japan
Tel: +81-52-744-2997
Email: hiroshi.nishigori@gmail.com
Published online: 3 September, TAPS 2019, 4(3), 66-78
DOI: https://doi.org/10.29060/TAPS.2019-4-3/OA2093
Amnuayporn Apiraksakorn1 & Stella Howden2
1Khon Kaen Medical Education Centre, Khon Kaen Hospital, Thailand; 2Centre for Medical Education (CME), School of Medicine, University of Dundee, United Kingdom
Abstract
Peer-assisted learning (PAL) is a common feature of health professions education, characterised as learning from and teaching others who are from a similar background. Evaluations of PAL identify a range of positive outcomes for peer tutors/tutees but rarely address the hidden curriculum, which is a by-product of the learners’ educational experiences, shaped by wider organisational influences and culture. The aim of this case study was to explore the hidden curriculum associated with two modes of PAL used in the final year of an undergraduate medical programme in Thailand: Case Discussions and a Journal Club. A naturalistic evaluation approach, incorporating multiple data sources, was used to explore students’ perspectives on PAL (interviews), student and faculty behaviours during PAL (observation) and the school’s formal/written curriculum (document analysis). Three themes emerged from the thematic analysis of student interviews, triangulated with the observational data (reflecting positive and negative aspects of PAL): 1) developing self as a doctor; 2) learning through dialogue and feedback; and 3) barriers to learning. New insights were gained in relation to the influence of norms and social interactions i.e. recycling materials for Case Discussions and student difficulties with English language journals. Some of the barriers to learning are inherently connected to the study context and recommendations can be made locally for PAL review, however, revealing what is being learned, in the medical habitus, intended and unintended outcomes, highlights the importance of considering the hidden curriculum as an integral part of PAL planning, implementation and evaluation.
Keywords: Peer-assisted Learning, Peer Teaching, Hidden Curriculum, Medical Students, Medical Education
Practice Highlights
- The hidden curriculum can affect all dimensions of an educational system, from what and how students are being taught and what is being learnt in the medical habitus, which then informs the medical curriculum and curricular development.
- New insights into the hidden curriculum associated with Peer-assisted Learning (PAL), in the context of a Thai medical school, are presented.
- By exploring and triangulating data from the written (formal) curriculum, class observations (taught curriculum) and student experiences of PAL in Journal Clubs and Case Discussions, rich data was generated.
- The findings indicated the positive influences of PAL on professional identity formation and developing empathy; difficulties experienced by students in comprehending English language journal articles and dilemmas faced by students when seeking additional feedback.
- The findings in the current study on hidden curriculum highlight the importance of considering the formal, informal, and hidden curriculum as an integral part of curriculum evaluation.
I. INTRODUCTION
Peer-assisted learning (PAL) or peer teaching refers to teaching by people of similar education, background and experience as the students/learners; an instance where neither the tutor nor tutee is a professional teacher (Henning, Weidner, & Jones, 2006; Topping, 1996). In the context of health professions education (e.g. nursing, medicine), PAL is evident at both undergraduate and postgraduate levels and is used to support learning from peers and learning by assuming a teaching/tutor role (Tai, Molloy, Haines, & Canny, 2016). As peer-tutor and tutee are at a similar level of study/training, the teaching-learning strategy is characterised as being collaborative and cooperative, where both parties work and help each other in teaching and learning to their mutual benefit (Henning, Weidner, & Marty, 2008).
Studies of PAL in health professional education have sought to identify the effectiveness and benefits of PAL and commonly investigate the intended learning outcomes and student reactions to PAL. Studies from Asia, Australia, USA and Europe consistently, positively report student acceptance of and learning gains associated with PAL (Awasthi & Yadav, 2015; Cameron, Binnie, Sherriff, & Bissell, 2015; Li, Hua, Chen, Li, & Shi, 2015; Lorio, Florman, Gore, Housley, & Nelson, 2016; McKenna & Williams, 2017; Sahoo, Venkatesan, Myint, & Moe, 2015). These studies are valuable in advancing the understanding of learning associated with PAL, however, they often lack exploration of the hidden curriculum and how that relates to PAL. Commonly used methods of data collection, for example, student self-report and survey methods fail to capture rich data about what is happening, how and why.
Understanding how students experience and are influenced by the hidden curriculum is fundamental work in medical education (Brainard & Brislen, 2007). The hidden curriculum is defined as, “a set of influences that function at the level of organisational structure and culture” (Hafferty, 1998, p. 404). It is proposed that the hidden curriculum has more influence on learners than the formal curriculum (Dewey, 1938; Karimi, Ashktorab, Mohammad, & Abedi, 2014) and is a by-product of educational experiences, related to norms, social interactions and values (Dreeben, 1968; Karnieli-Miller, Vu, Holtman, Clyman, & Inui, 2010; Kentli, 2009; Vallance, 1973). Exploration of the hidden curriculum often involves going beyond learners’ reactions and requires observation of the phenomenon of interest (Gray & Enright, 2018). To date, the hidden curriculum related to PAL in undergraduate medical education remains under investigated and, to the best of the researchers’ knowledge, has not been explored in the Thai, undergraduate medical education context.
The aim of the current study was to explore the hidden curriculum in PAL from the perspective of final year medical students. In this study context, PAL underpins two types of learning activities: Case Discussions (CDs) and the Journal Club (JC) and these are outlined in the Methods section. The findings from this study are anticipated to provide insight into the hidden curriculum embedded in this organisation and culture and how this affects students. The findings will be of interest to those using or planning to use PAL in health professions education and raise awareness of the need to consider the influence of prevailing norms, interactions and commonly held understandings as part of curriculum planning, implementation and evaluation. The research questions addressed by this study are: What are students’ experiences of and attitudes towards PAL; How do students view learning associated with the roles of peer-tutor and peer-tutee; and, How does the formal/written medical curriculum relate to what is observed in PAL?
II. METHODS
A. The Setting and Research Approach
The research approach is a case study with a focus on naturalistic evaluation, where the intent was to judge the value of PAL when examined in its natural (social) context (Yin, 2009). The context was PAL as it operated as a routine part of the final (6th) year studies for medical students at a thousand-bed tertiary care hospital affiliated with Khon Kaen University in Thailand. The curriculum uses a problem-based learning approach with PAL integrated in the clinical years (4thto 6thyear). Final-year medical students are required to be peer-tutors during CDs and JCs. In CDs, the peer-tutor prepares a patient case and presents this to peers (Appendix A) and in the JC the peer-tutor selects a journal article to present (Appendix B). In the final year, there were 47 students in total, with 14 attached to the paediatric placement at the time of data collection. The paediatric PAL activities were selected as the recruitment site as this was the most accessible activity for non-participant observation. This site reflected PAL across other placements sites and the researcher (AA) was a habitual attendee at these PAL sessions, thus minimising disruption of social interactions (Bonner & Tolhurst, 2002). The research approach used multiple sources of data, having an ‘insider’ as PAL observer (Palys, 2003) and relating this to themes developed from student accounts, which supported the generation of rich data as well as strengthening the study authenticity and validity (Miles & Huberman, 1994). A one-to-one interview approach was selected to promote in-depth exploration of individual accounts of learning, connected with their personal teaching tasks. It was also considered that the students, in a group setting, were less likely to share particular accounts. The interviews were an opportunity to capture the differences in experience as well as similarity.
B. Sampling and Recruitment
Purposive sampling (Cohen, Manion, & Morrison, 2013) was used to select participants who were all were final year students attending CDs and JC activities. Using a teaching coordinator to disseminate the information sheet about the study and the consent form was used to minimise any perceived coerciveness of the lead researcher (as the latter was a member of the paediatric faculty). Students had daily contact with the researcher in a teaching environment, enabling questions to be asked of the researcher at any time.
C. Ethical Considerations
As the lead for data collection (AA) was a faculty member, it was established that they had no current or future teaching or assessment responsibilities related to the sample group. Written informed consent was gained from all participants, and assurance given to participants that their participation would remain confidential and they would not be identifiable from any research reports.
D. Data Collection and Analysis
To capture the influence of the hidden curriculum, multiple methods of data collection were used, to gain insight from varied perspectives and enhance the richness of the data (Kuper, Lingard, & Levinson, 2008). One to one, semi-structured interviews (Rubin & Rubin, 2011) with students were used to elicit a focused conversation about PAL experiences (Appendix C). The interviews were audio-recorded, transcribed and translated into English for coding. To ensure translation accuracy multiple samples of anonymous transcript data were subject to ‘forward translation’ between Thai and English by a third party to affirm translation validity (Ozolins, 2009). Multiple non-participant observations of PAL activities, involving the recording of field notes were captured, and these related to the physical environment, participant numbers and patterns of interactions. Documentary analysis involved the review of the formal/written medical curriculum and the handbook for final year students to identify how the PAL activities were represented. Thematic analysis was used to identify, analyse and report themes from the interview data (Braun & Clarke, 2006). This process involved six phases: (1) familiarisation with the data; (2) generation of initial codes; (3) searching for themes; (4) reviewing themes; (5) defining and naming themes; and (6) reporting the themes. Initial coding and theme development were undertaken by the first author, with discussion and review with the second author. Contextual, descriptive analysis was used for the observational data and document analysis. Aligned with the interpretive research approach, it is accepted that the researcher cannot be separated from the findings (Savin-Baden & Major, 2013), however, a number of strategies were used to enhance the study quality and promote trustworthiness, including assuring that the research approach was epistemologically aligned with the research aims; privileging the students’ accounts of their experience and using quotations to support the findings and providing clear information about the context of the study, recruitment and participants (Lincoln & Guba, 1985).
III. RESULTS
A. Presentation of the Results
The results are organised around the themes derived from the interview data and presented as themes and sub-themes, where a theme is a pattern found across the student accounts (Braun & Clarke, 2006). Data from the observations and documentary analysis are integrated with the thematic reporting through identified interconnections, including (dis)connections between the experienced, observed and formal/written curriculum. Quotations from the interviews are presented throughout the results with quotation labels relating to gender (M/F) and the participant identification code, e.g. F1.
B. An Overview of Student Participants and the Data
1) Semi-structured interviews:A total of 14 final-year medical students (100%) in the first paediatric rotation participated in interviews, representing 30% of the year group. The characteristics of the participants are shown in Table 1. The study participants were of a similar age, educational background and ethnicity, and were reflective of the wider, medical student population.
| Final-year medical students (n = 14) | |
| Mean age ± SD (years) | 23.5 ± 0.91 |
| Sex: Male/Female | 5/9 |
| Ethnicity | Thai |
| Entry to medical school | Post high school |
Table 1. Characteristics of study cohort participating in the semi-structured interviews
2) Observations of PAL activities:The researcher (AA) observed 10 PAL sessions. The median and interquartile range (IQR) of participants for the eight CD sessions as well as the number of participants for JCs 1 and 2 in the first paediatric rotation are reported in Table 2. The median duration of the class for the eight CD sessions was 65 minutes (IQR 5). The duration of JC sessions 1 and 2 were 40 and 31 minutes, respectively.
| Types of Participants | Median (IQR) of participants for the 8 Case Discussion sessions | Number of participants for
Journal Club 1 |
Number of participants for
Journal Club 2 |
| Faculty | 4.5 (2) | 1 | 2 |
| Final-year medical students | 10 (2) | 10 | 9 |
| 5th year medical students | 11 (5) | 6 | 0 |
| Interns/residents | 8 (2) | 7 | 9 |
Table 2. Features of PAL sessions
3) Documentary analysis:There was no explicit, written curriculum regarding PAL in the medical curriculum document or the handbook for final year students. However, an outline of the CDs and JC (aligned with the information presented in Appendix A and B) was verbally presented during placement orientation sessions.
C. Students’ Experiences of PAL: Themes and Sub-themes
Three main themes emerged from analysis of the interviews, reflecting positive and negative aspects of PAL: 1) developing self as a doctor; 2) learning through dialogue and feedback; and 3) barriers to learning, see Table 3 for an outline the themes, sub-themes and illustrative quotations.
| Themes | Sub-themes | Illustrative quotations |
| Developing self as a doctor | Increasing confidence and skill as a teacher | When I was in the fourth and fifth year, I just observed the teacher and residents and didn’t feel any direct responsibility for the patient. In the 6th year, I needed to be a senior and leader with respect to [other] students. Sometimes I neglected others’ feeling. I forgot to pay attention to them. Sometimes the patient didn’t want to answer because they may have some private or personal reason. I learned how to be concerned about the feelings of others.”
(F3) |
| Advancing learning skills | “Now when I prepare to teach, I know that I have to master this topic in order to teach others. If I can teach others and help them to understand, that means I understand and I can apply this skill to communicate with others. I now advise my patients using common, non-medical language. I think these are all advantages. I think if I really understand, then I can summarise it in a simple way. I enjoy teaching…”
(F2) |
|
| Learning through dialogue and feedback | Valuing dialogue with peers for learning | “Friends open opportunities to ask questions and we don’t get nervous when friends teach.”
(F9) |
| Tension between wanting (teacher) feedback and concerns about initiating the dialogue | “If I expressed my own opinion, I felt unsure as to whether or not I express myself correctly to the teacher. However, if I talk with friends, I feel free to share my ideas… If the teacher were there; I think if I said something, it could be wrong. So, I kept quiet. Finally, I’m not sure whether I understand or not.”
(F2) |
|
| Barriers to learning | Difficulty with English language journals and statistics | “In [the] journal club, my problem is the interpretation… My problem is about the result which requires the basics of statistics, and [to] know the… methods and vocabulary which I don’t know… If I cannot interpret, I cannot explain to other. If we interpret incorrectly, we can make mistakes.”
(M2) |
| Recycling presentations | “The good point of using copied slides was speed. I did not have to read through all the stuff, but I could read the content related to the copied slides. The bad thing for the peer-tutor was instead of having a full knowledge, by reading and making one’s own slides, [was that] we got more superficial knowledge than our friends.”
(F2) |
|
| Disengagement during PAL | “When someone speaks monotonously, uses uninteresting slides or says the same thing over and over again, I don’t feel like listening at all.”
(M5) |
Table 3. Themes, sub-themes and supporting quotations derived from the student interviews
1) Theme 1 – Developing self as a doctor:Students strongly associated the experience of assuming the peer-tutor role as Increasing Confidence and Skill as a Teacher(sub-theme). This was related to teaching experiences which enhanced awareness of how it feltto be a teacher and a learner. These experiences provoked reflection on their actions as tutor/learner and closer examination of what other teachers (e.g. peers, residents) were doing; seeking out role models. This also acted as a motivator to use teaching strategies which would be effective and engaging. This enhanced tutor/learner empathy extended to considering patients’ experiences of patient-doctor communication and how they were assuming greater responsibilities as a senior student (emerging doctor) which would demand attentiveness to others’ feelings as part of being an effective communicator.
Most students reported they felt increasingly confident to teach others, including junior students, peers and, in time, other healthcare staff. This was associated with practice in the peer-tutor role and receiving supportive feedback from peers and faculty which enhanced feelings of competence and achievement.
Parallel to the emerging sense of becoming a better teacher and communicator, participants also noted that the peer-tutor role was Advancing Learning Skills(sub-theme). Participants highlighted the importance of spending time engaging with the PAL task, searching for and reviewing literature, preparing and practising presentations, understanding these activities as key to mastering the task, as a means of engaging in deeper learning. It was noted by some that this was an important preparation for being more self-directed in learning and was a valuable skill for future practice.
Overall, participants reported that the PAL activities promoted a sense of becoming a doctor, aligned with what they observed in practice (i.e. doctors as educators and teachers). The experience of being a peer-tutor acted as a bridge to understanding their future commitments and the teaching and learning skills required as a medical professional.
2) Theme 2 – Learning through dialogue and feedback:Participants were clear about Valuing Dialogue with Peers for Learning(sub-theme), as they associated PAL with opportunities to enter conversations with peers, before, during and after PAL sessions. They associated this with open and free conversation which allowed them to check their understandings, ask questions as well as build closer relationships with peers as they supported one another in learning. In contrast, participants noted that they often felt a Tension between Wanting (Teacher) Feedback and Concern about Initiating the Dialogue(sub-theme). Although students valued learning from and with one another, they were at times uncertain about their knowledge, reasoning etc. and wanted clarification or guidance from faculty. Where faculty guidance was offered freely in PAL sessions or before a session (e.g. when the faculty member reviewed a presentation) this was valued; although students noted this did not always happen. Generally, students were reluctant to ask staff questions or open a conversation with a faculty member in PAL sessions. This reluctance was attributed to a range of factors, feeling too shy to ask, concerned that their question may be answered by another question, concern that asking questions positioned the questioner as ‘ignorant’ or lacking understanding or concern that questioning may upset the teacher.
Observational data identified that peer-tutees and peer-tutors were particularly active in discussion in the early stages of CDs. However, when faculty asked questions this would often be met with silence (it was noted that there was only one occasion during 10 observation sessions where a student asked a question when prompted by a faculty member). This silence was also evident in the more complex/discursive elements of the CDs activities. The observational data also supported students’ accounts that faculty input was required, as there were two occasions where factually incorrect information was presented, and this was not corrected/identified by staff or students.
3) Theme 3 – Barriers to learning:Participants reported having Difficulty with English Language Journals and Statistics(sub-theme) which were a focal part of the JCs. Concerns about English language proficiency and knowledge of statistics were raised by students as barriers to learning from JCs. This was associated, for some, with feeling anxious when they perceived they could not lead an effective teaching session, based upon their own lack of understanding of the topic and method of analysis.
The majority of participants reported that they had copied presentations from friends, peers and/or the Internet (without including attributions) as part of their preparation for CDs. This was associated with ‘speeding up’ preparation and two reported that this activity had been supported by faculty. The practice of ‘recycling’ presentations and failing to attribute the work to others, but passing it off as their own (Recycling Presentations– sub-theme) was identified by one student (out of 14) as a form of academic dishonesty. A small number of students noted that this practice did diminish their learning when contrasted with developing their own materials and impacted negatively on their capacity to teach.
Observational data confirmed that presentations were used which were either copied from an Internet source or a friend, without relevant attributions. Both instances were revealed when a faculty member asked about the source of the presentation content.
Finally, Disengagement During PAL(sub-theme) represents a range of factors which participants noted impacted upon their interest and attentiveness in PAL sessions; 70% of students noted they have slept in or through a session. Reasons offered for disengagement included: tiredness from being on-call, boredom, topic difficulty, perceived lack of value, monotonous tutor-voice and the temperature of the room.
Observational data corroborated reports of students sleeping, in addition to holding conversations with friends (unrelated to the PAL topic) and using phones. These behaviours were more notable in sessions where there was less interactivity/dialogue between tutors, tutees and teachers. It was also observed that the teaching rooms were often excessively hot, with failing air conditioning systems; the local temperature was around 30ºC to 38ºC. Additional points, not noted by students were that on three occasions there were timetabling clashes, meaning some participants could not attend and up to 70% of the one hour PAL sessions did not start/finish on time (see Table 2).
IV. DISCUSSION
To situate the findings relative to existing PAL literature for health professions education, the discussion is organised as follows: students’ experiences of and learning from PAL; facilitators of learning and barriers to learning.
A. Students’ Experiences of and Learning from PAL
Overall, students were positive about their PAL experiences, in particular, the learning gains from assuming the role of peer-tutor. Similar to other study findings students reported collaborating with peers as helpful in building social relationships in addition to learning from one another in a mutually supportive way (McKenna & Williams, 2017; Tai et al., 2016). Developing skills and confidence as a teacher and communicator and self-directed learner were evident from the literature and this study (Sahoo et al., 2015). In addition, this study highlights the value of PAL in nurturing a sense of empathy for those in teaching and learning roles, extending to an increased awareness of patients’ emotions and perspectives when in a teaching or clinical consultation situation. Making connections to clinical practice may be associated with participants final year status and PAL activities being integrated with workplace-based learning, therefore, promoting reflection on PAL as aiding identity formation as ‘a doctor’. The PAL aims/assessments did not refer to (professional) identity formation, however, the combination of experiential learning, interaction with peers/senior staff, self-reflection and increased attentiveness to ‘good’ teaching role models i.e. observing doctors as teachers/educators, positions PAL, in this context, as supporting the identity formation process (Cruess, Cruess, Boudreau, Snell, & Steinert, 2014). The framing of PAL as a learning experience which shapes professional identity formation may be valuable when considering PAL design, where particular values and behaviours can be explicitly role modelled and conversations about what the ‘medical professional’ as teacher and communicator does, values, thinks, which may promote professional development (Hafferty, 2009).
B. Facilitators of Learning
Similar to other research findings the significance of peer-to-peer dialogue in PAL were significant for learning (Glynn, MacFarlane, Kelly, Cantillon, & Murphy, 2006). As expected, feedback from faculty and the supervisors (see Tables 1 and 2 for the supervisor roles) was also viewed as instrumental, providing reassurance and direction for students. A significant body of literature supports the requirement for faculty as well as peer feedback for learning (Brown, 2015). This was reinforced through the finding that ‘incorrect’ understandings were being shared during the PAL sessions, going unnoticed by faculty and students. In relation to local recommendations, exploration of faculty’s perspectives on the role of faculty in providing feedback for learning – in the context of Peer-assisted (but not peer-alone) Learning may be valuable. In addition, sharing observational data about teaching-moments that appeared to support peer-to-peer dialogue in the sessions may be helpful, as well as highlighting how faculty interjections often halted further student-to-student dialogue. In relation to the organisational commitment to PAL, to support learning, there were multiple positive features identified in this study: protected time for a range of students, trainees and faculty, dedicated space, equipment, scheduling and administration for PAL events, and coordination of peer-tutee/supervisor coupling.
C. Barriers to Learning
As a counterpoint to some of the features which support learning, the influence of unintended organisational and environmental issues may have impacted negatively on the PAL opportunities, e.g. high room temperatures; timetabling clashes and sessions starting and finishing late or being shortened. Some features may be difficult to influence but it may be important to acknowledge these challenges and to assert the importance of PAL, rather than allowing participants to interpret these as (unspoken) indicators of PAL to signal its lack of importance.
Students highlighted the taken for granted practice (transmitted peer-to-peer, and in some cases faculty-to-student) of copying presentations from one another and/or taking materials directly from the Internet to speed the process of preparation for PAL (without attributing the work to its source). Some students acknowledged that this negatively impacted on their capacity to teach as they had not fully engaged with the topic. Although this practice may be considered a form of academic misconduct in some cultures and contexts (Ison, 2018), it requires interpretation in relation to the educational system, which influences knowledge and practice regarding plagiarism (Shirazi, Jafarey, & Moazam, 2010). Gharedaghi et al. (2013) examined the knowledge of medical students regarding plagiarism and found that less than half knew how to reference in PowerPoint slides correctly. Culturally, it may be deemed inappropriate to change information received from friends/peers (to ‘save face’) and to respect (through copying) the words of revered scholars (Nguyen, Terlouw, & Pilot, 2006). However, the practice does present as an opportunity, in PAL, to discuss these issues, the impact on learning, different views globally, which may have particular relevance at a time of greater health professional workforce mobility (Hazelkorn, 2017).
Students’ difficulties with comprehension of English language journals (Hossain, Shamim, Shahana, Habib, & Rahman, 2010; Tar, Tanczos, & Wiwczaroski, 2010) and statistics (Zhang et al., 2012) were reported as barriers to learning and echo study findings from Bangladesh and Hungary and China. This finding prompts questions locally and perhaps more broadly, about the skills required of medical graduates, cultivated during their programme of education and how the curriculum supports those outcomes. If English language proficiency (for medical practice) and statistical knowledge are important, then appropriate support may need to be considered in curricula. The nature of this case study approach enabled comparison between what was expressed in the formal (written) curriculum, the student perspectives on learning (the learned curriculum), and observations of teaching (the taught curriculum). Triangulating this type data, with information about the requirements for practice in a particular setting (Monrouxe et al., 2018) may be valuable in identifying how different curricular facets support/hinder development as a doctor for that context.
Finally, students’ reluctance to initiate a conversation with faculty or ask a question may also be culturally influenced, where faculty members are viewed as being correct, not to be questioned and treated with deference (Nguyen et al., 2006). This, coupled with students concerns about losing face, feeling silly or making others feel uncomfortable may explain this finding in this context. Rather than considering this as something to be changed, it is perhaps apt to ask: what culturally acceptable pedagogical strategies could be used to facilitate students sharing their ideas, uncertainties and questions with faculty to gain useful feedback? An additional question can be raised about the potential affordance of PAL experiences where faculty and more senior trainees are less (or not) present, either as facilitators and/or audience members. Could more student-led and implemented PAL activities enable even richer learning?
D. Study Strengths and Limitations
This is the first study, that we are aware of, exploring the hidden curriculum in PAL using a case study approach in this context. As a single site exploration, which focused on paediatric placement PAL activities, with a sample of only 14 students, readers must exercise caution in transferring findings to their own settings. However, the research approach may inform the development of PAL evaluation in other contexts, drawing upon the ideas of making comparison of the formal/written, taught and lived PAL phenomena, to reveal the hidden curriculum. Future research is also needed to examine the influence of any changes made, associated with study recommendations, seeking to understand more about how the hidden curriculum can be shaped and the impact that may, or may not have upon learning.
V. CONCLUSION
This in-depth study of PAL in a Thai medical school identified positive and negative student experiences and presented new insights about the influence of the hidden curriculum, for example, activity norms and cultural influences. The value of PAL as aiding identity development as a doctor and nurturing teaching/communication skills and the outline of organisational, social and cultural features which facilitated and/or hindered learning will be of interest to curriculum developers. Overall, the study highlights the importance of evaluating or seeking out the influence of the hidden curriculum in PAL to aid curriculum development.
Notes on Contributors
Amnuayporn Apiraksakorn, BPH, LLB, MD, MMEd, AFAMEE, is the Deputy Director of Khon Kaen Medical Education Centre and Deputy Director of Research Centre, Khon Kaen Hospital, Thailand.
Stella Howden, BSc (Hons), MScEd, PhD, SFHEA, is the Associate Dean for Learning and Teaching, School of Medicine, University of Dundee and Senior Lecturer in Medical Education, Centre for Medical Education, UK.
Ethical Approval
This research was granted permission (KE57027) from the Khon Kaen Hospital Institutional Review Board for Human Research (KIRB).
Acknowledgements
The authors thanks (a) the medical students, residents, and my colleagues at Khon Kaen Hospital and Khon Kaen Medical Education Centre for inspiring me to pursue this degree in medical education; (b) the Collaborative Project to Increase Production of Rural Doctor, Ministry of Public Health, Thailand, for funding support; and (c) Mr Bryan Roderick Hamman, Mrs Janice Loewen-Hamman and Dr Patricia Back for proofreading the manuscript.
Funding
This research was supported by a grant from the Collaborative Project to Increase Production of Rural Doctor, Ministry of Public Health, Thailand.
Declaration of Interest
The authors report no conflict of interest. The authors alone are responsible for the content and writing of this article.
References
Awasthi, S., & Yadav, K. K. (2015). Assessment of the acceptance and effectiveness of peer-assisted learning in pediatrics. International Journal of Applied and Basic Medical Research, 5(Suppl 1), 3-6. https://doi.org/10.4103/2229-516x.162253
Bonner, A., & Tolhurst, G. (2002). Insider-outsider perspectives of participant observation. Nurse Researcher,9(4), 7-19. https://journals.rcni.com/doi/abs/10.7748/nr2002.07.9.4.7.c6194
Brainard, A. H., & Brislen, H. C. (2007). Learning professionalism: A view from the trenches. Academic Medicine, 82(11), 1010-1014. https://doi.org/10.1097/01.ACM.0000285343.95826.94
Braun, V., & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3(2), 77-101. https://www.tandfonline.com/doi/abs/10.1191/1478088706qp063oa
Brown, S. (2015). Learning, teaching and assessment in higher education: Global perspectives.London, England: Palgrave-MacMilan.
Cameron, D. A., Binnie, V. I., Sherriff, A., & Bissell, V. (2015). Peer assisted learning: Teaching dental skills and enhancing graduate attributes. British Dental Journal,219(6), 267-272. https://doi.org/10.1038/sj.bdj.2015.722
Cohen, L., Manion, L., & Morrison, K. (2013). Research methods in education. Oxford, England: Routledge.
Cruess, R. L., Cruess, S. R., Boudreau, J. D., Snell, L., & Steinert, Y. (2014). Reframing medical education to support professional identity formation. Academic Medicine, 89(11), 1446-1451. https://doi.org/10.1097/acm.0000000000000427
Dewey, J. (1938). Experience and education: The Kappa Delta Pi lecture series. New York, NY: CollierBooks.
Dreeben, R. (1968). On what is learned in school. Reading, MA: Addison Wesley Publishing Company.
Gharedaghi, M. H., Nourijelyani, K., Sadaghiani, M. S., Yousefzadeh-Fard, Y., Gharedaghi, A., Javadian, P., & Nedjat, S. (2013). Knowledge of medical students of Tehran University of medical sciences regarding plagiarism.Acta Medica Iranica, 51(6), 418-424. Retrieved from http://acta.tums.ac.ir/index.php/acta/article/view/4420/4618
Glynn, L. G., MacFarlane, A., Kelly, M., Cantillon, P., & Murphy, A. W. (2006). Helping each other to learn – A process evaluation of peer assisted learning. BMC Medical Education,6(1), 18.https://doi.org/10.1186/1472-6920-6-18
Gray, A., & Enright, H. (2018). Opening the black box: An observational study of teaching and learning interactions for paediatrics trainees on consultant ward rounds. Journal of Paediatrics and Child Health, 54(9), 1011-1015.
Hafferty, F. W.(1998). Beyond curriculum reform: Confronting medicine’s hidden curriculum. Academic Medicine, 73(4), 403-407. https://doi.org/10.1097/00001888-199804000-00013
Hafferty, F. W. (2009). Professionalism and the socialization of medical students. In R. L. Cruess, S. R. Cruess, & Y. Steinert (Eds.), Teaching medical professionalism: Supporting the development of a professional identity (pp. 53-70). New York, NY: Cambridge University Press.
Hazelkorn, E. (2017). What does global higher education mean for university leaders? London, England: The Leadership Foundation for Higher Education.
Henning, J. M., Weidner, T. G., & Jones, J. (2006). Peer-assisted learning in the athletic training clinical setting. Journal of Athletic Training, 41(1), 102-108.
Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1421493/pdf/i1062-6050-41-1-102.pdf
Henning, J. M., Weidner, T. G., & Marty, M. C. (2008). Peer assisted learning in clinical education: Literature review. Athletic Training Education Journal, 3(3), 84-90. Retrieved from https://www.natajournals.org/doi/pdf/10.4085/1947-380X-3.3.84
Hossain, S., Shamim, K. M., Shahana, N., Habib, M. A., & Rahman, A. (2010). Is English as a medium of instruction problem for undergraduate medical students? Journal of Armed Forces Medical College, Bangladesh,6(2), 32-36. https://doi.org/10.3329/jafmc.v6i2.7272
Ison, D. C. (2018). An empirical analysis of differences in plagiarism among world cultures. Journal of Higher Education Policy and Management, 40(4), 291-304. https://doi.org/10.1080/1360080x.2018.1479949
Karimi, Z., Ashktorab, T., Mohammad, E., & Abedi, H. (2014). Influential factors on learning through the hidden curriculum in the perspective of undergraduate baccalaureate nursing students. Journal of Advances in Medical Education & Professionalism, 2(2), 53-57.
Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4235555/pdf/jamp-2-53.pdf
Karnieli-Miller, O., Vu, T. R., Holtman, M. C., Clyman, S. G., & Inui, T. S. (2010). Medical students’ professionalism narratives: A window on the informal and hidden curriculum. Academic Medicine, 85(1), 124-133. https://doi.org/10.1097/acm.0b013e31
81c42896
Kentli, F. D. (2009). Comparison of hidden curriculum theories. European Journal of Educational Studies, 1(2), 83-88. Retrieved from https://pdfs.semanticscholar.org/7b6d/7275c2c3f5f176ee42d8e661ebdb4683e959.pdf
Kuper, A., Lingard, L., & Levinson, W. (2008). Critically appraising qualitative research. British Medical Journal, 337, a1035.https://doi.org/10.1136/bmj.a1035
Li, C. J., Hua, C. G., Chen, E., Li, S., & Shi, Z. D. (2015). Application of peer-assisted learning in evidence-based dentistry teaching. Shanghai Journal of Stomatology, 24(5), 632-636. Retrieved from https://europepmc.org/abstract/med/26598204
Lincoln, Y. S., & Guba, E. G. (1985). Naturalistic inquiry. Newbury Park, CA: Sage.
Lorio, A. K., Florman, T. M., Gore, J. B., Housley, S. N., & Nelson, M. A. (2016). Power of peer-assisted learning: An interdisciplinary mobility laboratory experience. Journal of Nursing Education,55(2), 83-86. https://doi.org/10.3928/01484834-20160114-04
McKenna, L., & Williams, B. (2017). The hidden curriculum in near-peer learning: An exploratory qualitative study. Nurse Education Today, 50, 77-81. https://doi.org/10.1016/j.nedt.2016.12.010
Miles, M. B., & Huberman, A. M. (1994). Qualitative data analysis: An expanded sourcebook.Thousand Oaks, CA: Sage.
Monrouxe, L. V., Bullock, A., Gormley, G., Kaufhold, K., Kelly, N., Roberts, C. E., … Rees, C. (2018). New graduate doctors’ preparedness for practice: A multistakeholder, multicentre narrative study. British Medical Journal Open, 8(8), e023146. https://doi.org/10.1136/bmjopen-2018-023146
Nguyen, P. M., Terlouw, C., & Pilot, A. (2006). Culturally appropriate pedagogy: The case of group learning in a Confucian Heritage Culture context. Intercultural Education, 17(1), 1-19. https://doi.org/10.1080/14675980500502172
Ozolins, U. (2009). Back translation as a means of giving translators a voice. Translation & Interpreting, 1(2), 1-13. Retrieved from http://trans-int.org/index.php/transint/article/download/38/55
Palys, T. S. (2003). Research decisions: Quantitative and qualitative perspectives.Ontario, Canada: Thomson Nelson.
Rubin, H. J., & Rubin, I. S. (2011). Qualitative interviewing: The art of hearing data. California: Sage.
Sahoo, S., Venkatesan, P., Myint, K. T., & Moe, S. (2015). Peer-assisted learning activities during undergraduate ophthalmology training: How the medical students of Asia Pacific region perceive. The Asia-Pacific Journal of Ophthalmology,4(2), 76-79. https://doi.org/10.1097/apo.0000000000000094
Savin-Baden, M., & Major, H. C. (2013). Qualitative research: The essential guide to theory and practice. Abingdon, England: Routledge.
Shirazi, B., Jafarey, A. M., & Moazam, F. (2010). Plagiarism and the medical fraternity: A study of knowledge and attitudes.The Journal of the Pakistan Medical Association, 60(4), 269-273. Retrieved from https://pdfs.semanticscholar.org/2069/dc0f1fd0366bdc3ebf2526dc068d5f3debef.pdf
Tai, J., Molloy, E., Haines, T., & Canny, B. (2016). Same-level peer assisted learning in medical clinical placements: A narrative systematic review. Medical Education,50(4), 469-484. https://doi.org/10.1111/medu.12898
Tar, I., Tanczos, J., & Wiwczaroski, T. B.(2010). Academic difficulties for L2 medical students in Hungary. English for Specific Purposes World, 30(9). Retrieved from http://www.esp-world.info/Articles_30/TarWiwczaroski.pdf
Topping, K. J. (1996). The effectiveness of peer tutoring in further and higher education: A typology and review of the literature.Higher Education, 32(3), 321-345. https://doi.org/10.1007/bf00138870
Vallance, E. (1973). Hiding the hidden curriculum: An interpretation of the language of justification in nineteenth-century educational reform. Curriculum Theory Network, 4(1), 5-22. https://doi.org/10.2307/1179123
Yin, R. K. (2009). Case study research: Design and methods(4th ed.). Thousand Oaks, CA: Sage.
Zhang, Y., Shang, L., Wang, R., Zhao, Q., Li, C., Xu, Y., & Su, H. (2012). Attitudes toward statistics in medical postgraduates: Measuring, evaluating and monitoring. BioMed Central Medical Education, 12(1), 117. https://doi.org/10.1186/1472-6920-12-117
*Amnuayporn Apiraksakorn
Khon Kaen Medical Education Centre,
Khon Kaen Hospital,
54, 56 Srichan Road, A. Muang,
Khon Kaen 40000, Thailand
Email: a.apiraksakorn@cpird.in.th
Published online: 3 September, TAPS 2019, 4(3), 3-12
DOI: https://doi.org/10.29060/TAPS.2019-4-3/OA2097
Tari Stowers1, Mataroria P. Lyndon2,3, Marcus A. Henning2, Andrew G. Hill3,4& Melinda Webber5
1Faculty of Education, The University of Auckland, New Zealand; 2Centre for Medical and Health Sciences Education, The University of Auckland, New Zealand; 3Counties Manukau District Health Board, New Zealand; 4South Auckland Clinical Campus, The University of Auckland, New Zealand; 5Te Puna Wānanga/School of Māori and Indigenous Education, The University of Auckland, New Zealand
Abstract
Introduction: This study explored motivation among a cohort of New Zealand medical students from The University of Auckland. The research questions were: 1) What motivates students to attend medical school? 2) What are the values, beliefs or cultural practices that influence students’ decisions to go to medical school? 3) How do students’ families influence their decisions to go to medical school?
Methods: Twenty medical students from The University of Auckland in Years Two and Five of a Bachelor of Medicine and Bachelor of Surgery (MBChB) degree participated in semi-structured focus group interviews. Two cohorts of medical students were involved, Māori and Pacific Admission Scheme students (MAPAS), and non-MAPAS students. An interpretive methodology was used, and data analysed using thematic analysis.
Findings: This study found both MAPAS and non-MAPAS students have intrinsic and extrinsic motivation to attend and continue medical school. However, the non-MAPAS students had more individualised motivations to study medicine whereas the MAPAS students were more motivated by collectivism. Family and cultural customs influenced MAPAS students’ motivation to study medicine. Non-MAPAS students were influenced by positive school experiences.
Common to both cohorts was the significant influence of family. Non-MAPAS students specified family members’ professions and educational support as influencing factors. In contrast, MAPAS students identified being motivated to study medicine to improve the financial and health situations of their families.
Conclusion: All students have different motivations for attending medical school which is influenced by their culture and environment. Culture encompasses the individual and their family, inclusive of ethnicity, beliefs, values and behaviours. Family plays a crucial role in motivating and influencing students to pursue medicine.
Keywords: Motivation, Medical Students, Culture, Indigenous, Ethnic Minority
Practice Highlights
- Māori and Pacific ethnic groups are underrepresented in the medical workforce in New Zealand.
- Motivation among medical students is influenced by their socio-cultural environment which is inclusive of family, ethnicity, beliefs and values.
- Māori and Pacific, and non-Māori and Pacific, medical students’ motivation is intrinsic that is, out of interest or enjoyment of learning medicine. On the other hand, their motivation is also extrinsic – out of concern for future financial prospects, prestige, and helping others.
- Family and cultural values have an influence on Māori and Pacific students’ motivation and career choice. This may have influenced these students to take on a more collectivist approach in their motivation to pursue a career in medicine.
I. INTRODUCTION
In New Zealand, a great disparity exists between the population requiring health care and the population providing health care. Māori (indigenous New Zealanders) and Pacific minority ethnic groups are grossly over-represented in poor health outcomes across life expectancy, morbidity, and mortality (Ministry of Health, 2014; Robson & Harris, 2007). The current underrepresentation of Māori and Pacific professionals within the health workforce continues to contribute to these disparities and undermines the efforts of achieving health equity. According to Curtis, Townsend and Airini (2012), Māori make up 15% of the New Zealand population but only 2.6% of doctors, while Pacific people are 7% of the New Zealand population but only 1.6% of doctors. The underrepresentation of indigenous and ethnic minority group health professionals has implications for diversity of health care delivery (Health Workforce Advisory Committee [HWAC], 2006), the processes and outcomes of health care (Smedley, Sith, & Nelson, 2003) and addressing the future health needs of these communities (HWAC, 2006).
The shortage of indigenous and ethnic minority health professionals is not specific to the New Zealand context but is mirrored across the world. Addressing this shortage remains a challenge as the causes are multifactorial and associated with a range of social, cultural, financial, demographic, and academic barriers that can impact on the recruitment and retention of students (Acosta & Olsen, 2006; Curtis & Reid, 2013; Hollow, Davis, Patterson, Olsen, & Baldwin, 2006; Omeri & Ahern, 1999; Thompson, Miller, Thomson, & Dresden, 1993; Zuzelo, 2005). Therefore, to increase the number of Māori and Pacific students studying medicine it is essential to support them in two ways: 1) when they are preparing to enter university and, 2) when they are accepted into medical school. It is critical that they are provided with recruitment, teaching and learning initiatives that are culturally appropriate, provide culturally safe learning environments, and encourage cohort cohesiveness (Curtis et al., 2012). It is also important to better understand what motivates students to study medicine, so we can educate families, schools, and communities on how best to encourage and support each student to achieve their goals, to become a doctor.
Motivation is a concept that provides insights into what leads people to engage in tasks and can vary in level (i.e., how much motivation) and in orientation (i.e., the type of motivation). Self-determination theory is specifically concerned with examining values, intrinsic motivation, development, motivation across cultures, individual differences, and psychological well-being (Reeve, Ryan, & Deci, 2018). Motivation toward learning can range from a motivation through various forms of extrinsic motivation up to intrinsic motivation, which is a preferred motivational orientation for learning. Orientation in motivation involves the core attitudes and goals that contribute to why an individual participates in an activity (Deci & Ryan, 2000a). It is beneficial to have an awareness of these motivational levels and orientations as it can provide valuable insights and explanations into qualitative aspects of how humans function (Deci, 1992), including an individual’s desire to pursue a particular course of learning or profession such as medicine.
Few studies have examined motivational differences across ethnic groups, in particular at a tertiary level and in medical education (Pintrich & Zusho, 2007; Woolf, Cave, Greenhalgh, & Dacre, 2008). Ethnic-based academic achievement differences have been reported in a medical education context, yet exactly how these ethnic groups differ in motivation is rarely investigated (McMarnus, Richards, Winder, & Sproston, 1996; Woolf, Haq, McManus, Higham, & Dacre, 2008). In a review of the literature, Kusurkar, Ten Cate, van Asperen and Croiset (2011) noted motivation among medical students may be influenced by underlying sociodemographic influences. These influences include; age, gender, ethnicity, personality traits, teacher, and parent support. The study acknowledged the significance of the respective cultures and contexts that can influence medical student motivation.
However, research on motivation among medical students remains sparse, with many aspects yet to be further explored – in particular, the ethnic and cultural influences on motivation. Further investigations into this would be beneficial as medical student demographic statistics nationally and internationally have demonstrated wide diversity in ethnic affiliation (Fitzjohn, Wilkinson, Denzil, & Mulder, 2003; Hauer et al., 2008; Woolf, Haq, et al., 2008).
The current study is qualitative and aims to investigate this gap within a New Zealand context by exploring the factors that motivate and influence Māori and Pacific students and how these may differ from non-Māori and Pacific students to attend medical school. Identifying potential differences in motivation may have implications for the recruitment and retention of medical students, curriculum development, teaching and learning methods, and student support services (Lyndon, 2016). The specific research questions were: 1) What motivates students to attend medical school? 2) What are the values, beliefs or cultural practices that influence students’ motivation to attend medical school?
II. METHODS
A. Study Design
This study employed a qualitative approach to research because it focused on participants’ personal perspectives and gathered information on their motivation, values, and influences with regards to studying medicine. In addition, an interpretive methodology was used to examine the insights, experiences, and opinions of participants (Smith & Osborn, 2004).
The study was primarily concerned with collecting rich, descriptive data from medical students at The University of Auckland (UOA). These students expressed their personal perspectives through words and feelings (Cohen, Manion, & Morrison, 2011) regarding what motivated and influenced them to attend medical school.
B. Study Setting
This study was conducted at UOA which offers a Bachelor of Medicine and a Bachelor of Surgery (MBChB) as a six-year undergraduate programme within the Faculty of Medical and Health Sciences. The medical curriculum consists of five years of study that follow on from a premedical year of health sciences or biomedical sciences. The first phase (Years 2 and 3) is considered the ‘pre-clinical’ phase and has a focus on science within clinical medicine; this is followed by the second phase, which is clinically oriented (Years 4 and 5), and the third phase, which prepares the student for the medical workforce (Year 6).
The Faculty of Medical and Health Sciences developed the Māori and Pacific Admission Scheme(MAPAS) initiative which was specifically designed to increase recruitment and retention of Māori and Pacific students to study in health-related fields (Curtis & Reid, 2013). MAPAS provides preferential admission and academic and pastoral support for students of Māori and Pacific ethnicity wanting to pursue careers in health. Data is collected via a data collection agency working within the University system in accordance with confidential protocols and this data is discussed internally amongst senior University staff. Furthermore, MAPAS supports the transition and retention of MAPAS students through their cultural and educational journey to successfully complete and graduate (The University of Auckland, 2016).
C. Study Participants and Procedures
The participants were medical students at UOA, in Years 2 and 5 of the medical programme and were organised into two groups: MAPAS and non-MAPAS. These year levels were specifically selected to gather a range of perspectives from different phases of the medical school programme: the pre-clinical phase (Year 2) and the clinically oriented phase (Year 5).
Year 2 students were notified via email, an online learning portal, and after a lecture or teaching session over a two-week period in October 2013. Year 5 students were notified through their university email over a one-week period in April 2014. Furthermore, snowball sampling was instigated, and this involved recruiting potential participants from among their acquaintances (Walter, 2006). Twenty students in total volunteered to participate in this study.
Participating students were allocated into focus groups based on their admissions criteria and year of study to distinguish the different groups’ perspectives. Four focus groups were conducted: Students were allocated into MAPAS focus groups (Years 2 and 5), while students entering through all other admission pathways were allocated into non-MAPAS focus groups (Years 2 and 5). The non-MAPAS focus groups included participants of New Zealand, European, Indian, and Sri Lankan ethnic groups.
Focus groups took place at UOA and Middlemore Hospital in a neutral, non-threatening area familiar to the students to ensure they felt comfortable (Drever, 1995). Each focus group interview lasted approximately 60 to 90 minutes.
D. Data Collection Methods
Data were collected through a semi-structured focus group interview process in which the researcher had a set of guiding questions but was flexible with the order they were presented. This allowed the interviewees to speak in more depth on the issues raised (Denscombe, 2014) and enabled interesting and unexpected data to emerge (O’Leary, 2014). The focus group interviews in the current study were conducted by study investigators (ML and MH) in a semi-formal manner to build rapport between the researcher and participants (O’Leary, 2014) over a light meal. Before starting participants were given a copy of the questions to be used during the focus group. They were asked to work individually and record personal responses to each question. The rationale was to start at an individual level, to “frontload” participants and give them time to think and share individual experiences free from influence or interruption.
Core activities during the focus group were brainstorming, reflection and exchange of ideas and experiences. During the focus groups, the facilitators encouraged participants to talk freely and to discuss the matters with each other to create an open atmosphere, to foster the exchange of individual experiences and thoughts, and to allow questioning and reconsideration through interaction. All focus group discussions were audiotaped and transcribed for analysis.
E. Data Analysis
The primary source of data was the focus group transcripts, which were transcribed by an independent research assistant for analysis.
The interview transcripts were analysed in NVivo in line with a general inductive approach (Thomas, 2006). The purpose of using the general inductive approach was to condense the textual data into summary findings and to establish the links between the research questions and the summary findings. The researcher, and an independent researcher, read through all the data to obtain a general sense of the information and to reflect on its meaning (Creswell, 2014). This was followed by detailed analysis and a coding process where data was organised into nodes (Rossman & Rallis, 2012) then organised under parent nodes. This involved the researchers re-reading through the transcripts, identifying emerging ideas, and extracting and filing segments of text into the appropriate node groups. This process was completed for each transcript, the initial nodes were used to code data, then additional nodes were added when necessary. Finally, all node groups were examined, refined, and grouped into categories then into subsequent themes. Each theme was organised and reported according to two cohorts: students who identify as MAPAS and students who identify with any other ethnic background (non-MAPAS).
The qualitative reliability procedures undertaken in this study involved checking transcripts against audio recordings to ensure accuracy, cross-checking codes developed by a fellow researcher, and comparing results developed independently (Gibbs, 2007). A final summative check between researchers was performed to verify the trustworthiness of the themes (Creswell, 2014). Member checking procedures with focus group facilitators and a rich, thick description to convey the research findings were also performed to enhance the accuracy of findings.
III. RESULTS
Four themes emerged from the transcripts about their motivation. These themes are outlined below according to this study’s research questions.
A. Question One: What Motivates Students to Attend Medical School?
The themes that emerged within question one of this study were 1) stimulation, engagement and interest, and 2) opportunity.
1) Stimulation, engagement and interest: This theme has links with motivational engagement (Valle et al., 2003). Participants uniformly reported an interest in the sciences and the human body, opportunities for continuous learning, the challenging nature of learning medicine and academic stimulation as reasons for attending medical school.
One participant reported that they hoped “to pursue a career that excited me”while others shared that they “wanted to do something interesting”and studying medicine would “fit well with my interests regarding science and health”. Other participants reported the challenging nature of studying medicine. One participant discussed how the study of medicine had been “hard work”but the educational process had been rewarding. Another shared a similar sentiment, describing medical school as his “biggest challenge yet”. Participants were also drawn to the academically stimulating nature of medicine; one participant highlighted that “you won’t get bored; you’re always learning… because you’re always going to stretch your mind, there’s always more things to know”.
Both cohorts were motivated by the challenges of medical school and found this engaging. MAPAS students were motivated both intrinsically and extrinsically gaining satisfaction from the challenge of medical school. Studying something academically demanding allowed them to demonstrate their interest in a challenge, pursuit of meaning, and the value of hard work. They were also attracted to the academic nature of medical school and the opportunities it provided. On the other hand, challenge for some non-MAPAS students was extrinsic and likened to a competition to gain qualifications. Similarly, non-MAPAS students liked the exploratory challenges presented and uncovering the unknown. MAPAS students’ comments alluded to intrinsic ideals such as enjoying opportunities to learn, whereas non-MAPAS students discussed extrinsic rewards and tangible outcomes. These findings highlighted the influence cultural and class experiences had on their motivation to go to medical school. MAPAS students stated that they strived for a career, which kept their minds engaged. In contrast, non-MAPAS students were interested in the process of acquisition: knowledge, rewards, grades, achievements, community involvement, and progress, suggesting they strived for tangible rewards they could achieve or attain.
2) Opportunity:This theme considers the potential for learning as an augmentation process influencing career goals and life skills (Billett, 2003). Participants described their thoughts about prospects after medical school, especially their need for employment and financial security. One participant voiced that by becoming a doctor, “you have always got job security, and you have almost always got a job”. Another participant spoke of “a life and a future where I don’t have to worry about money is very appealing to me”. In contrast, other participants stated that these factors were less important to them: “I think that these kinds of things are nice perks that you may end up with as a doctor or you may not, but they are definitely not things that led me to the decision towards medicine, they weren’t big factors for me”. Similarly, another participant added, “they are not in it for the money… way more jobs out there for that”.
Participants also voiced the opportunities for a challenging and diverse career. Participants spoke of the “flexibility of the career, where you can go with it, there is no limit to it”. A career in medicine is also perceived as an enabler: “you can go to any country in the world and it is completely translatable”. Along with the flexibility, there is a wide scope for specialisation, including “radiology”, “surgery”, “emergency medicine” and “general practice”.
MAPAS students noted the opportunity medicine provided to look after loved ones and provide security for their families. Many MAPAS students had experienced “going without” material resources and saw the long-term benefits of having a doctor in the family, including the transition towards financial security. They wanted to ensure security for others – most importantly their family. Various students explained their perspectives. Comments included “I know what lack feels like, doing med school will hopefully secure a stable career with good income so I can provide for those around me”; “One of my major motivations was to have a great job that I would enjoy doing the rest of my life that would support my wife and future family”, and “It has… been always built into me that it is my job to look after my… younger siblings… I have always felt responsible for them. This is a way that I can look after my family!”It appeared that the MAPAS students’ efforts to be socially responsive and responsible led to more motivation and commitment to completing their qualification successfully.
Both cohorts were motivated by the options, flexibility, and security attending medical school could provide. MAPAS students appreciated the options, freedom of choice, and how a career in medicine would enable them to look after family and provide security for them. Non-MAPAS students appreciated job and financial security. All students liked that they would not have trouble finding work, debt, or making money. MAPAS students were focused on how medicine would allow them to look after others whereas non-MAPAS students were interested in the financial aspects of medicine and the positive personal implications of this. These findings highlight how cultural and class experiences can influence motivation to pursue medical school. They suggest that MAPAS will do what is necessary to provide for their family, whereas non-MAPAS individuals were motivated by striving for accolades in return for their hard work and effort.
B. Question Two: What Are the Values, Beliefs or Cultural Practices That Influence Students’ Decisions to Go to Medical School?
The themes that emerged within question two of this study were 1) values, beliefs and cultural practices, and 2) prestige.
1) Values, beliefs and cultural practices:Participants reported that attending medical school was personally meaningful and congruent with their personal value systems and beliefs. This included making a difference in people’s lives through service and helping others. However, differences in responses were noted by admission criteria. It was primarily MAPAS students that discussed their aspirations surrounding wanting to provide support for their whānau(family). This desire developed from MAPAS students’ personal experiences observing family members either requiring or providing healthcare assistance. For example, one participant stated, “Definitely it was a good motivator, like, helping other people. Helping your own whānau, I didn’t really see it much before I started – but I see it more now, how bad the health issues are within the whānau… So that is quite a big motivator for me”.
For many MAPAS students, the beliefs and values regarding helping others, especially family, also stemmed from culture and upbringing. One student stated, “In my culture, family is a very important foundation. Growing up in a large family I learnt very quickly about servant leadership as well as caring for others”. Another participant spoke of cultural values, saying “Values can be tied in with a lot of tikanga (customs) I learnt as a kid. Things such as manākitanga (care for others), aroha (compassion), were well ingrained by older generations. Me having a big whānau also helped develop responsibility towards helping others”.
Non-MAPAS participants also placed an emphasis on helping people based on their own beliefs and values: “My own belief that it is important to earn skills which benefits others”. Another participant discussed, “I wanted to do something to help people – to have a big impact on their lives as a career”. It is evident that motivation to succeed, and the pursuit of socially responsible goals, do not function in isolation from each other.
2) Prestige:Another motivating factor, common to both MAPAS and non-MAPAS participants, was the perceived prestige of the medical profession. There was general agreement among participants that medicine is respected, especially within each of their own respective communities, but the associated benefits were for the sake of others rather than themselves. Non-MAPAS students also noted how their prestigious position may be used in a professional capacity to voice concerns of others. A student explained, “I think it is quite nice to know that because people regard you with prestige, you can do a lot with it. You can be a voice for people”. Another non-MAPAS student also noted:
“I think that I will have some prestige as a doctor, but I do not want this for personal benefit but more to use this as an avenue to make change or share my, or others, points of views, as people may listen because I am a doctor and they regard me with prestige.”
Both cohorts were extrinsically motivated acknowledging the notion of prestige. MAPAS students were influenced by prestigious role models and wanted to be role models for others. Similarly, non-MAPAS students liked the idea of being a voice for others. This highlights the importance of role models. Regular interactions with positive role models at home and in professional contexts provide students an example to work towards. In this study, role models provided the students with a sense of having a place of value and importance in the future.
C. Question Three: How Do Students’ Families Influence Their Decisions to Go to Medical School?
The theme that emerged within question three of this study was support.
Both MAPAS and non-MAPAS participants spoke of family influences on their decision to attend medical school because of positive role models and early exposure to the medical profession. One student stated, “My brother did ‘med’, he is the year ahead of me; seeing other people do it gave me the belief that I could do it”. As a result, participants had opportunities to view and be exposed to life within the medical profession. Such insights influenced students to pursue a career in medicine: “My dad is a ‘GP’ (general practitioner), and my brother is a paediatrician, my mum is a practice nurse… I saw what they did, and I liked it”.
Family members also played a supportive role in participants’ intentions to attend medical school. The majority of participants felt no pressure from family members to attend but were rather supportive after the fact: “My family is supportive of my choice to go into medicine but did not choose this path for me. Going to medical school is entirely my decision but my family has been behind me every step of the way”.
Non-MAPAS students also discussed family members in the medical profession. One student shared, “I’ve got three aunts that are midwives and nurses and I’ve got an uncle who’s a surgeon”. Students noted these family members’ involvement had an influence on their decision to attend medical school, but they did not pressure them: “My parents are both involved in the healthcare system. Both were happy with my choice but never pushed me”.
MAPAS students highlighted other forms of support offered by family that influenced and encouraged them to persevere:
“My family understood my desire to be a doctor from a young age. They nurtured this dream of mine and ensured my choices e.g. subject choices, extra-curricular activities and social commitments throughout life were well balanced and aligned with getting me closer towards my dream of being a doctor.”
“My parents play a huge role. They fund my fees and educational resources.”
MAPAS students not only appreciated the support family provided but wanted to be able to return the support after becoming a doctor. Students shared, “It was just my way of looking after the family”; “I wanted a career in which I could earn lots of money to support my own family”, and“It is my duty to gain skills to better look after, support, protect and help my family and friends”.
“From a young age I wanted to be a doctor and that had stemmed from me wanting to look after my grandparents, having been brought up by them a lot of the time”
Students noted support from family influenced their attendance at medical school. Support came in many forms including positive role models who led by example, experiences that ignited curiosities, as well as financial support during their time at medical school. MAPAS students described having medical professionals within their families. These family members were positive role models, providing opportunities to observe and experience life within the medical profession vicariously. Such insights ignited curiosities and influenced students to pursue a career in medicine.
Family members from both cohorts willingly supported students, nurturing their curiosities and encouraging them to pursue their aspirations. Medical professionals in MAPAS families modelled work ethic and commitment: in some instances, what will be expected in the future. Non-MAPAS families modelled career options, free from pressure and expectation. These findings highlight the underlying expectation of Māori and Pacific community members to care and provide for those around them, an added extrinsic motivator. In some instances, the family placed the expectation upon the student; for others, it was adopted by the students themselves.
IV. DISCUSSION
This study investigated factors that motivate and influence students to attend medical school. Identifying these factors is an important step in helping increase the number of indigenous and ethnic minority health professionals.
The first major finding of the study was both MAPAS and non-MAPAS students have intrinsic and extrinsic motivation to attend and continue medical school. However, the non-MAPAS students tended to be motivated by positive experiences at school, and the MAPAS students were motivated by family influences. In the context of Self Determination Theory (Deci & Ryan, 2000b), the non-MAPAS students in this study were intrinsically motivated, engaging in educational experiences out of enjoyment and interest (Deci & Ryan, 2000b). These educational experiences align with students’ interests in further developing, refining, and increasing their knowledge of science-related phenomena. Other literature has also suggested that students pursue medicine because of interest in learning (Salem et al., 2013), science and people (Lempp & Seale, 2006).
In contrast, many of the MAPAS students in this study were extrinsically motivated by their family to attend medical school. These students experienced integrated regulation; behaviour was self-determined and personally important because of the valued outcomes (Deci, Vallerand, Pelletier, & Ryan, 1991). Students wanted to be able to use their medical knowledge to help ill family members and to be financially secure and able to provide for their family in the future. These intentions are likely to relate to cultural values of communitarianism, reciprocity, respect, spirituality, and family (The Ministry of Pacific Island Affairs, 1998).
However, these intentions may also be influenced by other factors, including underlying sociodemographic influences (Korkmaz & Şenol, 2010; Pastor et al., 2009). In New Zealand, disparities in socioeconomic status between Māori and Pacific populations and other New Zealanders persist, and therefore, it is possible these differences may also be present in the medical student population (Marriott & Sim, 2014). Socio-economic factors are thus one pathway through which ethnic differences in motivation may potentially be mediated.
The next major finding of the study was the tension between individualism, collective service and cultural obligation. The non-MAPAS students were encouraged by family to be independent and given educational autonomy to pursue individual interests. The individualistic perspectives of the non-MAPAS students led them to have an independent view, seeing themselves separate from others and defined by their personal traits and characteristics (Hooper, 2015). In contrast, the MAPAS students came from backgrounds where individuals are considered part of a collective, who work together to support each other. This may have influenced these MAPAS students to take on a more collectivist approach in their motivation to pursue a career in medicine. These findings highlight and confirm differences in cultural influences and perspectives. Each perspective is a unique representation of the participants’ circumstances.
Finally, this study identified how familial influences have a significant impact on student motivation and career choice. Family members were alluded to as either role models who inspired students through their actions, examples to learn vicariously from, or authoritarians who specified the direction students must take. With regards to SDT, family members were a source of extrinsic motivation, by motivating students through their actions. However, the type of extrinsic regulation would vary depending on whether students perceived family influences as controlling or autonomy supportive.
The differences in student motivation have implications for recruiting students into medical school. Recruitment schemes must be tailored to suit the various motivational profiles of students. Understanding these motivations can help to customise support initiatives for students (Kusurkar, Croiset, Galindo-Garre, & Ten Cate, 2013). For Māori and Pacific recruitment, a collectivist approach could be used, incorporating their communities in this process, helping them to best support the individual throughout their study so they may remain motivated, experience success, and return to their community with new knowledge and skills to share. It would also be beneficial to help families, in particular, Māori and Pacific, to understand the importance of their role and how it influences the careers, attitudes, actions, and learning for their children.
A. Future Research Directions
It would be valuable to gain insights on what motivates and influences students from a wider range of ethnicities or cultures to pursue medicine. Perspectives such as age, gender, number of years into medical degree, and relationship status should also be used when considering this data because it is clear from this study that class and culture can influence student perspectives and motivations.
B. Limitations
This study was conducted in a large multicultural university in New Zealand’s largest city. However, this study has limitations. It was conducted at one university using a small sample of students from two cohorts. The semi-structured focus group interviews used only a single set of questions to extract students’ ideas on what motivated and influenced them to attend medical school. The findings of this study may not represent the wider population; therefore, caution must be taken when trying to generalise the results. However, the findings do contribute to the wider conversation about student motivation and influences when pursuing health careers.
V. CONCLUSION
Medical students have intrinsic and extrinsic motivation for attending medical school which can be influenced by their culture and environment. Family and cultural values heavily influenced motivation among MAPAS students. MAPAS students and their families come from collectivist cultures committed to helping others. In contrast, non-MAPAS families helped students become immersed in education and engage in positive learning experiences, which non-MAPAS students found motivating. The common thread throughout this study was the role of family. Family plays a crucial role in motivating and influencing all students to pursue medicine.
Notes on Contributors
Tari Stowers (BEd) is of Ngāti Hau descent and is a Master of Education Candidate in the Faculty of Education, The University of Auckland, New Zealand.
Mataroria P. Lyndon (MBChB, MPH, PhD) is of Ngāti Hine, Ngāti Whātua and Waikato descent; and a Senior Lecturer in Medical Education in the Centre for Medical and Health Sciences Education, The University of Auckland; and Lead Clinical Advisor Māori Health at Counties Manukau District Health Board, New Zealand.
Marcus A. Henning (PhD, MA, MBus) is an Associate Professor in the Centre for Medical and Health Sciences Education, The University of Auckland.
Andrew G. Hill (MBChB, MD, EdD, FRACS) is a Professor of Surgery and Head of South Auckland Clinical Campus, The University of Auckland.
Melinda Webber (PhD, MEd) is of Ngāti Whakaue, Ngāpuhi, Ngāti Kahu descent; and an Associate Professor in Te Puna Wānanga/School of Māori and Indigenous Education at The University of Auckland.
Ethical Approval
Ethics approval was granted by the University of Auckland Human Participants Ethics Committee (UAHEPC 9827).
Funding
No funding is involved for this paper.
Declaration of Interest
There is no conflict of interest.
References
Acosta, D., & Olsen, P. (2006). Meeting the needs of regional minority groups: The University of Washington’s programs to increase the American Indian and Alaskan Native physican workforce. Academic Medicine, 81(10), 863-870.
Billett, S. (2003). Vocational curriculum and pedagogy: An activity theory perspective. European Educational Research Journal, 2(1), 6-21.
Cohen, L., Manion, L., & Morrison, K. (2011). Research methods in education(7th ed.). New York, NY: Routledge.
Creswell, J. (2014). Research design: Qualitative, quantitative, and mixed methods approaches(4th ed.). Thousand Oaks, CA: SAGE Publications Ltd.
Curtis, E., & Reid, P. (2013). Indigenous health workforce development: Challenges and successes of the Vision 20:20 programme. ANZ Journal of Surgery, 83(1-2), 49-54.
Curtis, E., Townsend, S., & Airini. (2012). Improving indigenous and ethnic minority student success in foundation health study. Teaching in Higher Education, 17(5), 589-602.
Curtis, E. T., Wikaire, E., Lualua-Aati, T., Kool, B., Nepia, W., Ruka, M., … Poole, P. (2012). Tātou tātou/Success for all: Improving Māori student success. Retrieved from https://ako.ac.nz/assets/Knowledge-centre/NPF-08-002-Tatou-Tat
ou-Success-for-all-Improving-Maori-student-success/52178cfd54/
RESEARCH-REPORT-Tatou-Tatou-Success-For-All-Improving-Maori-Student-Success.pdf
Deci, E. (1992). On the nature and functions of motivation theories. Psychological Science, 3(3), 167-171.
Deci, E., & Ryan, R. (2000a). Intrinsic and extrinsic motivations: Classic definitions and new directions. Contemporary Educational Psychology, 25(1), 54-67.
Deci, E., & Ryan, R. (2000b). Self-determination theory and the facilitaion of intrinsic motivation, social development, and well-being. American Psychologist, 55(1), 68-78.
Deci, E., Vallerand, R., Pelletier, L., & Ryan, R. (1991). Motivation and education: The self-determination perspective. Educational Psychologist, 26(3), 325-346.
Denscombe, M. (2014). The good research guide: For small-scale social research projects(5th ed.). New York, NY: Open University Press.
Drever, E. (1995). Using semi-structured interviews in small-scale research: A teacher’s guide. Glasgow, Scotland: The Scottish Council for Research in Education.
Fitzjohn, J., Wilkinson, T., Denzil, G., & Mulder, R. (2003). The demographic characteristics of New Zealand medical students: The New Zealand wellbeing, intentions, debt and experiences (wide) survey of medical students 2001 study. The New Zealand Medical Journal, 116(1183), U626.
Gibbs, G. (2007). Analyzing qualitative data. London, England: SAGE Publications, Ltd.
Hauer, K., Durning, S., Kernan, W., Fagan, M., Mintz, M., O’Sullivan, P., … Schwartz, M. (2008). Factors associated with medical students’ career choices regarding internal medicine. Journal of the American Medical Association, 300(10), 1154-1164.
Health Workforce Advisory Committee. (2006). Report of the health workforce advisory committee on encouraging Māori to work in the health professions. Retrieved from http://www.moh.
govt.nz/NoteBook/nbbooks.nsf/0/DDFEB84C5B24BD31CC2576B20004C8F4/$file/EncouragingMaoritoWorkintheHealthProfessions.pdf
Hollow, W., Davis, G., Patterson, D., Olsen, P., & Baldwin, L. (2006). American Indians and Alaska Natives: How do they find their path to medical school? Academic Medicine, 81(10), 65-69.
Hooper, E. (2015, January 30). Individualist or collectivist? How culture influences behavior [Social network blog post]. Retrieved from https://healthypsych.com/individualist-or-collectivist-how-culture-influences-behavior/
Korkmaz, H., & Şenol, Y. Y. (2010). The characteristics of medical students and motivation towards career choice: Implications for curriculum. Hacettepe University Journal of Education, 28(1), 258-268.
Kusurkar, R., Croiset, G., Galindo-Garre, F., & Ten Cate, O. (2013). Motivational profiles of medical students: Association with study effort, academic performance and exhaustion. BMC Medical Education, 13(1), 87.
Kusurkar, R., Ten Cate, O., van Asperen, M., & Croiset, G. (2011). Motivation as a dependent and independent variable in medical education: A review of the literature. Medical Teacher, 33(5), 242-262.
Lempp, H., & Seale, C. (2006). Medical students’ perceptions in relation to ethnicity and gender: A qualitative study. BMC Medical Education, 6, 17. https://doi.org/10.1186/1472-6920-6-17
Lyndon, M. P. (2016). The impact of a medical curriculum on motivation and well-being among medical students (Doctoral dissertation). Retrieved from http://hdl.handle.net/2292/29918
Marriott, L., & Sim, D. (2014). Indicators of inequality for Māori and Pacific people. Retrieved from https://www.victoria.ac.nz/
sacl/centres-and-chairs/cpf/publications/working-papers/WP09_2
014_Indicators-of-Inequality.pdf
McMarnus, I., Richards, P., Winder, B., & Sproston, K. (1996). Final examination performance of medical students from ethnic minorities. Medical Education, 30(3), 195-200.
Ministry of Health. (2014). Ala Mo’ui: Pathways to Pacific health and wellbeing 2014–2018. Retrieved from https://www.health.govt.nz/publication/ala-moui-pathways-pacific-health-and-wellbeing-2014-2018
O’Leary, Z. (2014). The essential guide to doing research(2nd ed.). London, England: SAGE Publications Ltd.
Omeri, A., & Ahern, M. (1999). Utalising culturally congruent strategies to enhance recruitment and retention of Australian Indigenious nursing students. Journal of Transcultural Nursing, 10(2), 150-155.
Pastor, Á., López-Roig, S., Sánchez, S., Hart, J., Johnston, M., & Dixon, D. (2009). Analysing motivation to do medicine cross-culturally: The international motivation to do medicine scale. Escritos de Psicología, 2(2), 3-9.
Pintrich, P., & Zusho, A. (2007). Student motivation and self-regulated learning in the college classroom. In R. Perry & J. Smart (Eds.), The scholarship of teaching and learning in higher education: An evidence based perspective(pp. 731-810). Dordrecht, The Netherlands: Springer.
Reeve, J., Ryan, R., & Deci, E. (2018). Sociocultural influences on student motivation as viewed through the lens of self-determination theory. In D. M. McInerney & G. A. D. Liem (Eds.), Big theories revisited 2: Research on sociocultural influences on motivation and learning (pp. 15-40).Greenwich, CT: Information Age Publishing.
Robson, B., & Harris, R. (Eds.). (2007). Hauora: Māori standards of health IV: A study of the years 2000-2005. Retrieved from https://www.otago.ac.nz/wellington/departments/publichealth/research/erupomare/research/otago019494.html
Rossman, G., & Rallis, S. (2012). Learning in the field: An introduction to qualitative research(3rd ed.). Thousand Oaks, CA: SAGE Publications Ltd.
Salem, R. O., Al-Mously, N., Nabil, N. M., Al-Zalabani, A. H., Al-Dhawi, A. F., & Al-Hamdan, N. (2013). Academic and socio-demographic factors influencing students’ performance in a new Saudi medical school. Medical Teacher, 35(sup1), S83-S89. https://doi.org/10.3109/0142159X.2013.765551
Smedley, B., Sith, A., & Nelson, A. (2003). Unequal treatment confronting racial and ethnic disparities in health care. Washington, DC: National Academy Press.
Smith, J. A., & Osborn, M. (2004). Interpretative phenomenological analysis. In G. M. Breakwell (Ed.), Doing social psychology research(pp. 229-254). Malden, MA: Blackwell Publishing.
The Ministry of Pacific Island Affairs. (1998). Pacific analysis framework with Pacific consultation guidelines: Analysing public policy through Pacific lenses. Retrieved from http://www.moh.govt.nz/notebook/nbbooks.nsf/0/0C0F5D6D16FA75FFCC256CE6007B97BC/$file/Pacific_analysis_framework.pdf
The University of Auckland. (2016). About MAPAS. Retrieved from https://www.fmhs.auckland.ac.nz/en/faculty/for/future-under
graduates/maori-and-pacific-admission-scheme.html
Thomas, D. R. (2006). A general inductive approach for analyzing qualitative evaluation data. American Journal of Evaluation, 27(2), 237-246. http://dx.doi.org/10.1177/1098214005283748
Thompson, B., Miller, L., Thomson, W., & Dresden, J. (1993). Evaluating magnet schools for the health professions: Career aspirations of hispanic and non-minority students. Retrieved from https://eric.ed.gov/?id=ED360457
Valle, A., Cabanach, R. G., Núnez, J. C., González-Pienda, J., Rodríguez, S., & Piñeiro, I. (2003). Multiple goals, motivation and academic learning. British Journal of Educational Psychology, 73(1), 71-87. http://dx.doi.org/10.1348/000709903762869923
Walter, M. (Ed.). (2006). Social research methods: An Australian perspective. Oxford, England: Oxford University Press.
Woolf, K., Cave, J., Greenhalgh, T., & Dacre, J. (2008). Ethnic stereotypes and the underachievement of UK medical students from ethnic minorities: Qualitative study. British Medical Journal, 337, a1220.
Woolf, K., Haq, I., McManus, I., Higham, J., & Dacre, J. (2008). Exploring the underperformance of male and minority ethnic medical students in first year clinical examinations. Advances in Health Sciences Education, 13(5), 607-616.
Zuzelo, P. (2005). Affirming the disadvantaged student. Nurse Educator, 30(1), 27-31.
*Mataroria Lyndon
Private Bag 92019,
Auckland 1142, New Zealand
Tel: +64 (0) 9 923 6235
Email: mataroria.lyndon@auckland.ac.nz
Announcements
- Best Reviewer Awards 2024
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2024.
Refer here for the list of recipients. - Most Accessed Article 2024
The Most Accessed Article of 2024 goes to Persons with Disabilities (PWD) as patient educators: Effects on medical student attitudes.
Congratulations, Dr Vivien Lee and co-authors! - Best Article Award 2024
The Best Article Award of 2024 goes to Achieving Competency for Year 1 Doctors in Singapore: Comparing Night Float or Traditional Call.
Congratulations, Dr Tan Mae Yue and co-authors! - Fourth Thematic Issue: Call for Submissions
The Asia Pacific Scholar is now calling for submissions for its Fourth Thematic Publication on “Developing a Holistic Healthcare Practitioner for a Sustainable Future”!
The Guest Editors for this Thematic Issue are A/Prof Marcus Henning and Adj A/Prof Mabel Yap. For more information on paper submissions, check out here! - Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Volume 9 Number 1 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors. - Volume 8 Number 3 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2021
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2021.
Refer here for the list of recipients. - Most Accessed Article 2021
The Most Accessed Article of 2021 goes to Professional identity formation-oriented mentoring technique as a method to improve self-regulated learning: A mixed-method study.
Congratulations, Assoc/Prof Matsuyama and co-authors. - Best Reviewer Awards 2020
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2020.
Refer here for the list of recipients. - Most Accessed Article 2020
The Most Accessed Article of 2020 goes to Inter-related issues that impact motivation in biomedical sciences graduate education. Congratulations, Dr Chen Zhi Xiong and co-authors.









