
Issue 48
Nov 2023
AFFAIRS OF THE HEART
By Dr Hayang Yang, Research Fellow, Cardiovascular Metabolic Disease Translational Research Programme, NUS Yong Loo Lin School of Medicine (NUS Medicine), Mr Shaun Loong, Final year medical student, NUS Medicine, Dr PL Soong, Senior Research Fellow, Cardiovascular Metabolic Disease Translational Research Programme, NUS Medicine, Dr Mayank Dalakoti, Associate Consultant Cardiologist, Ng Teng Fong Hospital, Clinical Lead, Cardiovascular Metabolic Disease Translational Research Programme, NUS Medicine, Professor Josip Car, Head of School of Life Course and Population Sciences, King’s College London, Visiting Professor of Medicine, Cardiovascular Metabolic Disease Translational Research Programme, NUS Medicine, Professor Wang Wenru, Professor of Medicine, Alice Lee Centre for Nursing Studies and Cardiovascular Metabolic Disease Translational Research Programme, NUS Medicine, and Professor Roger Foo, Zayed bin Sultan Al-Nahyan Professor of Medicine and Director, Cardiovascular Metabolic Disease Translational Research Programme, NUS Medicine
Cardiovascular disease (CVD) killed over 26,000 Singaporeans in 20221. Most people discover they have the disease only when symptoms present. Many others remain unaware, their latent illness undetected. Now, a nation-wide study involving clinicians and scientists from Singapore’s two national heart centres, the Agency for Science, Technology and Research as well as international partners aims to track and map the causes, scale and extent of cardiovascular ill health in Singapore and Southeast Asia. The research team will also aim to identify disease markers and use Artificial Intelligence (AI) to develop tools that can detect and prevent CVD.
Cardiovascular disease (CVD) is the leading cause of death and illness worldwide. Its prevalence is surging, largely fuelled by a rise in obesity and other heart-related risk factors2,3. Large resources, spanning across decades, have been invested in the research of established CVDs (heart failure, myocardial infarction and stroke). However, in the current age of personalised preventive medicine, the more ambitious challenge will be to identify and tackle early drivers of CVDs, with the aim of arresting CVD development or progression before the manifestation of any symptoms.
Launched by Minister of Health Ong Ye Kung on 27 September 2023, Project RESET (“Redirecting immune, lipid and metabolic drivers of early cardiovascular disease”) is a recently awarded Singapore National Medical Research Council (NMRC) Large Collaborative Grant (LCG). This project brings together our nationwide community of cardiovascular, metabolic, data science and digital health researchers, as well as clinicians across primary and tertiary care to study the immune, lifestyle and metabolic underpinnings of early CVD4.
The Multi-Ethnic Study in Atherosclerosis (MESA) in USA5, and the Progression of Early Atherosclerosis (PESA) study in Spain6, have paved the way for the characterisation and assessment of CVDs among predominantly European descent (white) populations. Beyond doubt, they have now confirmed that subclinical atherosclerosis progression is a key risk factor of CVD, which means that anyone who has atherosclerotic plaques is worth paying closer attention to, even if they may not yet have clinical symptoms.
In other words, we need to screen healthy people for subclinical atherosclerosis. This has resulted in the development and adoption of a holistic assessment strategy for CVD prevention, which considers regular screening for atherosclerosis such as with coronary artery calcium scoring (CACS), in addition to demographic and medium-term modifiable risk factors in quantitative, multivariate Atherosclerotic Cardiovascular Disease (ASCVD) risk scores7.
“This project brings together our nationwide community of cardiovascular, metabolic, data science and digital health researchers, as well as clinicians across primary and tertiary care to study the immune, lifestyle and metabolic underpinnings of early CVD.”
A much-needed study
However, in Asian populations such as Singapore’s, many patients with CVD have normal cholesterol levels, and many with elevated cholesterol do not develop CVD. The extent of subclinical atherosclerosis in our population is also uncharted. Hence, we need to improve risk assessment, especially for the under-studied 0.6 billion population in Southeast Asia. Moreover, studies here show that a heavy burden of metabolic risk factors contribute towards CVD among Southeast Asian populations, and more so than is in the West8,9,10. Hence, subclinical CVD itself needs clearer study in our region.
Four thematic studies of the heart
First, RESET will compile and study dynamic lifestyle and physiological variables, all of which are not yet included in current risk prediction algorithms. We believe that these represent a promising but unexploited dimension of personalisable modifiable risk factors. Moreover, while lifestyle factors such as diet, physical activity and sleep patterns have all been shown individually to play important roles in CVD development, none have been studied in a deeply characterised cohort, nor have all the lifestyle variables been integratively analysed.
Second, we will establish a selection of molecular markers comprising metabolites, cytokines, RNA and DNA, either free in plasma or packaged within exosomes, and have them systematically characterised for subclinical disease.
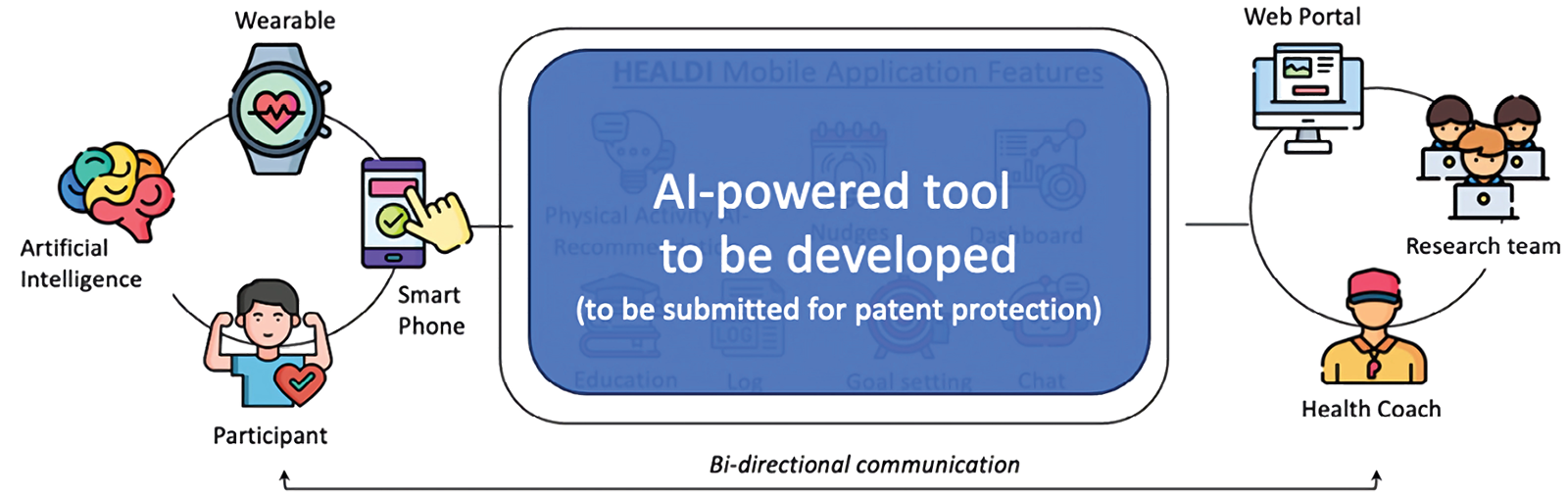
Third, with rapidly advancing tools for big data and AI, we will generate data-driven and AI-powered algorithms for the prediction and prevention of subclinical CVD. We hypothesise that future prediction tools will rely on an individual’s billion-point database, rather than conventional singular predictive assays, enabling personalised management and tracking of disease progression or regression.
Finally, we will assess subclinical markers in the heart muscle itself, such as left ventricular (LV) fibrosis, which may uncover especially relevant early disease trajectories in Asia, where heart failure frequently progresses independently of blocked arteries, and where up to 60% of heart failure patients never had a history of ischemia11,12.
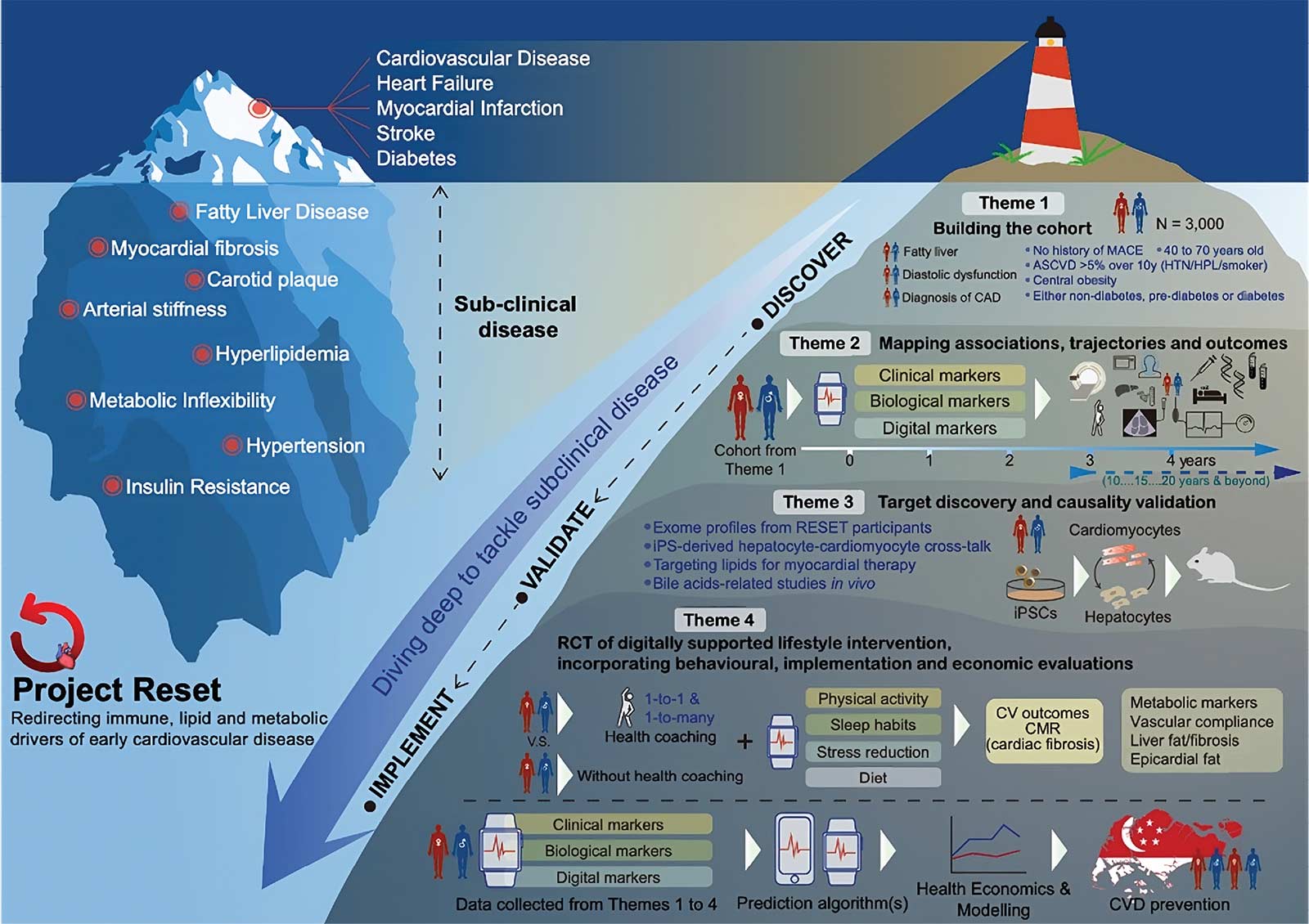
The RESET cohort will be followed longitudinally for five years, and beyond. Annual interval assessments will be carried out for RESET participants, comprising cardiac, liver, and metabolic tests.
Five years to analyse, understand workings of the cardiometabolic system
The RESET cohort will be followed longitudinally for five years, and beyond. Annual interval assessments will be carried out for RESET participants, comprising cardiac, liver, and metabolic tests. Samples will be biobanked for molecular profiling and dynamic lifestyle data collected by a study app and smartwatch, which will be given to each RESET participant for five years.
A sub-group of 200 participants with LV fibrosis on cardiac MRI will be invited to join an intervention study to test the efficacy of a one-year long digitally-enhanced lifestyle intervention, incorporating behavioural, economic and implementation evaluations. The primary outcome of the trial will be LV fibrosis, and secondary outcomes will be vascular, metabolic, and molecular phenotypes.
A sub-group of 200 participants with LV fibrosis on cardiac MRI will be invited to join an intervention study to test the efficacy of a one-year long digitally-enhanced lifestyle intervention, incorporating behavioural, economic and implementation evaluations.
A national study with global implications
The RESET team will also be collaborating with leading international cardiometabolic disease and CVD digital health key opinion leaders. They will form a RESET advisory panel. Finally, reflecting the timeliness of increasing attention on cardiometabolic disease, early disease detection, and global prevention, exciting plans are also underway for parallel RESET cohort studies in the United Kingdom and Southeast Asia.
Partners:
The RESET team will be collaborating with leading international cardiometabolic disease and cardiovascular diseases digital health key opinion leaders.
|
• |
A*STAR’s Bioinformatics Institute |
|
• |
Duke-NUS Medical School |
|
• |
Genome Institute of Singapore |
|
• |
National Heart Centre Singapore |
|
• |
National Heart Research Institute Singapore |
|
• |
National University Health System |
|
• |
National University Heart Centre, Singapore |
|
• |
Nanyang Technological University, Singapore |
|
• |
Ng Teng Fong General Hospital |
|
• |
Singapore Institute for Clinical Sciences |
Amidst huge strides made towards developing precision medicine in Singapore, RESET will push the envelope of precision medicine towards heart disease prevention. Leveraging the most up to date deep learning and AI methods, we are now more than equipped for the deep dive into the vast ocean of data that will be generated in Project RESET.
https://www.myheart.org.sg/.
doi:10.1016/j.eclinm.2023.101850.
doi:10.1161/CIR.0b013e31820a55f5.
doi: 10.1093/eurheartj/ehad543
doi: 10.1093/aje/kwf113.
doi:10.1016/j.ahj.2013.08.024.
doi:10.1161/01.cir.0000437741.48606.98.
doi: 10.1016/j.ajpc.2020.100096.
doi: 10.1016/j.jacc.2022.11.005.
doi: 10.1016/j.jacasi.2021.04.007.
doi:10.1016/j.jchf.2020.12.015.
doi:10.1161/JAHA.119.012199
More from this issue
A WORLD IN A GRAIN OF SAND
Antibodies, The Magic Bullets (Zauberkugel) in Medicine


