Primary Care Research: Now More Than Ever
By Professor Doris Young,
Head, Department of Family Medicine,
National University Health System
Primary Care Research Gap
As I write this, many of Singapore’s General Practitioners/ Family Physicians will be engaging with people seeking primary or first contact medical care. This will be happening in the consultation room, over the phone, on home visits and in many varied locations. People will also be seeking primary care services from nurses, pharmacists, traditional Chinese medicine and other health practitioners.
However, many of the clinical decisions these health practitioners make will be taken on the basis of unsubstantiated evidence. There is concern all around the world, that there is simply not enough research conducted in primary care, to deliver the necessary evidence.
Why is this so, when so much health care takes place in primary care settings? And yet, the majority of research funding supports research into one specific disease, organ system and molecular or biochemical processes – rather than being spent on family /general practice or primary care. Very little is known about important topics such as how primary care services are best organised, how to maximise and prioritise care, how to introduce and disseminate new discoveries so they work in real life, and how patients can best decide how and when to seek care and learn to manage their own care.
Research in primary care in Singapore – Why it’s needed
Most public and population health researchers would argue that research in primary care is essential in order to test and improve clinical practice and question population data. We also have to improve the organisation and delivery of primary care services in order
to provide value and quality of care to the community we serve. Furthermore, we must question the beliefs and behaviour of our patients and engage and empower them to work together to improve the quality of their care and to improve health outcomes. The recent Singapore health policy stipulated the Three Beyonds: beyond hospital to the community, health care to health and quality to value. This vision needs to be delivered by establishing new innovative models of care and alongside the new services, requires rigorous research methodologies to engage primary care providers and users of the care.
Types of research in family practice and primary care
At the outset, it is important to point out that Family Medicine and Primary Care research is different from public/ population health research. We collaborate with Public Health and other clinical specialist colleagues, but we primarily generate research questions aiming to improve care delivery to our patients at the Primary Care interface involving nursing and other allied health professionals. It is often known as implementation and translational research, influences practice and policy using mixed research methods. The gold standard is conducting pragmatic complex intervention clinical trials to improve health outcomes in the primary care setting, linking closely to the community.
Primary care research translates science into the practice of medicine and caring for patients. It provides further understanding of how to better organise healthcare to meet patient and population needs. It develops and evaluates innovations to provide the best healthcare to patients by engaging patients, communities, and practices to improve Health Research Sciences.

Some examples of primary care research trends
As the population ages and chronic diseases and multiple morbidities increase, primary care researchers respond by developing new innovative models of care through empowering and engaging with their patient communities using new digital technologies. As primary care doctors have more patient encounters than any other medical specialists, they have a vital role to play in the screening and assessment of patients for chronic diseases as well as follow up using evidence based guidelines. Therefore, interventions to address the barriers to and facilitators of bowel cancer, cervical and breast screenings are best performed in the primary care settings.
We need to screen and manage the high prevalence of mental health conditions such as depression and anxiety presented to primary care, often as co-morbidities of chronic disease. The pre-frail and frail elderly should also be screened and managed when they present to the family physicians. So the research questions are: What are the best ways to do this? How much funding do we need and what training do doctors need to do this well? How do we engage the doctors and the patients? How do we measure successes and failures?
Some research trends in primary care include the following:
• Type 2 diabetes: prevention, detection and management, Continuous Glucose Monitoring (CGM)
• Trial innovative models of care for people with chronic diseases in the primary care settings
• Ageing and aged care research: screening for falls prevention, detection of dementia
• Mental health: anxiety and depression as singular or co-morbidity
• Modify patterns of care for population groups (chronic disease management, preventative health, mental health, aged care)
• Effectiveness of health services delivery using digitalisation in primary care
• Interest in health outcomes measures (quality of life scales) and burden of diseases
• Amalgamation of large datasets to study populations (AI)
• Health inequalities and disadvantaged populations – need to target high risk group as they present to primary care health professionals
Primary care research translates science into the practice of medicine and caring for patients. It provides further understanding of how to better organise health care to meet patient and population needs. It develops and evaluates innovations to provide the best health care to patients by engaging patients, communities, and practices to improve Health Research Sciences.
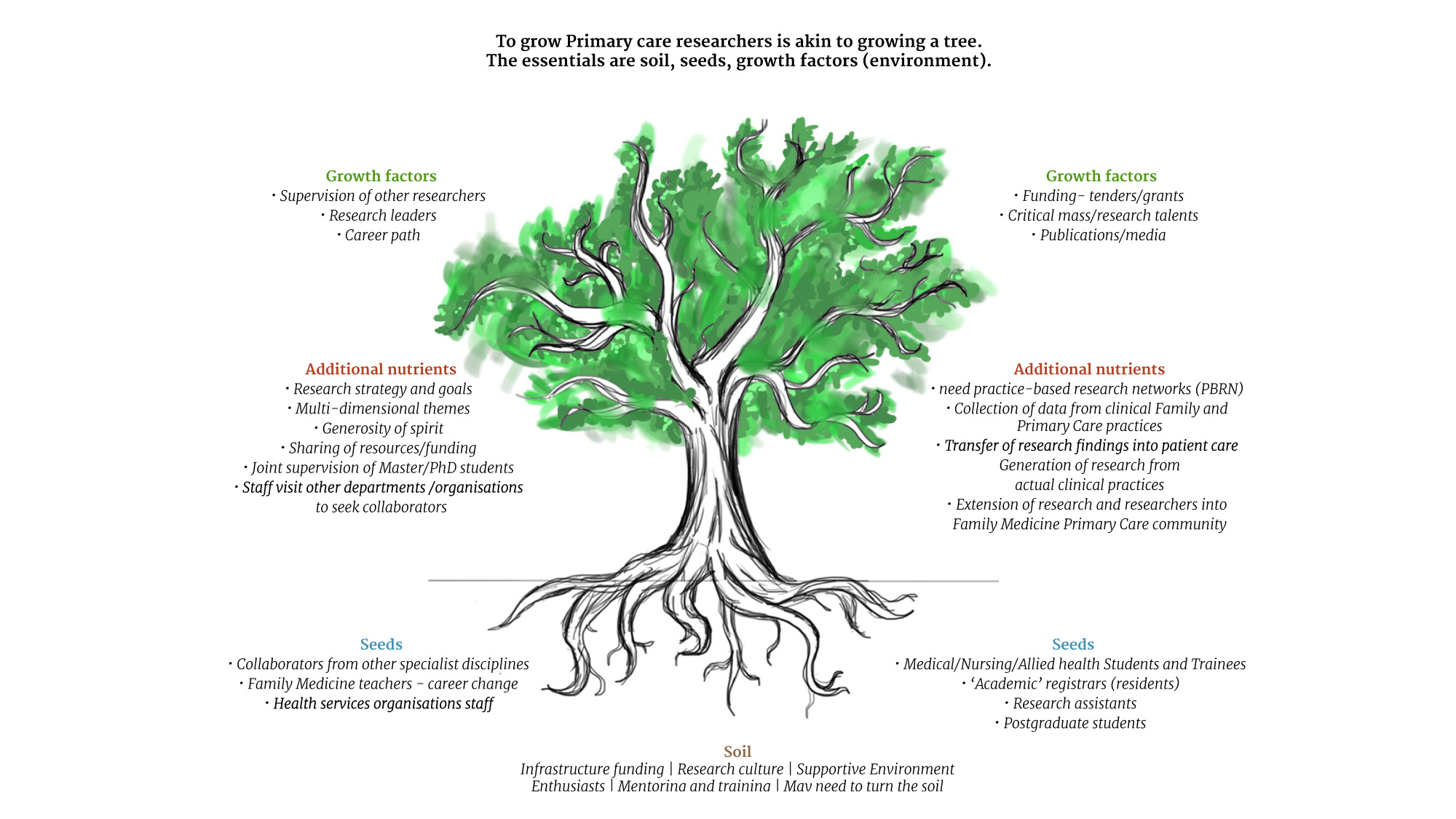
Growing primary care researchers
In order to build primary care research, we need a critical mass. There are not enough well-trained researchers in primary care, because most primary care health professionals such as family doctors and nurses are focused on service delivery.
We need specific funding for primary care-based health services research, such as the UK NHS-funded National Institute for Health Research (NIHR), which has a School for primary care research as well as social care and public health. To date in Singapore and in other parts of the world, most research funding goes to laboratory and hospital-based research and little investment is made in academic Family Medicine and primary care research. It is also evident that academic primary care is strong in countries where substantial levels of research funding are available for general practice/family medicine and primary care research and researchers. However, this amount of funding still lags behind those engaged in biomedical sciences research.
Training for Family Doctors, Nurses, Allied Health professionals to pursue research has to be enhanced. We need to increase the number of clinical staff in primary care with research and development expertise. We need to achieve an evidence-based culture in primary care. In order to do this well, we need to give those conducting research protected time for research and development, through flexible appointments with linked clinical and protected academic sessions. Universities need to develop research training courses and offer higher degrees such as Masters/ PhDs in primary care research with coursework modules that are relevant to general/ family practice. Finally, there must be a clinical academic career pathway for those who wish to combine clinical work and research.
Ways forward for primary care research
• All patients attending primary care services be given opportunity to participate in research
• Primary care research community need to provide more rapid response to new and emerging infectious diseases in the community
• Primary care community need to gain better understanding of the impact of
environment, population and individual risk factors on the health of their patients eg domestic violence, genetic predisposition, health literacy, poverty etc
• Utilisation of new technologies to conduct and disseminate research eg mobile devices, internet-based interventions
• Primary care researchers be more active in engaging in social and political debates to influence policy makers and funding bodies.
Tasks ahead for Department of Family Medicine at NUHS
The primary care strategy that is established includes a framework and support for regional primary care research networks (PCRNs) Table*
Such networks be linked to academic departments of Family Medicine and Primary Care with links to nursing and other primary care clinical professional groups Should include structures for community education, engagement and representation
Such networks should be supported by targeted funding and contractual arrangement allowing dedicated time and resources for active participation of practitioners.
Integrated approach to building sustainable Primary Care leadership and research capacity
