Issue 56
Nov 2025
AFFAIRS OF THE HEART
By Dr Srishti Chhabra, Senior Resident in Infectious Diseases, National University Hospital, Dr Hu Ting Huey, Research Fellow, NUS Yong Loo Lin School of Medicine, Associate Professor Catherine Ong, NUS Yong Loo Lin School of Medicine
new TB cases and
1.25 million
deaths globally in 2023
A global health challenge
Tuberculosis (TB) remains a formidable global health challenge as the leading infectious disease resulting in death. The infection causes potential long-lasting complications even after cure. Declared a global health emergency by the World Health Organization (WHO) in 1993, TB continues to have a worldwide impact—with one in four individuals infected with TB.
In 2023, there were approximately 10.8 million new cases and 1.25 million deaths globally. The rise of drug-resistant strains, specifically multidrug-resistant (MDR) and extensively drug‑resistant (XDR) TB, complicates the situation, limiting treatment options and threatening to escalate this epidemic further. Despite being a high-income country, Singapore is a middle-TB burden setting, a potent indicator of TB’s persistent grip.
Beyond lung damage, the disease may also result in cardiovascular complications. Survivors of TB are at increased risk of conditions such as TB pericarditis and acute coronary syndrome. Furthermore, long-term sequelae in the form of post-TB lung disease may be drivers of pulmonary hypertension, which may result in right heart failure. In literature, up to 47% of pulmonary TB survivors may be afflicted with pulmonary hypertension. The association between TB and cardiovascular disease highlights the need for further research into the long-term health consequences of TB and treatment options to improve patient quality of life.
Clinical studies
Associate Professor Catherine Ong, Assistant Dean (Research) at the Yong Loo Lin School of Medicine, National University of Singapore (NUS Medicine) and Head of the NUHS Clinician-Scientist Academy, has clinical and research interest in mitigating TB immunopathology. Her research team comprises both clinicians and scientists with a specific focus on translational medicine that bridges laboratory insights with clinical application and utilises cellular and animal TB models in multinational clinical trials.
47%
of pulmonary TB survivors may be afflicted with pulmonary hypertension
At the forefront of pioneering research into complex immune interactions between Mycobacterium tuberculosis and host factors driving immunopathology, the lab has conducted cross-sectional studies to explore immune dysregulation in patients with poorly-controlled diabetes who contract pulmonary TB—an area of critical importance given the global prevalence of both conditions. We found an upregulation of matrix metalloproteinases (MMPs), which drive inflammation in patients with pulmonary TB, and hyper-inflammatory immune dysregulation in pulmonary TB patients with poorly controlled diabetes, such as defective phagocytosis and hyper-responsive neutrophil inflammation.
This work is driven by PhD student Dr Thong Pei Min, now a Research Fellow at the National Centre for Infectious Diseases, and funded by the National Medical Research Council. Dr Thong won the Best Poster prize at the leading international Infectious Disease Congress—European Society of Clinical Microbiology and Infectious Diseases (ESCMID)—and was also awarded the National Centre for Infectious Disease Short Term Fellowship. This research sheds light on how metabolic disorders might alter immune responses, potentially guiding new treatment strategies. Patients with pulmonary TB who had poorly controlled diabetes also expressed higher angiogenic factors. Further investigation into this is being driven by Research Associate Mr Wong Yi Hao who has successfully developed a diabetic murine model of pulmonary TB and is currently working towards his PhD.
On the therapeutic front, our lab has conducted a randomised-controlled Phase 2 clinical trial, which has demonstrated the efficacy of host-directed therapies, such as doxycycline (an MMP inhibitor), in reducing the inflammatory transcriptome and immune-phenotype seen in pulmonary TB, with corresponding reduction of lung cavity volume. Through this study, we investigated host transcriptomics using bulk RNA sequencing and utilised bioinformatics to identify mechanistic immune signatures seen in TB.

UMS BSL-2+ where TB samples will be processed for the Phase 3 Randomised Controlled Trial at Sabah sites, Malaysia.

Singaporean and Malaysian researchers.

The team at the NUHS Scientific & Innovation Summit 2024.
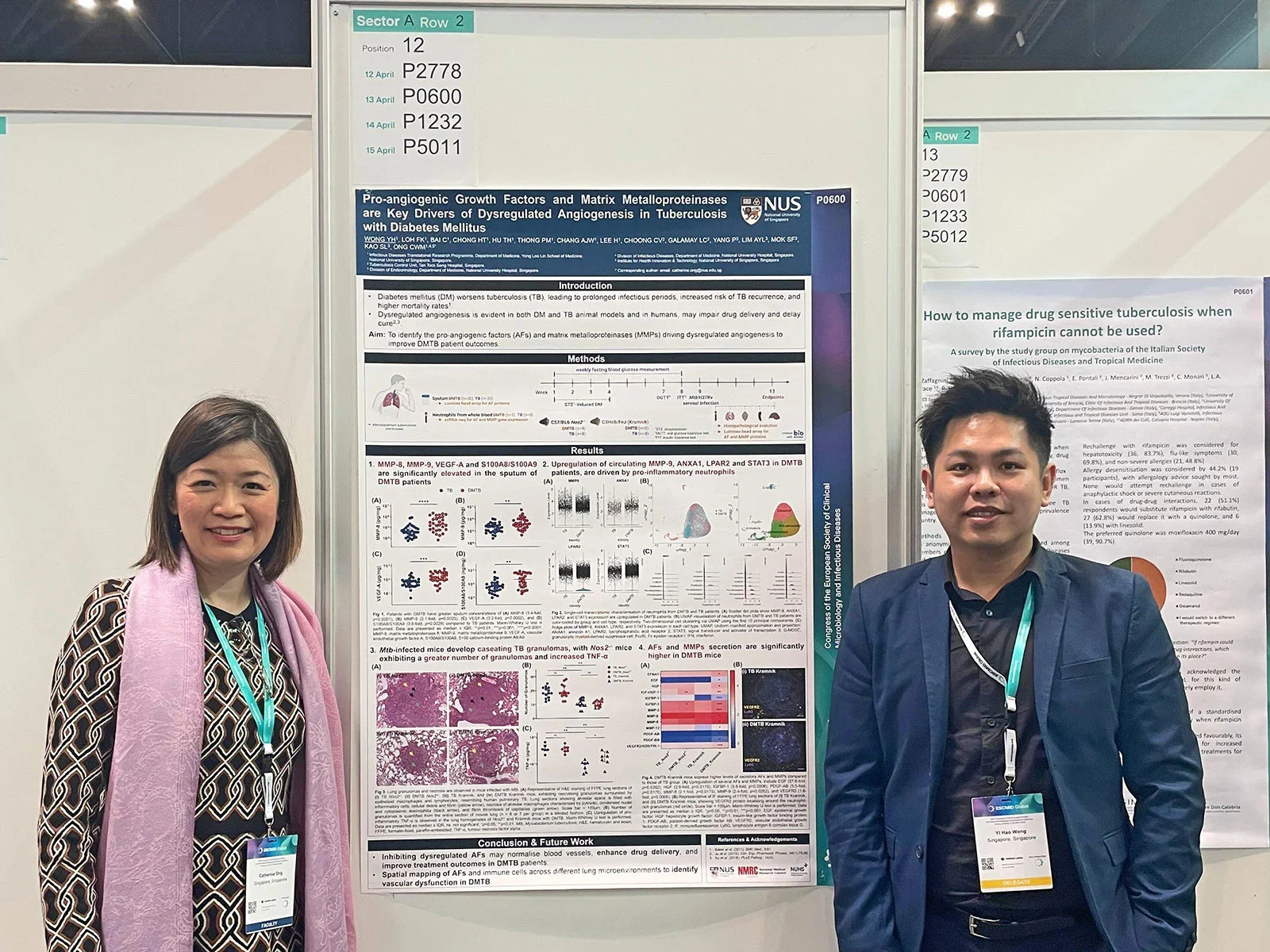
A/Prof Catherine Ong and Mr Wong Yi Hao, Research Associate, presented their poster at the European Society of Clinical Microbiology and Infectious Diseases (ESCMID) 2025 in Vienna, Austria.
Our team is validating the findings of the Phase 2 trial with an ongoing international multicentre Phase 3 randomised controlled trial, which assesses the long-term effects of adjunctive doxycycline on pulmonary and cardiovascular outcomes in patients with cavitary pulmonary TB. This is being conducted at four trial sites in Singapore and Sabah, Malaysia. This eight-year study with experimental medicine component, funded by NMRC CS-IRG and CSA (Senior Investigator), is driven by PhD student Dr Angelica Win, Research Fellow Dr Hu Ting Huey and Infectious Diseases Senior Resident Dr Srishti Chhabra. They will be performing cardiac blood tests (Troponin I, NT Pro‑BNP), echocardiograms and electrocardiograms to assess the effect of adjunctive doxycycline on the development or resolution of pulmonary hypertension. They will also assess doxycycline’s effect on the rates of acute coronary syndrome. This cutting-edge translational work advances both the understanding and treatment of TB at the intersection of infectious disease and host pathology, with important global health implications.
Funding and collaboration
The extensive translational work is made possible by collaboration with multidisciplinary experts in Singapore and the South East Asia region. We have close partnerships with local experts such as Cardiovascular-Metabolic Disease Translational Research Programme (CVMD-TRP), NUH Investigational Medical Unit (IMU) and National Tuberculosis Care Centre (NTBCC). Our team also collaborates with global partners, including University of Sydney (Australia), University of Southampton (UK), Clinical Research Centre (CRC) Sabah, University Malaysia Sabah (UMS) and Queen Elizabeth Hospital Sabah, Malaysia. The National Medical Research Council (NMRC), National University of Singapore (NUS) and National University Hospital Singapore (NUHS) have continuously funded our work.
We have consistently been selected to present our work at multiple national and international conferences, including the annual European Respiratory Society Conference and the ESCMID. Our lab members have won the NUS Medicine Chan Heng Leong Award, Department of Medicine Junior Research Award for three consecutive years (2022-2024), and international awards such as APCCMI Best Oral presentation and a Wellcome Trust Bursary.
Our lab is committed to employing host-directed strategies and novel therapeutics in our fight against TB, aligning with the WHO’s goal to end the TB epidemic by 2035. By focusing on the intersection of host-pathogen interactions and leveraging cutting-edge transcriptomics and bioinformatics, we aim to uncover innovative treatment approaches that address TB’s complex pathology and its association with other health conditions such as diabetes and cardiovascular disease.
More from this issue