
Issue 56
Nov 2025
AFFAIRS OF THE HEART
By Dr Leonard Yeo, Adjunct Associate Professor, NUS Yong Loo Lin School of Medicine

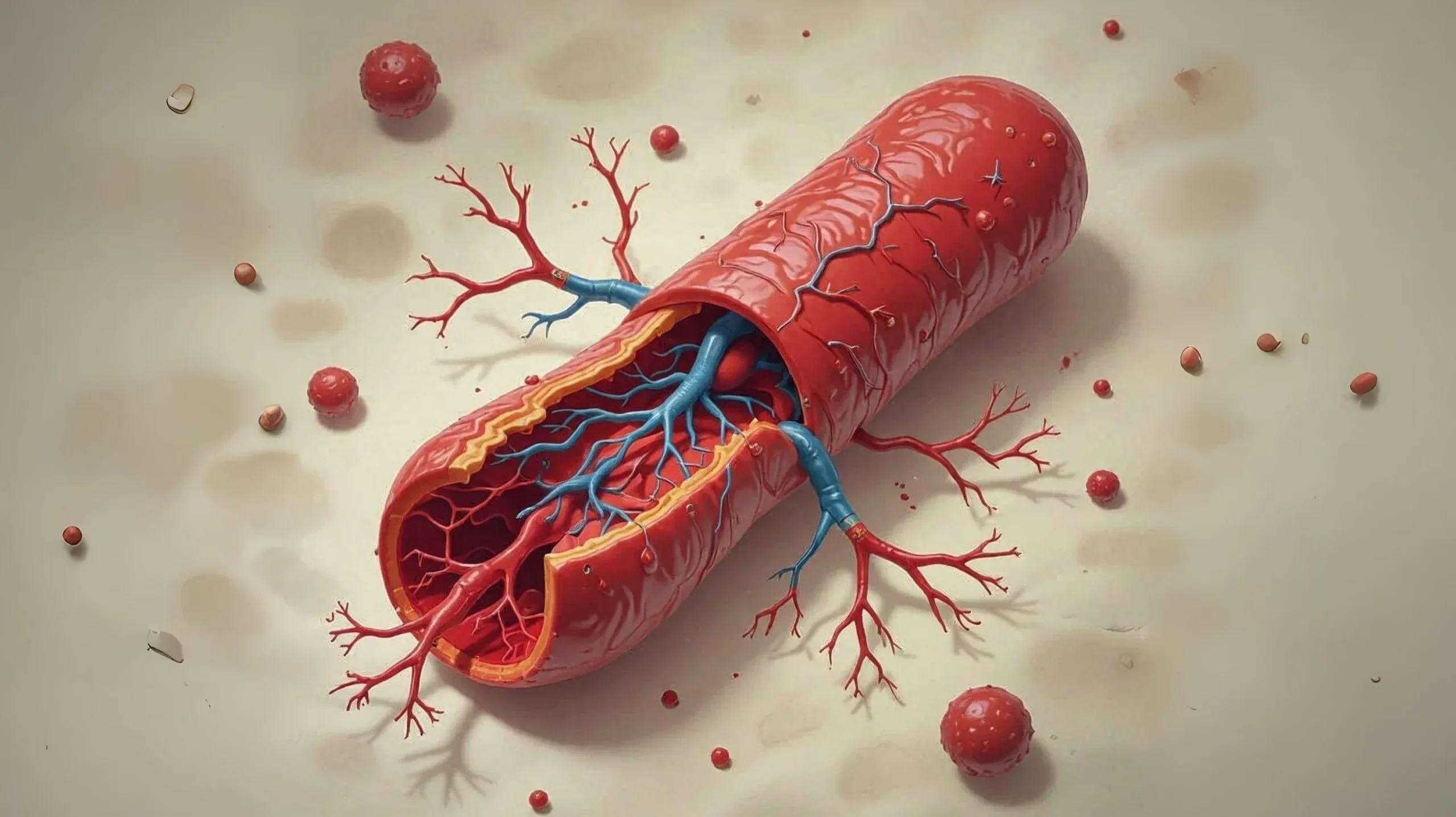
Imagine a narrow pipe clogged with debris, with water unable to flow through. Now, picture that same scenario inside one of the arteries in your brain. This is what happens with intracranial atherosclerotic stenosis (ICAS)—a dangerous narrowing of the brain’s blood vessels that can lead to strokes.
Strokes caused by ICAS are a major global health problem, especially among Asian, Black, and Hispanic populations. Doctors currently focus on the degree that an artery has narrowed to decide on treatment, but this approach isn’t perfect—some people with mild narrowing still have strokes, while others with severe blockages remain fine.
New research suggests that the key to better stroke prevention may lie not just in how narrow the artery is, but in how blood flows through it. This article explores why ICAS is so dangerous, why current treatments fall short, and how studying blood flow patterns could revolutionise stroke care.
Intracranial stenosis: A hidden stroke threat
A global problem with uneven impact
ICAS doesn’t affect everyone equally. While it causes about 10% of strokes in the US, that number jumps to nearly 50% in some Asian countries. This suggests that genetics, diet, or other factors play a big role.
How ICAS causes strokes
There are three main ways a narrowed brain artery can lead to a stroke:
|
• |
Not enough blood flow – If the artery is too narrow, parts of the brain may not get enough oxygen, leading to a stroke. |
|
• |
Clots breaking off – A rough or unstable piece of plaque inside the artery can send small clots downstream, blocking smaller vessels. |
|
• |
Small adjacent blood vessels – Small blood vessels called perforators originate within larger blood vessels: plaques can grow over and cover the openings of these small blood vessels, blocking them. |
Currently, doctors mostly rely on how much the artery has narrowed to assess risk. But studies show that even a moderate narrowing (50-70%) can be dangerous if blood flow is disrupted—meaning we’re missing something important.
Why current treatments aren’t enough
Similar to cardiology practice, placing a stent (a tiny mesh tube) to prop open the artery might seem like a good solution, but studies have found that stenting actually caused more strokes than medications alone in the short term. There have been three major randomised clinical trials on ICAS treatment where they compared stenting with medical therapy and found that aggressive medical therapy—blood thinners, cholesterol drugs, and blood pressure control—worked better than stenting for preventing strokes. Because of this, stents are now only used in salvage cases where medications fail. Guidelines stipulate that patients need to have had a stroke, been given medication and had another stroke before they can undergo stenting. However, by then, many patients already have permanent disability. Despite this, our treatment solutions are woefully inadequate as even with the best medications, about 8-12% of patients have another stroke within a year.

Placing a stent (a tiny mesh tube) to prop open the artery might seem like a good solution, but studies have found that stenting actually caused more strokes than medications alone in the short term. Because of this, stents are now only used in salvage cases where medications fail.
The big problem: Measuring narrowing of arteries doesn’t tell the whole story
Imagine two people with a 70% blocked artery:
|
• |
Person A has good supplementary blood flow from other vessels (collaterals) and has never had a stroke. |
|
• |
Person B has no supplementary or unstable blood flow and suffers a stroke. |
Current imaging (like CT or MRI scans) shows how narrow the artery is, but not how well blood is moving through it. That’s why some people with “mild” blockages have strokes, while others with “severe” narrowing don’t. In cardiology the measurement of blood flow includes the supplementary blood flow and is called the fractional flow reserve (FFR). It is measured by a pressure sensing wire and requires the vessel to be at its maximum dilation to be accurate. In the brain, it is difficult to measure FFR, given the danger of inserting wires into the brain over the narrowing and giving medications to dilate the vessels.
The future: Blood flow as a key to better treatment
What are flow dynamics?
Think of blood flow like water in a river. If the river narrows, the water speeds up, gets turbulent, or even flows backward in some spots. Similarly, when an artery narrows:
|
• |
High-speed jets of blood can damage the vessel wall. |
|
• |
Turbulence can lead to clot formation. |
|
• |
Low flow areas may starve parts of the brain of oxygen. |
New technology lets doctors measure these changes, which could help predict stroke risk better than just looking at narrowing.
New tools to study ICAS
|
• |
Computational Fluid Dynamics (CFD) – Uses computer simulations based on MRI/CT scans to model blood flow and find dangerous patterns. |
|
• |
Specialised MRI scans – Can detect inflamed or unstable plaques that are more likely to cause clots. Furthermore, in patients with ICAS, there can be many plaques in the same vessel: these scans help to determine which is the problematic plaque and its characteristics, to ensure correct and personalised tailored treatment. |
|
• |
Blood based biomarkers – Different types of strokes (i.e. clots breaking off versus not enough blood flow) may give rise to different expressions of biomarkers that can be picked up in a blood test. |
The Vertebrobasilar Flow Evaluation and Risk of Transient Ischemic Attack and Stroke (VERiTAS) study found that measuring blood flow haemodynamics predicted stroke risk better than just looking at how narrow the artery was.1 Other research shows that abnormal blood flow patterns (like low wall shear stress) are linked to higher stroke risk. Finally, some companies have biomarker blood profiles which can determine if a person is at risk of developing or suffering from atherosclerosis, and if there are unstable plaques in the heart and neck vessels.
What this means for patients
In the future, doctors might:
|
• |
Use blood flow tests to find high-risk blockages before a stroke happens and identify patients who can be stented rather than wait for patients to have a stroke before treatment. |
|
• |
Personalised treatment—for example, recommending stents only if blood flow is severely disrupted while increasing the strength of antiplatelet treatment or anticoagulation medication if clots breaking off is the underlying cause of stroke. |
|
• |
Monitor therapy success by checking if medications improve blood flow. Improved perfusion to the brain can also result in functional improvements—better and sharper thinking and possibly a reduced risk of vascular dementia. |
Conclusion: A smarter way to prevent strokes
Intracranial stenosis is a complex problem, and current treatments don’t work well enough for everyone. The missing pieces are due to a lack of understanding of the mechanisms and fluid dynamics of ICAS, and not just the degree of artery narrowing.
By combining advanced imaging, plaque characteristics and biomarkers with computer modelling, doctors can soon predict strokes more accurately and tailor treatments to each patient’s unique risk. This mindset shift—from asking “How narrow is it?”—could save countless lives by preventing strokes before they strike in this Asian-predominant disease that is widespread in Singapore.
Amin-Hanjani S, Pandey DK, Rose-Finnell L, Du X, Richardson D, Thulborn KR, Elkind MS, Zipfel GJ, Liebeskind DS, Silver FL, Kasner SE, Aletich VA, Caplan LR, Derdeyn CP, Gorelick PB, Charbel FT; Vertebrobasilar Flow Evaluation and Risk of Transient Ischemic Attack and Stroke Study Group. Effect of Hemodynamics on Stroke Risk in Symptomatic Atherosclerotic Vertebrobasilar Occlusive Disease. JAMA Neurol. 2016 Feb;73(2):178-85. doi: 10.1001/jamaneurol.2015.3772. PMID: 26720181; PMCID: PMC5274634.
More from this issue



