Issue 55
Sep 2025
AFFAIRS OF THE HEART
By Associate Professor Marie Ng, PhD, NUS Yong Loo Lin School of Medicine
Cardiovascular disease (CVD) is the leading cause of mortality and morbidity among member states of the Association of Southeast Asian Nations (ASEAN). In 2021, there were an estimated 36.8 million prevalent cases of CVD in the region, resulting in 1.66 million deaths. In Singapore, the number of prevalent cases has increased by nearly 200% over the past 30 years, reaching an estimated 386,000 cases in 2021. These are the findings based on the Global Burden of Disease 2021 study, published in The Lancet Public Health ASEAN special issue in June.
In a first-of-its-kind collaboration, the Yong Loo Lin School of Medicine, National University of Singapore (NUS Medicine) joined forces with the Institute for Health Metrics and Evaluation (IHME) at the University of Washington, along with partners across the region, to launch a special ASEAN paper series in The Lancet Public Health. This paper series explores both existing and emerging epidemiological challenges in the region—including CVD1, smoking2, injuries3, and mental disorders4.
This paper series is part of the Global Burden of Disease (GBD) study—one of the largest and most comprehensive epidemiological research collaborations in the world. The GBD provides a powerful framework for understanding the causes of suboptimal health, equipping policymakers, clinicians, researchers, and the general public with the evidence needed to advocate for meaningful change.
First launched in the 1990s and featured in the World Development Report 1993, the GBD was designed to answer four fundamental questions: How many people are dying? What are they dying from? What causes illness? And what are the factors leading to death and disease? The original iteration of the GBD focused on 107 diseases, providing aggregated estimates for eight regions. Over the past three decades, it has expanded to cover more than 459 health outcomes and risk factors across 204 countries and territories from 1990 to the present. The GBD offers an unparalleled view of global health trends, helping to inform and shape effective public health strategies and interventions.
The guiding principles of the GBD are to produce comprehensive, comparable, and transparent estimates of health loss across diseases, injuries, and risk factors for all populations over time. Many people may not realise the extent of heterogeneity and bias present in healthcare data. Electronic medical records capture only diagnosed cases, often missing undetected or untreated conditions. Claims data reflect only individuals with insurance coverage, excluding those without. While health surveys can offer valuable population-level insights, they are prone to self-reporting bias and are typically not conducted annually—resulting in temporal gaps in the data.
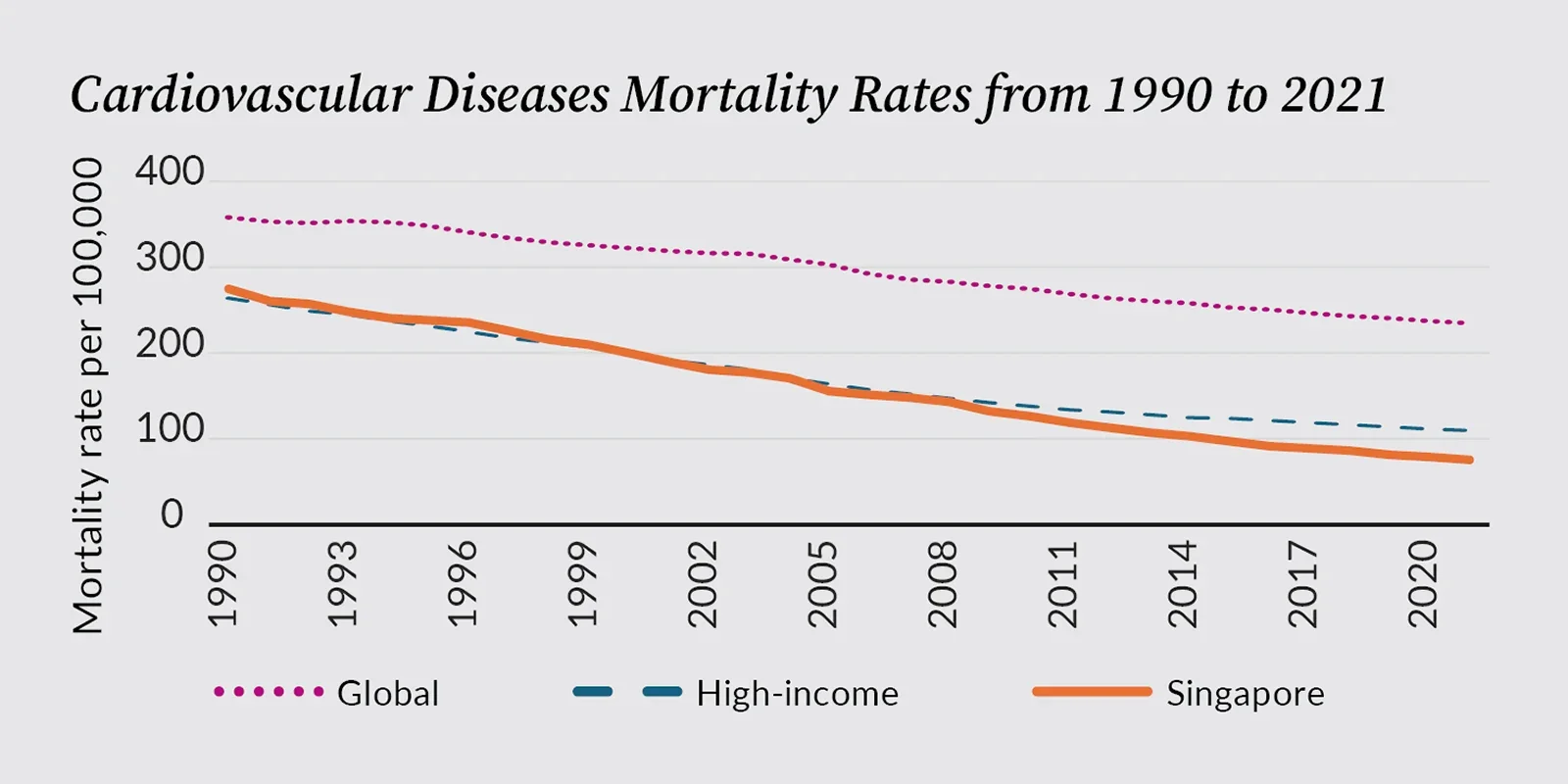
The GBD is a monumental analytical effort that synthesises data from all available sources using highly standardised methodologies to ensure consistency, harmonise definitions, and apply advanced modelling techniques to interpolate and generate robust estimates. These continuous and consistent estimates enable both geographical and temporal comparisons. For example, we can confidently compare Singapore’s CVD mortality with that of other high-income Asia Pacific countries, knowing that the metrics are derived from standardised definitions and methods.
In 2021, Singapore’s age-standardised CVD mortality rate was estimated at 75 per 100,000—slightly higher than Japan’s rate of 72 per 100,000, but lower than South Korea’s 85.9 per 100,000, the high-income country average of 110 per 100,000, and the global average of 235 per 100,000. Consistent metrics such as these allow countries to benchmark progress, identify emerging disease trends, and project future healthcare resource needs with greater precision.
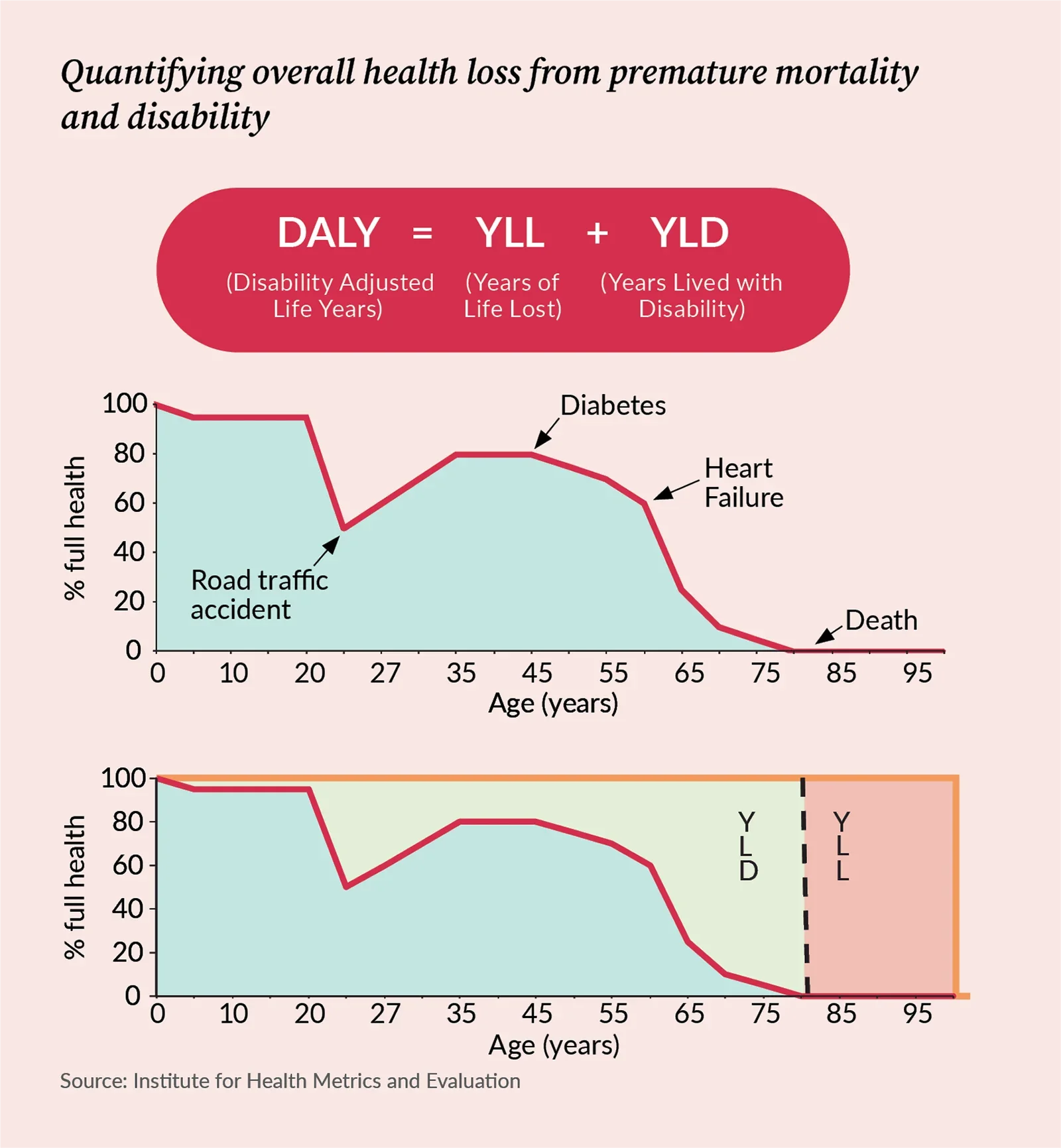
Another valuable feature of the GBD is its assessment of disease burden not only from deaths but also from disability. The study’s signature metric—the disability-adjusted life year (DALY)—combines years of life lost (YLL) due to premature death and years lived with disability (YLD). YLL measures the number of years lost due to death before a presumed optimal life expectancy, while YLD reflects the years lived in suboptimal health.
With advances in medicine and improvements in socio-environmental conditions, the prevalence, incidence, and mortality of many fatal diseases have gradually declined.
However, individuals are now living longer with chronic, non-fatal conditions. Many of these conditions impose a substantial burden of disability, undermining individual well-being, and have profound health, social, and economic consequences. Returning to CVD: while the all-age YLL rate has declined by 37% since 1990, the all-age YLD rate has increased by 22%. The former reflects the remarkable success of Singapore’s advanced healthcare system and clinical technologies in reducing mortality from CVD. In contrast, the latter signals a growing burden of morbidity. In other words, although individuals are living longer, they are not necessarily living healthier lives. With an ageing population, the burden of disability is likely to continue increasing in the years ahead.
In addition to tracking diseases, the GBD quantifies the impact of key risk factors—metabolic, environmental, and behavioural—that contribute to illness and death. Using an established epidemiological approach known as comparative risk assessment, GBD estimates the proportion of disease burden attributable to specific risk factors. In Singapore, high blood pressure was the leading CVD risk factor in 2021, accounting for 39% of the total CVD burden. Dietary risks, such as high sodium intake, low fruit consumption, and low dietary fiber intake, were responsible for 29%. High fasting plasma glucose and tobacco use each contributed 13% of the CVD burden.
A particularly concerning risk factor is high body mass index (BMI). Over the past 30 years, the CVD burden attributable to high BMI has increased by 120% in the country. A different GBD study published earlier this year forecasted that more than 60% of Singaporean adults will experience overweight or obesity by 2050.5 Alarmingly, the rate of increase in childhood obesity in Singapore is the fastest among all high-income countries.6 Childhood obesity is associated with early onset of diabetes, CVD, and other non-communicable diseases. To reduce future disease burden, there is an urgent need to invest in risk factor prevention in the younger generation.
As healthcare in Singapore moves beyond traditional hospital-centric care towards a population health paradigm, understanding population health metrics is becoming increasingly important for clinicians. The ability to compare and interpret key epidemiological statistics, and to distil data into actionable insights, matters not only at the macro policy level but also in clinical practice, where patient care can be meaningfully contextualised within broader disease trends.
In November 2024, NUS Medicine and IHME signed a Memorandum of Understanding to strengthen collaboration and advance the understanding and application of population health metrics. Through this partnership, NUS Medicine hopes to inspire more researchers and clinicians across NUS and National University Health System to engage in GBD–related work and contribute to the growing field of population health research.
Goh LH, Chong B, Lubbe SCC van der, et al. The epidemiology and burden of cardiovascular diseases in countries of the Association of Southeast Asian Nations (ASEAN), 1990–2021: findings from the Global Burden of Disease Study 2021. The Lancet Public Health 2025; 10: e467–79.
Dai X, Ng M, Gil GF, et al. The epidemiology and burden of smoking in countries of the Association of Southeast Asian Nations (ASEAN), 1990–2021: findings from the Global Burden of Disease Study 2021. The Lancet Public Health 2025; 10: e442–55.
Lubbe SCC van der, Chong LS, Hay SI, et al. The epidemiology and burden of injury in countries of the Association of Southeast Asian Nations (ASEAN), 1990–2021: findings from the Global Burden of Disease Study 2021. The Lancet Public Health 2025; 10: e456–66.
Szücs A, Lubbe SCC van der, Torre JA de la, et al. The epidemiology and burden of ten mental disorders in countries of the Association of Southeast Asian Nations (ASEAN), 1990–2021: findings from the Global Burden of Disease Study 2021. The Lancet Public Health 2025; 10: e480–91.
Ng M, Gakidou E, Lo J, et al. Global, regional, and national prevalence of adult overweight and obesity, 1990–2021, with forecasts to 2050: a forecasting study for the Global Burden of Disease Study 2021. The Lancet 2025; 405: 813–38.
Kerr JA, Patton GC, Cini KI, et al. Global, regional, and national prevalence of child and adolescent overweight and obesity, 1990–2021, with forecasts to 2050: a forecasting study for the Global Burden of Disease Study 2021. The Lancet 2025; 405: 785–812.
More from this issue