
Issue 54
Jul 2025
IN VIVO
A year ago, four young Chinese medical students arrived at Yong Loo Lin School of Medicine, National University of Singapore (NUS Medicine) on an exchange programme. Li Hongpeng, Yang Yufan, Zhang Youran and Zhou Yuechen say the experience thus far has been transformative—educationally and personally.
Come August, the quartet from Tsinghua Medicine will have reached the halfway mark of their two-year exchange programme at NUS Medicine. They are the second batch of medical exchange students, following the inaugural group from Université Paris Cité (UPC) in August 2023.
Why did you choose to do your exchange at NUS Medicine?
Youran: I am on the physician-scientist track at Tsinghua Medicine. As part of this track, I must complete three years of foundational studies at Tsinghua Medicine before moving on to clinical training or research. It so happens that Yuechen, Yufan, and I all chose to conduct our research at the University of Pittsburgh, US, for 2.5 years. That was where we were before coming to NUS Medicine.
When the opportunity arose to complete our clinical training at one of three institutions—Peking Union Medical College, one of the region’s top medical centres, Beijing Tsinghua Changgung Hospital, a newly affiliated hospital of Tsinghua Medicine, or NUS—we unanimously chose NUS. We wanted to explore and experience medical education in another country.
Yufan: Like Youran, I wanted to broaden my perspective on medical education and experience first-hand what a healthcare system in an international setting is like. Noting that Singapore is a multicultural country with a sizable medical tourism economy, I was confident it would offer the experience I sought. Additionally, I saw it as a great opportunity to develop cultural sensitivity and strengthen my communication skills—both essential qualities for a future doctor.

Yuechen (fourth from left) having lunch with her CG mates at Ghim Moh Road Food Centre.

Yufan (first from right) having dinner with clinical group mates to celebrate the completion of their Family Medicine posting.
Hongpeng: I chose NUS Medicine for a few reasons. NUS is globally renowned for its medical programmes, particularly in areas like tropical medicine, public health, and healthcare innovation. I wanted to experience its rigorous curriculum and gain exposure to Singapore’s advanced healthcare system, which integrates cutting-edge technology with efficient medical practices. I also value the chance to connect and work alongside accomplished professionals and researchers, opening doors to future collaborations or international medical practice—all of which align closely with my interest in health policy and medical technology.
Singapore’s multicultural environment provides a unique lens on healthcare delivery in a diverse society. Engaging with peers and patients from varied backgrounds and experiencing Singapore’s healthcare system first-hand enhances my ability to work in global health settings, strengthens my theoretical knowledge, and inspires ideas for potential reforms when I return to China for clinical practice.

Hongpeng (middle) celebrating the Lantern Festival with his nightly running and badminton mates.
Yuechen: I share the same sentiments as Youran, Hongpeng and Yufan. On a personal level, I particularly appreciate the opportunity to interact with patients from various ethnic and cultural backgrounds. This experience has helped me understand how cultural factors influence healthcare decision-making, allowing me to develop a more holistic and culturally sensitive approach to patient care.
Beyond the academic and clinical aspects, I was also drawn to Singapore as a vibrant multicultural country. I am deeply impressed by the country’s commitment to inclusivity, which is reflected not only in its healthcare system but also in many aspects of daily life.
How does studying Medicine at NUS compare to studying at Tsinghua University?
Hongpeng: The rigour and emphasis on interprofessional education are similar at both NUS Medicine and Tsinghua Medicine. Both universities are equipped with state-of-the-art medical facilities—simulation labs, research labs, and libraries—and students at both universities have access to extensive digital resources, including research journals, medical databases, and online platforms for remote learning.
However, the two institutions differ in their curriculum structure, teaching approach, and language of instruction. NUS offers an integrated curriculum with early clinical exposure, emphasising case-based learning and patient-centred care, along with strong partnerships with teaching hospitals. In contrast, Tsinghua Medicine incorporates both Western medicine and Traditional Chinese Medicine (TCM), reflecting China’s rich medical heritage, while also placing a strong emphasis on research, technological innovation, and a collaborative approach.
Yufan: Top off, the intensity and workload of the curriculum are comparable. In both instances, a high level of dedication, self-discipline, and perseverance is necessary to excel. However, due to the nature of my academic track, I do not have sufficient insights into medical science education at NUS Medicine or clinical education at Tsinghua Medicine to make a meaningful comparison.

Hongpeng (back row, right) with his clinical group mates during the Internal Medicine posting.
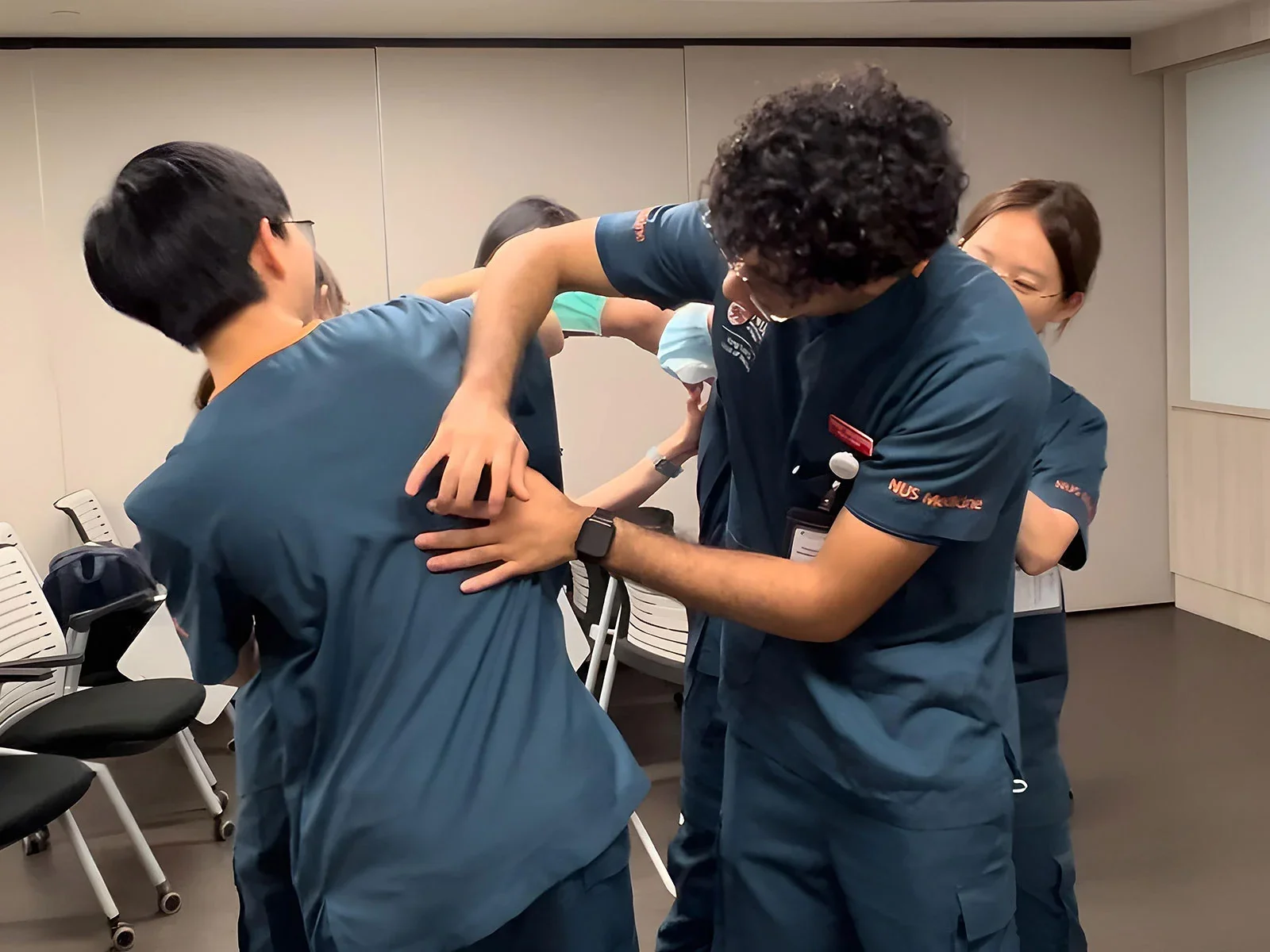
Yufan practising percussion with her clinical group mates.
Yuechen: Like Yufan, I spent all my preclinical years at Tsinghua Medicine and, so far, have done all my clinical studies at NUS. During my preclinical years at Tsinghua Medicine, we attended many lectures conducted by biomedical scientists, exposing us to cutting-edge research in immunology, microbiology, neurology, etc. From what I understand from my NUS Medicine clinical group mates, their early years at NUS Medicine focused more on clinical applications.
Based on what my Tsinghua Medicine batchmates have shared, the structure of the clinical years also differs significantly. At Tsinghua Medicine, students begin with several months of didactic teaching covering all specialties before starting hospital postings. Here, at NUS, lectures form a relatively small component of the postings, requiring students to take a more proactive role in learning through patient interactions.
My conclusion is that both schools emphasise integrating medical students into patient care as an essential part of clinical training. The hands-on learning ensures that students are not just passive observers but important members of the healthcare team.
Youran: Tsinghua Medicine offers two programmes: the physician-scientist programme, which Yufan, Yuechen, and I are enrolled in, and the clinician-scholar programme, which is similar to the bachelor’s programmes at NUS Medicine. The physician-scientist programme places a much stronger emphasis on research. These differences in curriculum structure meant that we had to hit the ground running when we first arrived at NUS Medicine. We had to familiarise ourselves with all of the clinical skills foundation content, such as measuring vitals, drawing blood, taking patient history, and conducting physical examinations—because NUS students had already learnt these skills in their second year.
NUS Medicine’s strong culture of encouraging students to take a more proactive role in their learning is also evident in the way classes are conducted. Unlike the didactic teaching I am more accustomed to, lectures and tutorials here are heavily discussion-based, often requiring students to analyse case scenarios and propose solutions. This approach pushes us beyond simply acquiring knowledge—it trains us to apply it effectively in real world settings, just as competent doctors are expected to do.
Another interesting difference between NUS Medicine and Tsinghua Medicine—and even the University of Pittsburgh—is that NUS Medicine students are not limited to clinical rotations in a single hospital network. Instead, they train across multiple healthcare clusters, including SingHealth, the National Healthcare Group, and the National University Health System. This exposure allows them to experience diverse healthcare delivery models and interact with healthcare professionals from various backgrounds. Additionally, it provides opportunities to collaborate with medical students from other institutions, such as Duke-NUS.

Youran (front row, second from left) out for an evening run with his friends.

Yuechen (back row, right) wrapping up IM posting at NUH.
How has your experiences so far changed your views about Medicine or healthcare?
Yuechen: We learnt about motivational interviewing and effective communications with persons with disabilities in class. Subsequently, during my Family Medicine posting, I had the opportunity to witness how the doctors applied these techniques to convince an elderly gentleman with intestinal obstruction to proceed with stenting. This experience made me realise the importance of structured communication frameworks in building rapport, addressing patient concerns, and guiding them towards informed decision-making. Beyond diagnosing and treating diseases, a physician’s ability to engage, educate, and empower patients significantly influences clinical outcomes.
Another time, I met a frail elderly lady suffering from systemic sclerosis-associated lung disease. I had researched on this topic before coming to Singapore, but nothing beats the experience of seeing first-hand how the disease profoundly affected her daily life, mobility, and breathing. No amount of reading or research could replicate this experience. It was a powerful reminder of why I chose Medicine—to bring meaningful improvements in patients’ lives through day-to-day clinical practice and translational research.
Yufan: I agree with Yuechen. Like her, I’ve come to appreciate the importance of effective communication. Whether it is building rapport with my clinical group mates, establishing trust with patients we see or connecting with professionals we work with at the hospitals, strong communication is essential for my learning and excelling in my work—both as a researcher and a doctor.
Youran: This programme was my first real exposure to clinical practice, and the experience was both novel and fascinating. Seeing the knowledge we worked so hard to memorise for exams come to life in real patient cases reminded me to take learning seriously—because in clinical settings, our knowledge directly impacts diagnosis, treatment decisions, and most importantly, patient outcomes.
One particular case stands out to me. I examined a young boy who complained of ear pain and partial hearing loss. Hearing his symptoms, I immediately suspected a neurological condition—only to be gently reminded by the supervising doctor to check his ears first. Sure enough, he had a significant build-up of earwax, which was the actual cause of his discomfort. That experience taught me that not all symptoms stem from disease—sometimes, the simplest explanations are the correct ones.
Going through this programme has also deepened my respect for how cultural and geographical differences influence medical practice. For example, in Singapore’s tropical climate, dengue fever is always a key consideration when evaluating potential diagnoses. During Ramadan, Muslim patients who fast for a month may require adjustments to their insulin dosage, while individuals on a vegan diet need tailored nutritional plans to ensure adequate intake of essential nutrients. In addition, the opportunity to interact with a diverse patient demographic—including Chinese, Malay, Indian, and international patients—has enhanced my ability to navigate cultural nuances in healthcare, strengthening my competence in a more globalised medical setting.

Yufan (second from left) attending a talk by Dr Wann Jia Loh on Lipoprotein(a).
Hongpeng: During my Family Medicine posting, I observed a diverse group of patients, many of whom faced significant socio-economic challenges. It was eye-opening to see how social determinants—such as income, education, and access to healthcare—played such a significant role in their health outcomes. One particular case involved a patient with a chronic condition who struggled to adhere to treatment due to financial constraints and lack of family support. This experience reinforced the fact that healthcare is not just about diagnosing and treating diseases—it’s also about understanding the broader context of a patient’s life and working to remove barriers to care. As doctors, we need not only medical knowledge but also compassion, social awareness, and the ability to advocate for patients beyond the clinical setting. It strengthened my commitment to pursue a holistic approach to medicine.
On another occasion, I met a cancer patient undergoing treatment for colon cancer. She had been battling the disease for several months. Despite her challenges, she refused to let the illness define her and instead embraced each day with gratitude and hope. Her positive outlook on life, despite the difficult circumstances, was both inspiring and humbling. It is a reminder of the importance of mental and emotional resilience in the face of illness and how a patient’s mindset can have such a powerful impact on their healing journey.
How does this exchange experience at NUS Medicine contribute to your growth and your future medical career?
Hongpeng: My exchange experience at NUS Medicine has been incredibly transformative, both personally and professionally. It has broadened my perspective on healthcare by exposing me to diverse patient populations and teaching me how to approach medicine with cultural sensitivity, empathy, and a holistic view. Interacting with patients from various backgrounds and learning about the challenges they face has made me realise the importance of considering social determinants of health, not just medical conditions.
Academically, NUS Medicine’s rigorous curriculum and hands-on clinical experiences have strengthened my clinical skills and deepened my understanding of medical theory. The emphasis on patient-centred care, case-based learning, and teamwork has made me a more adaptable and reflective learner, and I feel better prepared to handle the complexities of modern medicine.
On a personal level, this exchange has helped me develop resilience and a deeper sense of empathy, which I believe are crucial qualities for any healthcare professional. I’ve also learnt the importance of maintaining work-life balance and taking care of my own well-being in such a demanding field. As I move forward in my medical career, the lessons and insights I gained at NUS will guide my approach to patient care, reminding me that Medicine is as much about human connection as it is about clinical expertise.

Hongpeng (left) with his clinical group mates during campus based learning week of General Surgery posting.
Yuechen: When I first arrived at NUS Medicine, I struggled with both Singlish and my limited clinical knowledge. A year on, I am happy to say that I have overcome these challenges with the support of my clinical group mates, tutors, and even patients. This experience underscored the importance of teamwork—and how improving a patient’s health is never the effort of just one person.
The opportunity to interact with a diverse patient population has also strengthened my ability to adapt my communication style to different individuals. I believe this skill will be invaluable regardless of the healthcare setting or country I work in. Every patient deserves to feel heard, understood, and respected.
Youran: To quickly add to Yuechen’s point about teamwork—NUS Medicine truly reinforces the importance of multidisciplinary care by requiring medical students to observe nurses and learn Nursing techniques, such as stoma care and wound dressing, from them. It was a valuable experience to see first-hand how a patient’s healthcare journey is shaped not just by doctors, but also by nurses and other healthcare professionals.
Like Yuechen, I also find myself adopting a Singaporean tone and using a lot of Singlish when taking patients’ histories. As a healthcare professional, I see it as my responsibility to make patients feel comfortable and ensure they understand what I’m asking—not the other way around. Judging by their responses, I would say this approach has been quite effective.
On a separate note, entering my clinical training phase here has deepened my commitment to research—because there are millions of unaddressed questions and doctors are too busy taking care of patients in the clinical settings to think about them. But these are not simple questions—they require individuals with both medical and scientific training to bridge the gap between patient needs and clinical challenges. I’m excited to contribute to this cause.
More from this issue



