Issue 50
May 2024
SCIENCE OF LIFE

Less is more—that is what researchers have found while conducting a tri-nation clinical trial to see if shorter courses of antibiotics are as effective as longer prescriptions of the drug to treat ventilator-associated pneumonia (VAP).
460
patients in
39
ICUs in Nepal, Thailand and Singapore were involved in the REGARD-VAP study
Patients with VAP have a
40%
risk of death
Led by Dr Mo Yin from the Infectious Diseases Translational Research Programme at the Yong Loo Lin School of Medicine, National University of Singapore (NUS Medicine) and Consultant from the Division of Infectious Diseases in the Department of Medicine at National University Hospital (NUH), the 4-year long REducinG Antibiotic tReatment Duration for Ventilator-Associated Pneumonia (REGARD-VAP) study involved 460 patients in 39 hospital intensive care units (ICUs) in Nepal, Thailand and Singapore.
VAP is a common lung infection among critically ill patients in hospital ICUs, who are dependent on ventilators to breathe. It occurs when bacteria invade the lower respiratory tract and thin lung tissues via the breathing tube. The infection leads to longer hospital stays, increased antibiotic use, and the risk of death is as much as 40%. While personalised short-course treatment duration for patients with VAP was just as effective in reducing the duration of pneumonia in comparison to the standard treatment duration, the short-course treatment strategy also successfully reduced antibiotic side effects from 38% to 8%.
460 patients with VAP were randomly assigned into two groups—a 3-to-5-day individualised, short-course antibiotic treatment plan, and a longer standard-of-care treatment plan of at least 8 days. The main aim was to determine if the individualised short-course strategy is non-inferior to the usual standard-of-care duration, in terms of the increased risk of death or the recurrence of pneumonia within 60 days of enrolling into the study. Of the 460 participants, 41% in the individualised short-course group and 44% in the standard-of-care group either died or had pneumonia recurrence.
Participants were reviewed daily to assess if they met the criteria to stop antibiotics. The criteria included a core body temperature of less than or equal to 38.3 degree Celsius for 48 hours and a stable blood pressure. When the criteria were met, all participants in the short-course treatment strategy group were weaned off antibiotics after 3 to 5 days of receiving VAP treatment. For patients in the standard care duration group, the antibiotic treatment strategy lasted at least 8 days, as determined by their primary physicians. Current standard-of-care antibiotic treatment can last up to 2 to 3 weeks, accompanied by higher risks of side effects and unnecessary economic costs.
The study’s findings serve as a point of reference for antibiotic usage reduction and titration, so that the onset of antibiotic resistance can be prevented.
Antibiotics are the default treatment used for patients with VAP, which is the commonest hospital-acquired infection in the ICUs. However, antibiotics when used indiscriminately in large amounts will make antibiotics less effective overtime and increase bacteria’s resistance to antibiotics. This clinical study shows that the duration and the strategy of antibiotic treatment can be tailored based on how the patient responds to treatment and is feasible to be adopted even in settings with limited resources, coupled with constant evaluation by attending physicians.”

Dr Mo Yin (second from left) discussing a patient’s case with local doctors in Sri Lanka during a site visit in January 2024.
“Antibiotics are the default treatment used for patients with VAP, which is the commonest hospital-acquired infection in the ICUs. However, antibiotics when used indiscriminately in large amounts will make antibiotics less effective overtime and increase bacteria’s resistance to antibiotics. This clinical study shows that the duration and the strategy of antibiotic treatment can be tailored based on how the patient responds to treatment and is feasible to be adopted even in settings with limited resources, coupled with constant evaluation by attending physicians,” said Dr Mo Yin, Infectious Diseases Translational Research Programme at NUS Medicine.
The REGARD-VAP clinical trial was jointly funded by the Singapore National Medical Research Council and the United Kingdom Medical Research Council. The paper titled ‘Reducing antibiotic treatment duration for ventilator-associated pneumonia (REGARD-VAP): a trial protocol for a randomised clinical trial’ was published in the Lancet Respiratory Medicine on 23 January 2024.
Click here to read the full paper.
More from this issue

SCIENCE OF LIFE
What women want to see in pregnancy health apps
SCIENCE OF LIFE
Healthcare Ethics? Think like an engineer

SCIENCE OF LIFE
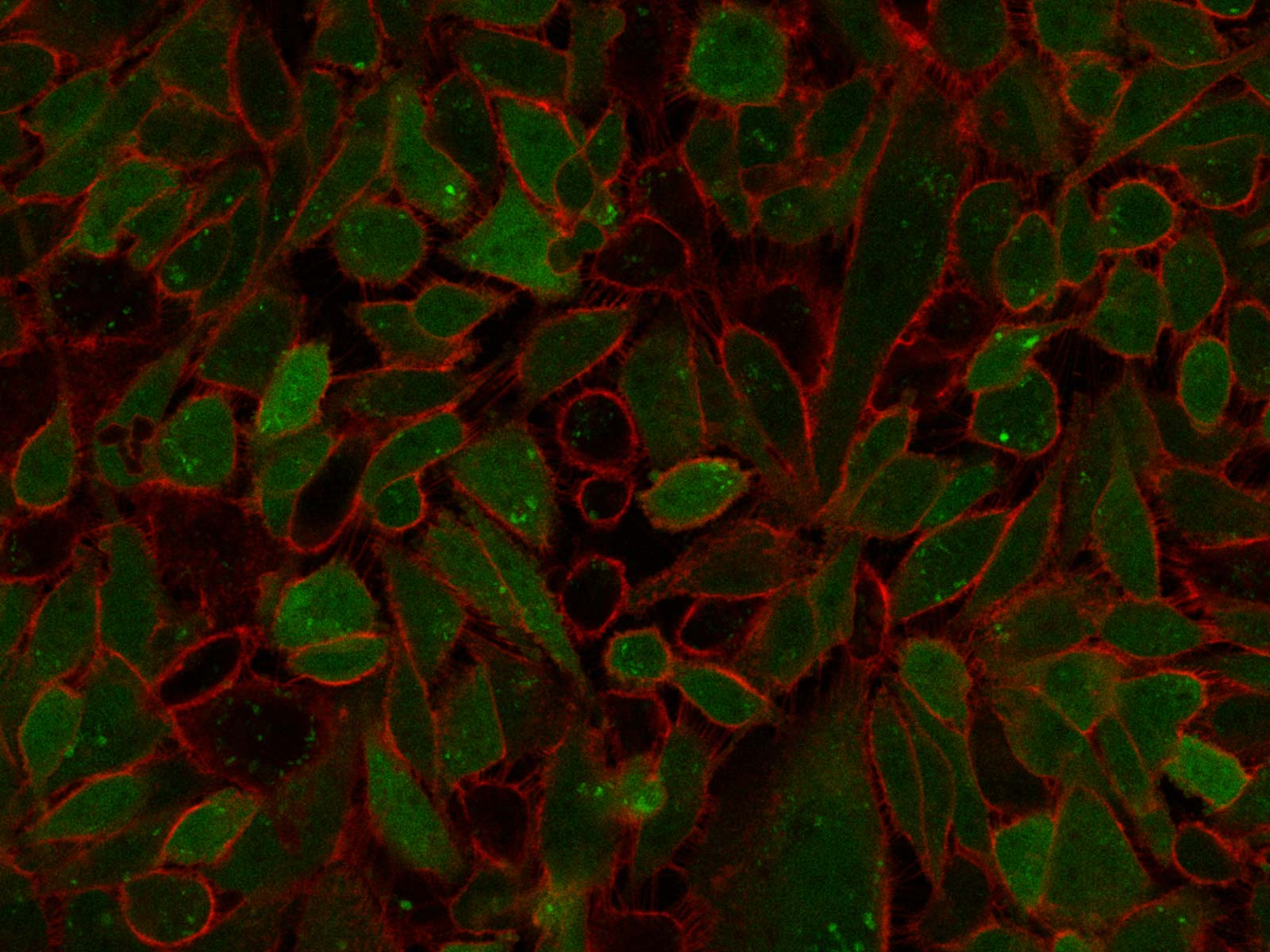
Self-sacrificing Cancer Cells