
Issue 49
Feb 2024
INSIGHTS
By Distinguished Professor Ashok Venkitaraman, Director, Cancer Science Institute of Singapore, National University of Singapore & Research Director, Institute for Molecular and Cell Biology, A*STAR
Roughly one in every three of us is expected to suffer from cancer at some point in our lives. Cancer incidence is increasing worldwide, and this disease is a leading cause of death amongst Singaporeans.
But cancer is not a singular disease. It can arise in almost any organ in our bodies, and at each site, with distinctive characteristics. For example, breast cancer is different from liver cancer or stomach cancer, and so on. For these reasons, cancer is best considered as a group of diseases rather than a singular entity.
When cells go rogue
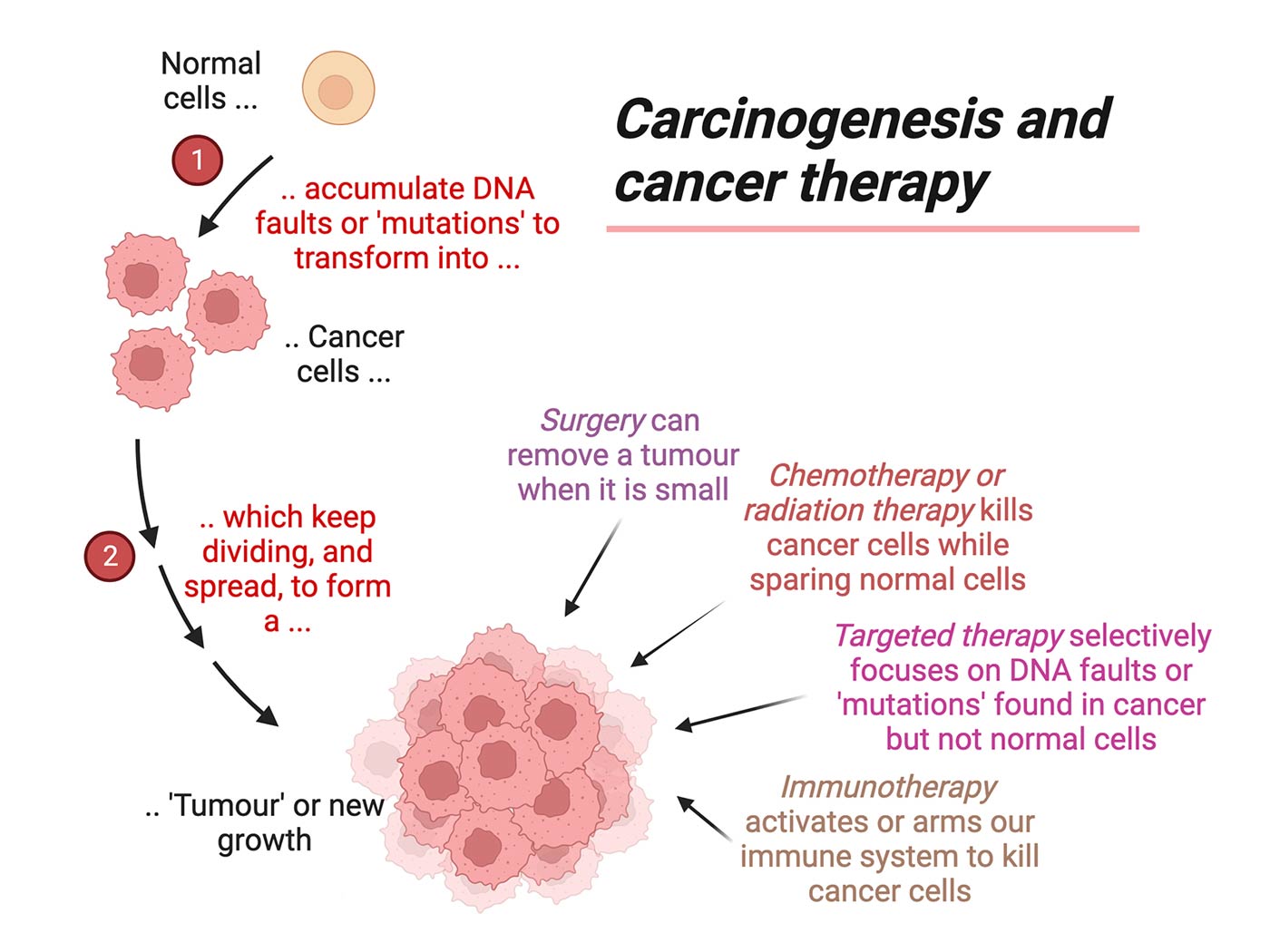
Nevertheless, cancers arising anywhere have certain shared features, which come from the events that lead to cancer formation. We call this process “carcinogenesis”. During carcinogenesis, normal cells that make up different organs are transformed into cancer cells. So, for example, how is a normal liver cell different from a cancerous liver cell?
By and large, normal cells are well behaved, and play by inbuilt rules that keep us healthy. For instance, normal cells have a defined lifespan. Normal cells will not keep dividing to create daughter cells unless instructed to do so when necessary. Normal cells tend to stay in place, and do not invade other parts of the body.
Cancer cells break these inbuilt rules, and go rogue. They overcome limits on normal lifespan, and often continue to divide into daughter cells, forming a tumour (which is a term to describe swelling or new growth). Cancer cells invade other parts of the body, often distant from where the tumour was first formed.
What makes cancer cells break the inbuilt rules that keep us healthy? These inbuilt rules are encoded in our genes (which are made from a molecule called DNA, present in each of our cells). During carcinogenesis, normal cells accumulate more and more faults in their genes. The growing number of faults cause the rules that govern normal cells to break down, transforming them into cancer cells. This process can be likened to the accumulation of faults over time in the memory of a computer, which eventually causes the computer to fail, because the instructions for its operation stored in the memory have been damaged. DNA in a similar way serves as a memory which carries instructions for normal cell behaviour encoded as genes—when faults accumulate in genes, normal cell behaviour breaks down, and normal cells can be transformed into cancer cells.
Simply understanding how cancers are formed, and how cancer cells are different from normal cells, helps to explain why cancer is so hard to treat.
1 IN 3
individuals is expected to suffer from cancer at some point in their lives
Total eradication of rogue cells is essential
To cure cancer, we must completely remove or eliminate all—100%—of the rogue cancer cells. Getting rid of even 99% may not be enough, because cancer cells will often continue to divide into daughter cells, and the cancer could come back.
Sometimes—when cancer is detected in its earliest stages and is still small—surgery can remove the entire tumour. However, if even a small number of cancer cells is left behind, the cancer can come back. That is why surgeons must be very careful to completely remove the cancer, and why after surgery, patients are often monitored for several years to check if the cancer starts to come back.
Unfortunately, many cancers are too advanced at the time of diagnosis to be completely removed by surgery alone, and other treatments are required. Any effective treatment for cancer has to specifically target cancer cells, but leave normal cells unharmed. Cancer treatments attempt to achieve this goal by targeting features of cancer cells that are not shared with normal cells.
Carcinogenesis and cancer therapy. Created with BioRender.com
For example, cancer cells often divide whereas normal cells do not. Many treatments for cancer—like chemotherapy or radiation—tend to kill cells that are dividing rapidly. So, cancer cells are more sensitive to these treatments than normal cells. However, the margin of sensitivity is not very high, and so treatments like chemotherapy or radiation also have side-effects on normal cells and cannot be given in very high doses. For this reason, it is often impossible to completely kill 100% of cancer cells using chemotherapy or radiation, making cancer difficult to treat.
To make matters worse, cancer cells often develop resistance to drugs or radiation. Such resistant cancer cells cannot be killed by these treatments, again making cancer difficult to treat.
Sometimes—when cancer is detected in its earliest stages and is still small—surgery can remove the entire tumour. However, if even a small number of cancer cells is left behind, the cancer can come back. That is why surgeons must be very careful to completely remove the cancer, and why after surgery, patients are often monitored for several years to check if the cancer starts to come back.”
In addition, cancer cells unlike normal cells spread throughout the body. A cancer patient at the time of diagnosis may have cancers in many different parts of the body, and not just in one place. Such spreading makes it almost impossible to completely remove advanced cancers using surgery alone, and also makes cancer difficult to treat using drugs or radiation after it has spread widely.
Advances in treatment
What is being done to solve these problems and make cancer treatment more effective? There have been many important advances in recent years that offer increasing hope for cancer patients. Most cancers are now being treated using a combination of drugs, or drugs plus radiation. ‘Combination therapy’ has two main advantages. Combinations that kill cancer cells in different ways are often more effective than a single therapy. Moreover, drug resistance becomes less problematic, because the chance that cancer cells develop resistance to different kinds of therapy at the same time is low.
New modes of treatment that are more efficient at killing cancer cells and with fewer side effects, are being developed. It is now possible to ‘read’ the DNA in cancers, and pinpoint the faulty genes that cause the cancer. Very specific treatments—termed ‘targeted therapy’—can be developed to selectively kill cancer cells carrying these faulty genes, while sparing normal cells. So, targeted therapy is more effective and has fewer side effects.

Cancer cells can evade our immune system by assuming a stealth mode in which they become invisible to the immune system, and thereby evade elimination. New therapies—called ‘immunotherapy’—which reactivate the immune system against cancer have been developed. Some immunotherapies involve drugs that make cancer cells visible to the immune system. Other immunotherapies arm our own immune cells to identify and kill cancer. These armed cells—called CAR-T or TCR-T cells—can be injected back into cancer patients to treat cancer. While immunotherapies are proving effective, they remain very expensive and often do not work for reasons that are not yet well understood.
Further research on cancer remains vital to overcome these problems. Over half of the world’s population is of Asian descent, but most cancer research has been carried out on samples or models that reflect European descent. We have begun to appreciate that cancers in Asia can differ from cancers in other populations, and that different treatments may be required. This is one important reason for continuing cancer research in Singapore, to ensure that patients here can benefit from the latest advances.
More from this issue

ETHICALLY SPEAKING
Small Country, Large Research Trials – What Singapore Can Learn from Denmark


