Issue 41 / February 2022
SCIENCE OF LIFE
Singapore Research Team Uses Indoor Air Sampling Surveillance to Sniff Out COVID-19
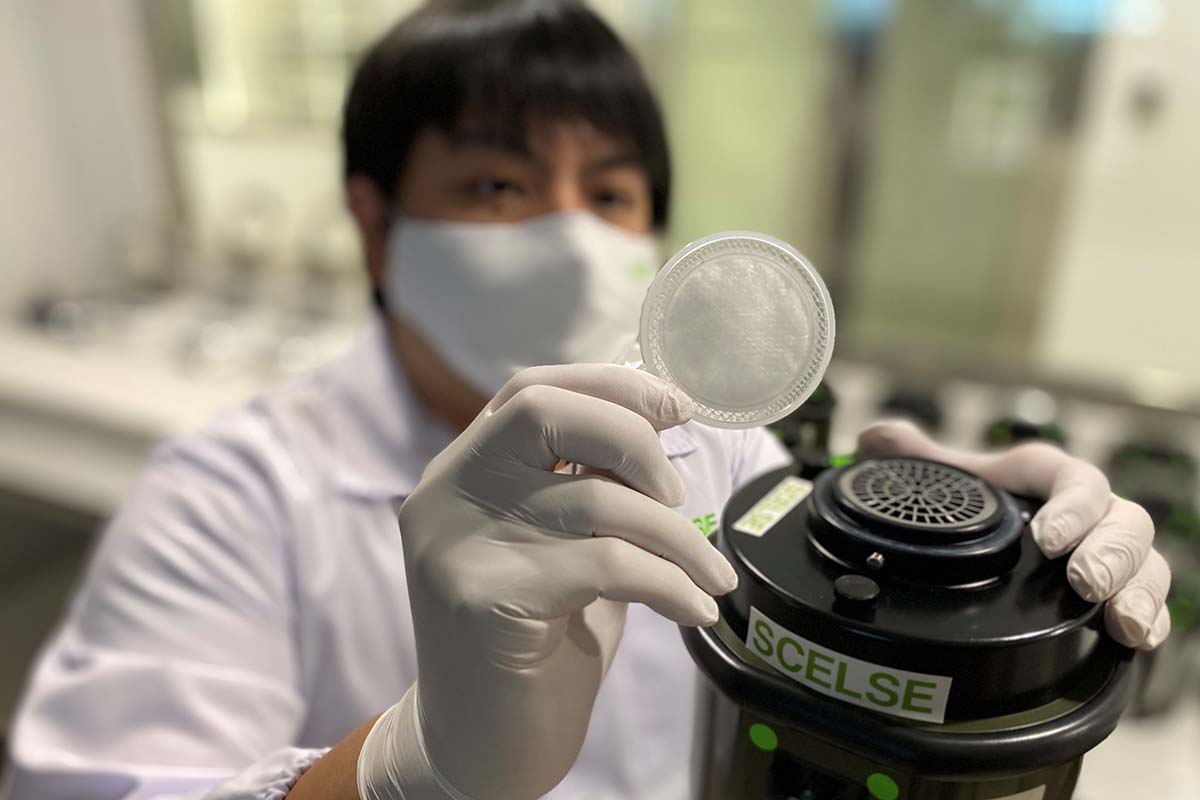
A team of scientists and doctors from the Singapore Centre for Environmental Life Sciences Engineering (SCELSE) at Nanyang Technological University, Singapore (NTU Singapore) and NUS Medicine has developed a capability to detect airborne SARS-CoV-2 RNA—the nucleic acid coding for the virus that causes COVID-19—indoors through air sampling.
hen trialled in two inpatient wards of a major Singaporean hospital caring for active COVID-19 patients, the air surveillance approach produced a higher detection rate of environmental SARS-CoV-2 RNA, compared to surface swab samples collected in the same area.
The COVID-19 Delta variant’s rapid spread in Singapore and globally underlines the need for rapid identification of the presence of SARS-CoV-2 in the environment. While wastewater testing is a reliable indicator of the presence of virus in sewage discharge, the retrospective nature of this approach means pre-emptive action is not possible.
The findings, described in a study published in Indoor Air on 14 September, indicate the potential for an airborne surveillance system that monitors for the presence of the virus and provides early warning of infection risks, especially valuable in hospitals and nursing homes, and enclosed places where large numbers of people congregate, said the research team.
Professor Paul Tambyah, Deputy Director of NUS Medicine’s Infectious Diseases Translational Research Programme and President of Asia Pacific Society of Clinical Microbiology and Infection, highlighted, “The results of this air sampling study are encouraging, with the potential for the simple monitoring for the presence of COVID-19 in possible hotspots. This will allow for timely intervention where necessary to prevent the emergence of clusters. Hopefully this will prove useful as the country gradually transitions into recognising the disease as endemic and everyone learns to live as normally as possible with the virus.”
Dr Irvan Luhung, SCELSE senior research fellow and study co-lead author, pointed out, “This study demonstrated the versatility and sensitivity of air sampling for monitoring SARS-CoV-2 in hospital settings, something that was previously not thought possible due to the high ventilation rate of hospital wards. Such an air surveillance capability could make a valuable contribution towards keeping frontline medical staff safe in this pandemic. In hospitals with a high daily number of COVID-19 patients, employing a routine air surveillance programme with high sensitivity could be beneficial in detecting the virus early and help keep frontline medical staff safe.”
Associate Professor David Allen from NUS Medicine’s Infectious Diseases Translational Research Programme and an infectious diseases clinician at the National University Health System (NUHS), said, “The paper’s findings expand our knowledge of the extent to which the virus may potentially be transmitted in different types of wards—this impacts safety and needed precautions for healthcare workers. The findings also advance the potential use of different methods for detecting virus in the environment, providing additional tools for mass screening (other methods are screening each person, sampling sewage, etc)—in our case a device which samples the air for the presence of virus.”
The findings indicate the potential for an airborne surveillance system that monitors for the presence of the virus and provides early warning of infection risks, especially valuable in hospitals and nursing homes, and enclosed places where large numbers of people congregate.
Professor Stephan Schuster, Deputy Centre Director at SCELSE, and genomics professor at the School of Biological Sciences, NTU, and Associate Professor David Allen, led the joint study.
How the study was conducted
In ventilated indoor settings with a large air change rate—an industry standard measurement that indicates how often the air in a room is replaced by outdoor air—it can be difficult to detect a viral agent in the air. For instance, the air change rate in an hospital isolation ward can be up to 14 times per hour.
To overcome this challenge, the scientists deployed air sampling devices in combination with an ultra-low biomass analysis approach developed by the team from SCELSE at NTU. The analysis approach consists of a series of steps tailored for successful RNA extraction from air samples.
The extracted RNA is subjected to real-time quantitative reverse transcription polymerase chain (RT-qPCR), which has the same sensitivity as the standard nasopharyngeal swab test which tests for the presence of SARS-CoV-2 in the sample.
Two types of hospital wards were tested between February and May 2020: a naturally ventilated, open-cohort ward and a mechanically ventilated isolation ward. Air sample collectors with varying flow rates were deployed for eight-hour periods in different areas in the ward, such as the PPE donning area in the open-cohort ward, the windowsill in the isolation ward, and the toilets of both wards. A total of 27 air samples were collected.
Alongside the air samples, 73 surface swab samples from the patient care, staff, and toilet areas of the two ward types were collected and analysed for comparison. The chosen swab sites were not cleaned for at least eight hours prior to swabbing.
The scientists found that their devices operating at the higher air sampling flowrate of 150L/min (compared to the lower flowrate of 50L/min) improved the chances of successful airborne SARS-CoV-2 surveillance.
Among the samples collected by the high flowrate sample collectors, 72% were found to contain the SARS-CoV-2 virus. This is in comparison to the surface swab samples, which showed a positive detection rate of 9.6%. These results highlight the potential of air sampling as a tool to detect the presence of SARS-CoV-2 in the environment, said the scientists.
Future air surveillance studies will need to be tested in locations outside of hospital environments—where mass gatherings occur—for rapid and sensitive high throughput communal testing at the population level, said the research team.
The study was funded by a National Medical Research Council grant to NTU, and an alumni gift to NUS by Freepoint Commodities Pte Ltd.
‘Airborne SARS-CoV-2 surveillance in hospital environment using high-flowrate air samplers and its comparison to surface sampling’ published in Indoor Air, 14 September 2021. https://doi.org/10.1111/ina.12930.