Issue 38 / May 2021
Science of Life
Stem Cells Lead the Way to Saving Sight
Age-related macular degeneration (AMD) is a debilitating disease that results in blurring or loss of the sharp central vision, which we use to see fine details. AMD affects approximately 196 million people worldwide, a number that is projected to increase to 288 million in 20401.
he macula is a small area in the middle of the retina. In AMD, a single layer of cells under the macula called the retinal pigment epithelium (RPE) is damaged, resulting in blurriness and even central vision loss. In the initial stages, straight lines may also look wavy.
The RPE has many roles, including acting as the blood-retina barrier, controlling fluid transport, and recycling parts of worn-out photoreceptors (special cells in the retina that convert light into an electrical signal for the brain). To carry out their recycling function, the cells of the RPE must be able to phagocytose (engulf) and recycle photoreceptor outer-segments.
196 million
people are affected
by AMD globally today
288 million
people are projected
to be affected by
AMD worldwide by 2040
Over the years, researchers have tried different methods to replace the essential RPE layer. These include autologous RPE patches via macular translocation. A promising new approach involves transplanting stem cell-derived RPE cells to the damaged area under the macula.
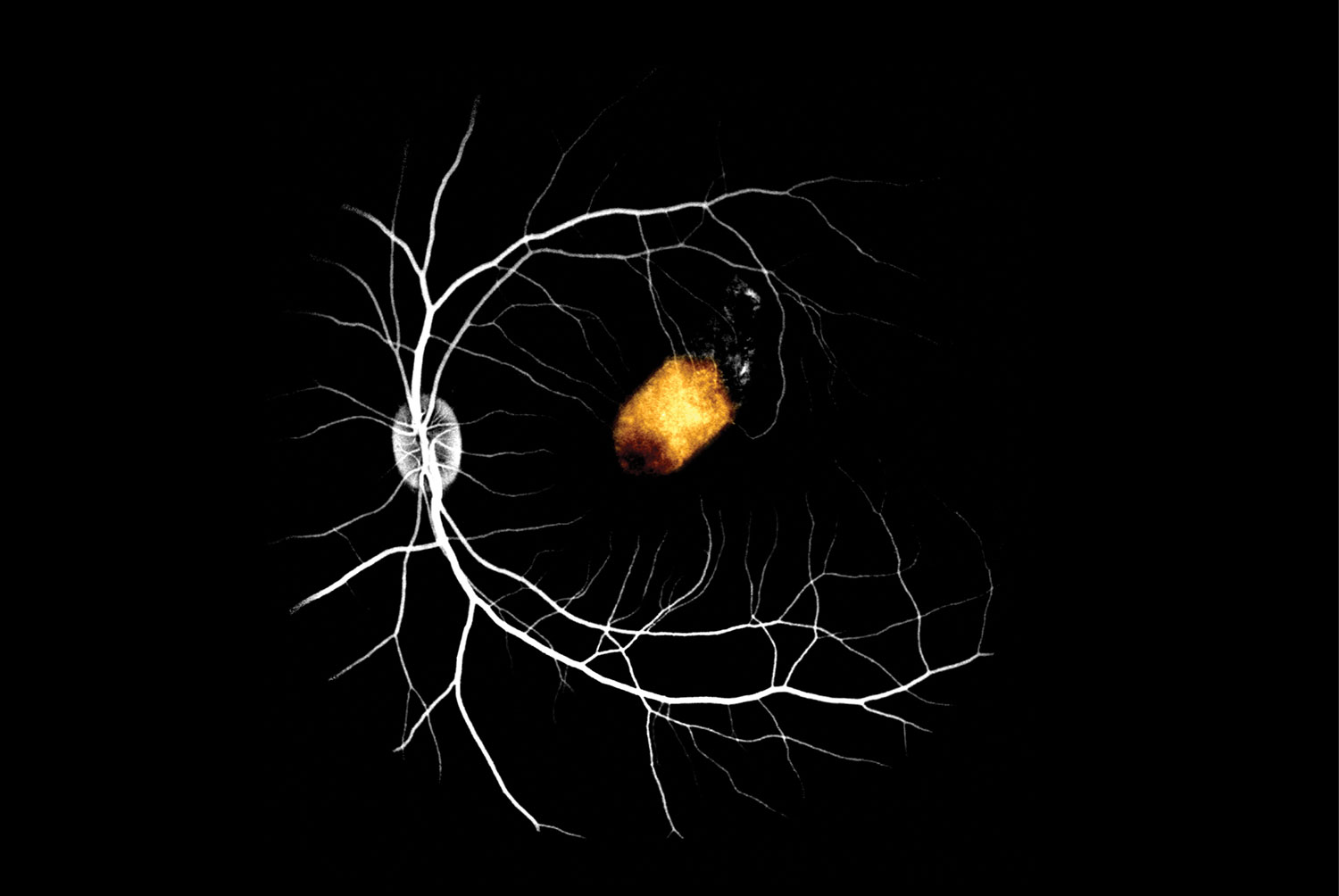
A team of researchers at NUS Medicine, led by Assistant Professor Su Xinyi, extracted retinal stem cells from donated cadaver adult eyes, grew them into RPE cells and transplanted them into the eyes of monkeys. They found that RPE patches transplanted under the monkey’s macula stably integrated for at least three months with no serious side effects. What is more, the stem cell-derived RPE partially took over the function of the monkey RPE and was able to support normal photoreceptor function.
Importantly, these cells did not undergo transformation to cause retinal scarring, or exhibit any other deleterious effect post-transplantation. Also, these unique cells have the potential to serve as an unlimited resource of human RPE, with the possibility of donor compatibility matching.
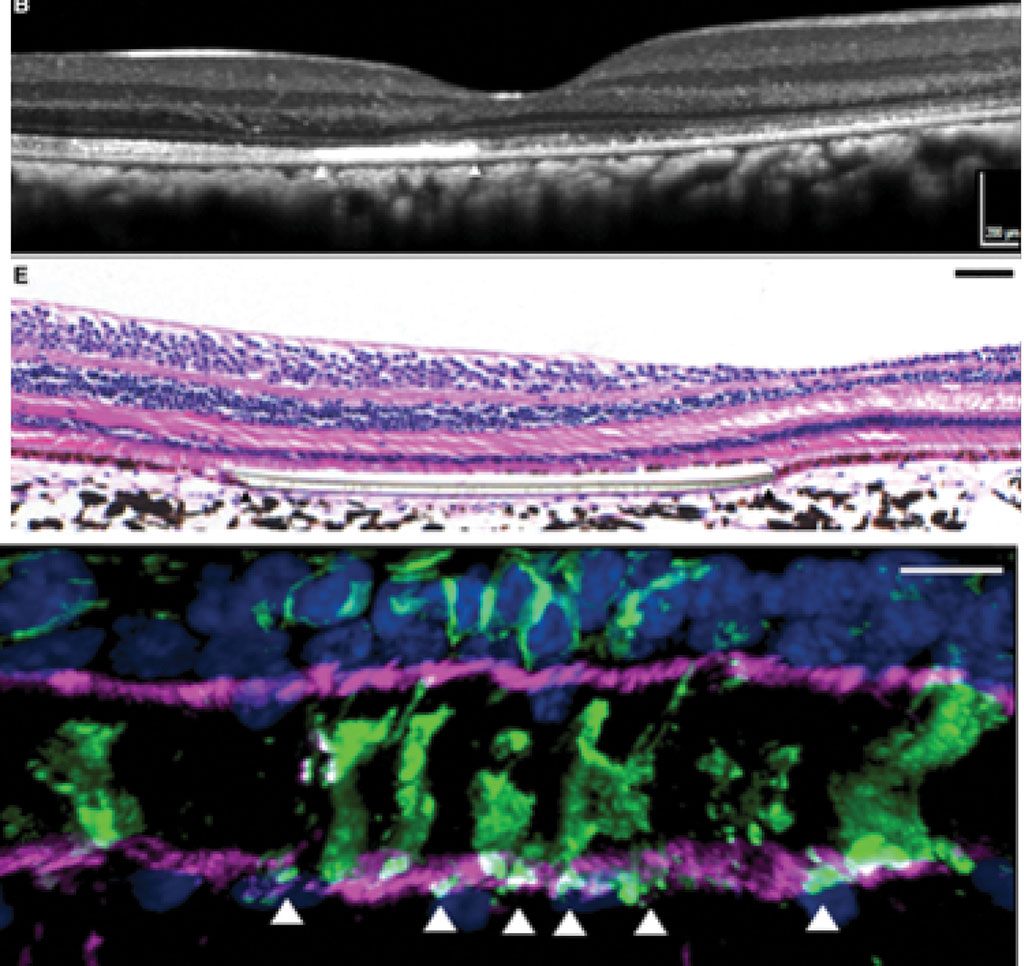
Transplanted RPE demonstrated functional phagocytosis by the presence of internalised rod photoreceptor outer segments stained with rhodopsin (white arrowheads) within transplanted RPE. (Credit: A/Prof Su Xinyi)
Altogether, this demonstrates the feasibility of using adult retinal stem cell-derived RPE transplants to replace defective RPE as a possible treatment for macular degeneration. However, further experiments need to be conducted. This includes evidence to demonstrate adult retinal stem cell-derived RPE can restore vision in diseased non-human primate models, and eventually in regulatory human clinical trials. Nonetheless, this proof-of-principle study is an important early step in validating this approach.
By demonstrating the success of a stem cell transplant to re-establish a new RPE monolayer in preclinical models, A/Prof Su and colleagues offer hope to the many millions of people who are losing their sight to AMD and other macular degenerative diseases.
“These results encourage optimism that hRPESC-RPE may become a promising alternative source of RPE for cell replacement therapy for patients with RPE-dysfunction-related vision loss. In the near future, we hope to conduct first-in-man clinical trials to further validate these results,” said A/Prof Su.
“These results encourage optimism that hRPESC-RPE may become a promising alternative source of RPE for cell replacement therapy for patients with RPE-dysfunction-related vision loss. In the near future, we hope to conduct first-in-man clinical trials to further validate these results.”
A/Prof Su Xinyi
“I am honoured to be part of this international collaboration between Assistant Professor Tim Blenkinsop at the Icahn School of Medicine at Mount Sinai (New York) and Associate Professor Boris Stanzel from Eye Clinic Sulzbach (Germany).”
-
Wong WL, Su X, Li X, Cheung CMG, Klein R, Cheng C-Y. Global prevalence of age-related macular degeneration and disease burden projection for 2020 and 2040: a systematic review and meta-analysis. Lancet Global Health. 2014;2:e106-e116.