Finding Needles in the Cardiac Haystack
Clinician-scientists discover new biomarkers to predict heart failure after a heart attack.
Besides being a traumatic event, a heart attack (also known as a myocardial infarction) may damage or stiffen the heart, leading to a condition called heart failure.1 The occurrence of heart failure after a heart attack is truly a double tragedy for the affected patient. Just as the patient is starting to get back on his feet after a severe illness, another major wave crashes over him. In heart failure, the heart stops pumping blood properly causing severe breathlessness, markedly reduced stamina and reduction of quality-of-life.2 Heart failure results in frequent hospitalisations and one in five patients will die in five years.2 Heart failure is rising in prevalence worldwide, with 4.5% of people in Singapore affected by the condition.3
Identifying myocardial infarction patients who are at high risk of developing heart failure would enable doctors to intervene earlier and perhaps prevent heart failure from occurring. While hundreds of proteins have been found to be associated with the development of heart failure after a myocardial infarction, researchers still have to conduct extensive experimentation of each protein to determine if it can be a useful biomarker or possible drug target in heart failure after a heart attack. This is in essence a massive undertaking that is akin to looking for the proverbial needle in the haystack. A new study by Associate Professor Mark Chan from the NUS Yong Loo Lin School of Medicine and Senior Consultant of the Department of Cardiology at the National University Heart Centre, Singapore, Professor A. Mark Richards, NUS Yong Loo Lin School of Medicine and Senior Consultant of the Department of Cardiology and Deputy Director at the National University Heart Centre, Singapore, and colleagues combined two powerful new technologies to help accelerate this process of discovering new biomarkers and potential treatment targets to prevent heart failure after a heart attack.4
![]()
1 in 5
heart failure patients
will die in five years
4.5%
of people in Singapore
are affected by heart failure
Sifting Through the Haystack
This study, the results of which were published online ahead-of-print in the journal Circulation, involved patients from two countries who had experienced a myocardial infarction: 1) the Coronary Disease Cohort Study (CDCS), consisting of 500 patients in New Zealand, and 2) the Improving Outcomes in Myocardial Infarction through Reversal of Cardiac Remodelling (IMMACULATE) registry, comprising 200 patients in Singapore.
“This work, the result of bilateral and interdisciplinary collaboration, all skilfully coordinated by Assoc Prof Mark Chan, has taken us an important step closer to being able to step in post-heart attack and more fully protect patients from further harm.”
— Prof A. Mark Richards
The first powerful discovery technology that Assoc Prof Chan and team applied was large-scale plasma proteomics which uses short DNA strands called aptamers to simultaneously measure more than a thousand proteins in blood.5 The major advantage of this protein-profiling technology is that it is incredibly sensitive and can detect even minute quantities of individual proteins with high certainty. To ensure that the proteins they measured had actually increased because of changes in living cells, rather than through a non-specific release from dying heart muscle cells early after the myocardial infarction, the researchers waited one month after the myocardial infarction before taking blood samples and performing the assay.
Assoc Prof Chan and colleagues found more than 200 proteins that predicted the future onset of heart failure up to seven years after the myocardial infarction. They then cross-referenced the proteins of the greatest significance to the RNA fragments of more than 6,000 different individual cells from mice and humans with heart attacks and heart failure using the second powerful discovery technology called single-cell RNA sequencing. RNA is the product of our more than 20,000 genes (DNA). When genes are activated to produce a certain protein, cellular RNA production is increased. Because RNA are precursors of proteins, correlation between RNA from cells and proteins in the blood give greater assurance that the proteins discovered by the first technology are relevant to the disease process. By analysing the RNA content of single cells one at a time, instead of the more conventional method of analysing RNA from a large groups of cells en masse, the researchers were able to detect subtle but important changes in RNA expression in subpopulations of cells that would otherwise be missed with a bulk cell approach.
After hundreds of hours of bioinformatics analysis shifting through massive amounts of data, Assoc Prof Chan and colleagues found their ‘needles in the haystack’—six “highest-priority” proteins for other investigators to focus their efforts on, instead of testing several hundred proteins. Of these six proteins, two were already well-established biomarkers of heart failure after a heart attack—cardiac troponin T, and N-terminal B-type natriuretic peptide — that were secreted from heart muscle cells after a heart attack, giving them confidence about the other four proteins. The single cell RNA sequencing determined that two of these six proteins—thrombospondin 2 and latent transforming growth factor-β binding protein-4—originated not from heart muscle cells but from other cells within the scaffold in which heart muscle cells are embedded, called the extracellular matrix. To the surprise of the investigators, the sixth key protein was not secreted by either heart muscle or extracellular matrix cells but the inner lining of blood vessels, called the endothelium.
This study, the results of which were published online ahead-of-print in the journal Circulation, involved patients from two countries who had experienced a myocardial infarction: 1) the Coronary Disease Cohort Study (CDCS), consisting of 500 patients in New Zealand, and 2) the Improving Outcomes in Myocardial Infarction through Reversal of Cardiac Remodelling (IMMACULATE) registry, comprising 200 patients in Singapore.
The first powerful discovery technology that Assoc Prof Chan and team applied was large-scale plasma proteomics which uses short DNA strands called aptamers to simultaneously measure more than a thousand proteins in blood.5 The major advantage of this protein-profiling technology is that it is incredibly sensitive and can detect even minute quantities of individual proteins with high certainty. To ensure that the proteins they measured had actually increased because of changes in living cells, rather than through a non-specific release from dying heart muscle cells early after the myocardial infarction, the researchers waited one month after the myocardial infarction before taking blood samples and performing the assay.
Assoc Prof Chan and colleagues found more than 200 proteins that predicted the future onset of heart failure up to seven years after the myocardial infarction. They then cross-referenced the proteins of the greatest significance to the RNA fragments of more than 6,000 different individual cells from mice and humans with heart attacks and heart failure using the second powerful discovery technology called single-cell RNA sequencing. RNA is the product of our more than 20,000 genes (DNA). When genes are activated to produce a certain protein, cellular RNA production is increased. Because RNA are precursors of proteins, correlation between RNA from cells and proteins in the blood give greater assurance that the proteins discovered by the first technology are relevant to the disease process. By analysing the RNA content of single cells one at a time, instead of the more conventional method of analysing RNA from a large groups of cells en masse, the researchers were able to detect subtle but important changes in RNA expression in subpopulations of cells that would otherwise be missed with a bulk cell approach.
After hundreds of hours of bioinformatics analysis shifting through massive amounts of data, Assoc Prof Chan and colleagues found their ‘needles in the haystack’—six “highest-priority” proteins for other investigators to focus their efforts on, instead of testing several hundred proteins. Of these six proteins, two were already well-established biomarkers of heart failure after a heart attack—cardiac troponin T, and N-terminal B-type natriuretic peptide — that were secreted from heart muscle cells after a heart attack, giving them confidence about the other four proteins. The single cell RNA sequencing determined that two of these six proteins—thrombospondin 2 and latent transforming growth factor-β binding protein-4—originated not from heart muscle cells but from other cells within the scaffold in which heart muscle cells are embedded, called the extracellular matrix. To the surprise of the investigators, the sixth key protein was not secreted by either heart muscle or extracellular matrix cells but the inner lining of blood vessels, called the endothelium.
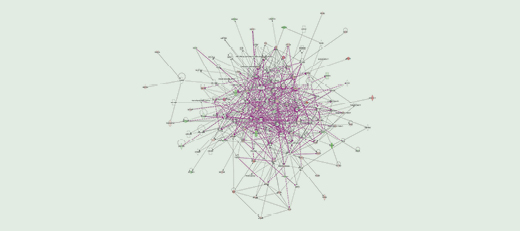
Network analysis of interconnected proteins and gene transcript in the combined plasma proteomics and single cell RNA analysis. Larger nodes indicate proteins/genes of potentially greater biological relevance to heart failure after a heart attack.
(Figure by Motakis Effymios)
Saving Lives: A Glimpse into the Future
![]()
Over 200
proteins that can predict
the future onset of heart failure are found
6
proteins were identified as biomarkers
of heart failure after a heart attack
Assoc Prof Chan and colleagues are now collaborating with biomedical engineers to develop ‘lab-on-chip’ devices to measure these proteins for user-friendly detection. Prof Richards has also completed work on some of these proteins showing that modifying their effect can accelerate recovery of heart function after a heart attack.
“Strong and reliable signals, identifying those patients who are unfortunate enough to incur heart failure following their heart attack, remain an urgent need,” said Prof Richards. “This work, the result of bilateral and interdisciplinary collaboration, all skilfully coordinated by Assoc Prof Mark Chan, has taken us an important step closer to being able to step in post-heart attack and more fully protect patients from further harm.”
Said Assoc Prof Mark Chan, “As a cardiologist who has spent a lot of time looking after patients with heart attacks in the last 10 years, it is disheartening to see patients develop heart failure even after performing emergency angioplasty for them in double-quick time. Paradoxically, by saving more lives, emergency angioplasty has actually led to more patients having heart failure after surviving a heart attack. He added, “This research would not have been possible 10 years ago, but recent technology has enabled us to measure thousands of blood proteins at once with large-scale plasma proteomics and sequence tens of thousands of RNA fragments one cell at a time with single-cell RNA sequencing, helping us to save time by focusing on the targets that matter most to predict and possibly find new treatments for heart failure after a heart attack. A big thank you to the 19 colleagues who worked tirelessly with me to deliver this important discovery.”
“This research would not have been possible 10 years ago, but recent technology has enabled us to measure thousands of blood proteins at once with large-scale plasma proteomics and sequence tens of thousands of RNA fragments one cell at a time with single-cell RNA sequencing, helping us to save time by focusing on the targets that matter most to predict and possibly find new treatments for heart failure after a heart attack.”
— Assoc Prof Mark Chan
Watch to find out more about this discovery!
REFERENCES
1 Mayo Clinic. Heart Failure. https://www.mayoclinic.org/diseases-conditions/heartfailure/symptoms-causes/syc-20373142. Updated 2020. Accessed August 28, 2020
2 Gerber Y, Weston SA, Enriquez-Sarano M, et al. Mortality associated with heart failure after myocardial infarction: a contemporary community perspective. Circ Heart Fail. 2016;9:e002460
3 Lam CSP. Heart failure in Southeast Asia: facts and numbers. ESC Heart Failure. 2015;2:46-49.
4 Chan MY, Motakis E, Tan S-H, et al. Prioritizing Candidates of Post-Myocardial Infarction Heart Failure Using Plasma Proteomics and Single-Cell Transcriptomics. Circulation…
5 Rohloff JC, Gelinas AD, Jarvis TC, et al. Nucleic acid ligands with protein-like side chains: Modified aptamers and their use as diagnostic and therapeutic agents. Mol Ther Nucleic Acids. 2014;3:e201.
