Pathogen Central
Have you ever wondered where viruses are studied? What goes into studying virus samples? Who are the people who support the day-to-day research operations? The answers lie inside the largest research-focused biocontainment facility in Singapore, currently housed on campus at Yong Loo Lin School of Medicine, and known as the Biosafety Level-3 Core Facility.

Opened in November 2014, the NUS Medicine Biosafety Level-3 (BSL-3) core facility is currently the largest research-focused biocontainment facility in Singapore that is properly equipped to handle work involving indigenous or exotic biological agents. At a time when COVID-19 is causing health, economic and social devastation around the world, the race to find a globally-viable vaccine has been running at full speed in the BSL-3 Core Facility at NUS Medicine.
BEHIND THE BSL-3 LABORATORY DOORS
A BSL-3 core facility is designed and certified to work on indigenous or exotic infectious agents, which can potentially develop into lethal diseases through inhalation. This includes viruses such as the West Nile virus, the causative agent of tuberculosis (Mycobacterium tuberculosis), and SARS-CoV-2. Experimental practices such as virus isolation and characterisation of viral agents recovered in cultures of specimens can only be handled in a specialised level three facility, where trained expertise is available.
The NUS Medicine facility has a suite of specialised equipment needed for diagnosis, in vivo and in vitro research on Risk Group 3 pathogens. Typically, biological labs are ranked from one to four, with one being lowest biosafety lab level and four being a highly specialised research laboratory that deals with deadly infectious agents such as Ebola.
Gazetted as Protected Place under the Infrastructure Protection Act and to achieve the highest biosafety and biocontainment, the entire infrastructure of the core facility, down to its Heating, Ventilation and Air Conditioning (HVAC) systems, have been specially designed to ensure no airborne particles can exit the enclosed space.
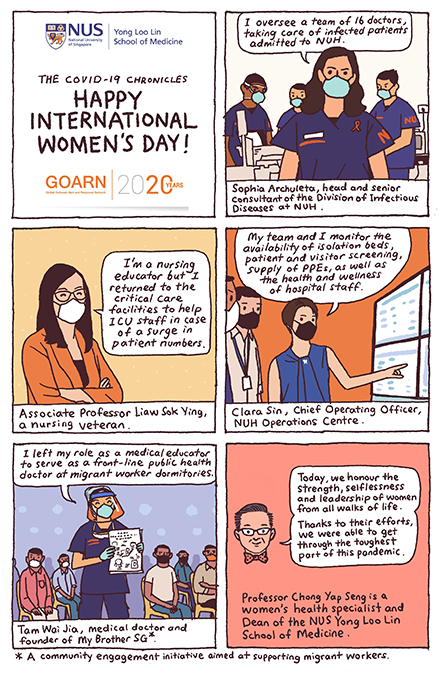
nIt takes competent and experienced, specially-trained personnel to run such a lab. They consist of the Operation Team, Research Team and Science Service Support Team, under the leadership of the BSL-3 Core Facility Director. From running engineering and lab operations to assisting in COVID-19 work alongside clinicians, and managing scientific programmes according to biorisk policies and guidelines, it takes tremendous work as well as the efforts of many to run a safe and efficient biosafety lab. These consistent efforts earned the NUS Medicine BSL-3 facility a reputation for managing a very comprehensive biorisk management programme.
KEY WORK IN INFECTIOUS DISEASES
As NUS Medicine is a founding institutional member of the National University Health System (NUHS), an academic health system, researchers at laboratory are able to tap on the wealth of resources at the National University Hospital (NUH) to fuel COVID-19 research.
nDisease surveillance is a key agenda of this core facility. The success of a national outbreak response depends on a well- managed surveillance programme for accurate and rapid diagnoses and outbreak responses, which in turn, could bring about a significant decrease in intensity and duration of disease outbreaks. In this regard, the NUS Medicine BSL-3 facility supports the National Public Health Laboratories in disease surveillance and plays an important role in combating endemic diseases including COVID-19, outbreak situations, and national emergencies of many highly infectious and zoonotic diseases of public health importance.u00a0
Besides, the laboratory simultaneously conducts research on potential treatments, therapies and vaccines.
nThe world will continue to see outbreaks and threats of new pandemics beyond COVID-19, amplified by globalisation, urbanisation and increased farming activity. As an international trade and commerce centre, Singapore is particularly susceptible infectious diseases, evident with outbreaks of Zika, H1N1 influenza, that have appeared after the Severe Acute Respiratory Syndrome (SARS) outbreak in 2003.
nSince infectious diseases remain a major burden for mortality and morbidity in Singapore, cutting-edge facilities like the NUS Medicine BSL-3 core facility are needed to improve surveillance and research technologies and capabilities, in anticipation of other novel infectious diseases.
How are scientists protected from viruses in the BSL-3 lab?n

All personnel entering the BSL-3 facility are highly trained

They wear dedicated, special Personal BSL-3 Protective Equipment (PPE)

This includes breathing through a Powered Air-Purifying Respirator (PAPR)
No personal belongings are allowed

Scientists observe appropriate safety equipment and practices

Labs are designed with negative pressure rooms, with clean air moving into the space in higher supply than the exhaust air leaving the facility
Air flows only in one direction

Exhaust air is High Efficiency Particulate Air (HEPA) filtered to remove tiny, airborne particles as part of contamination control
