Disruptive Behaviour: Why We Should Nip It in the Bud

by Dr Inthrani Raja Indran and
Associate Professor Tan Chay Hoon
Department of Pharmacology
The inevitable “disruption” in healthcare may be viewed with optimism, given the hope that technological advances can help drive improvement in patient outcomes. “Disruptive behaviour” in healthcare may be similarly perceived to be inevitable. However, it is important to recognise that such behaviour is a concern that needs to be urgently addressed, because of its impact on healthcare team members and the risk that it poses to patient care and safety.
According to the American Medical Association, disruptive behaviour is defined as “personal conduct, whether verbal or physical, that negatively affects or that potentially negatively affects patient care”.1 It is linked to a lack of professionalism and refers to language and actions that are inappropriate and uncivil. Commonly observed examples of disruptive behaviour include rudeness and disrespect, scolding of colleagues, abusive language and condescending actions.2
Causes of disruptive behaviour
Disruptive behaviour may be due to a wide range of factors linked to the individual and/or the working environment. Certainly, an individual’s personality and capability are key to determining how they interact and engage with other people. Some people may lack communication skills and/or the self-mastery that is critical for professionalism. Disruptive behaviour may also arise from mental health issues (such as depression) or factors such as stress, fatigue and illness.3
It has been shown that the high levels of stress that are typical of today’s healthcare working environment contribute to disruptive behaviour, particularly if there is pressure to see a large number of patients.4 The hierarchical structure of hospitals also likely contributes to this sort of behaviour, particularly if disruptive behaviour is learned by previous recipients of such behaviour and/or those who tolerate it, thus perpetuating and exacerbating the problem. In fact, disruptive behaviour may increase in frequency when uncivil behaviour is tolerated, which may in turn result when people refrain from comment so as to avoid being targeted themselves. As the working environment becomes increasingly toxic, patient interactions are eventually also affected, putting patient safety at risk.5

Impact of disruptive behaviour at the individual, team and institutional level
Various studies have examined the impact of disruptive behaviour, proving that it affects the healthcare team, patient care and safety as well as the healthcare institution.
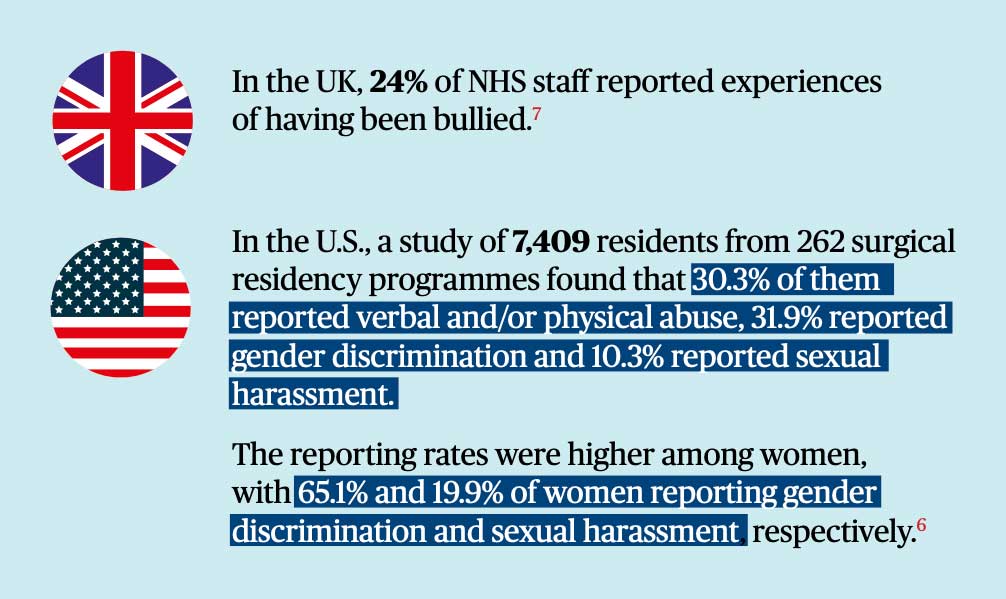
Effective communication and collaboration require that interpersonal interactions be respectful and civil. However, disruptive behaviour distracts people from their primary focus of patient care, reducing staff morale and job satisfaction. According to a recent study published in the New England Journal of Medicine, residents who reported experiencing discrimination, abuse, or harassment regularly (i.e., at least a few times per month) were more likely to show signs of burnout than residents who did not report such experiences.6
Disruptive behaviour renders the members of the healthcare team reluctant to discuss and cooperate in an open manner, undermining their ability to work together as a team. Fear of criticism and reprimands may cause anxiety that increases the risk of medical error, which may also adversely impact the quality of patient care.4
Therefore, there is risk to the healthcare institution that arises due to concerns not only regarding patient safety, but also staff engagement and retention. In fact, a 2018 study estimated that the financial cost of bullying and harassment in the UK’s National Health Service (NHS) is approximately £2.28bn (USD 2.96bn) per year. This cost is due to absence (including sick leave), loss of productivity among staff who are physically present (“presenteeism”), staff turnover as well as compensation and litigation costs.7
How prevalent is disruptive behaviour in healthcare?
Examples of Disruptive Behaviour3
- Use of language that is inappropriate, profane, rude, disrespectful, insulting, demeaning or abusive
- Shaming or reprimanding of colleagues or staff in front of colleagues, patients and/or visitors
- Inappropriate arguments
- Unnecessarily excessive negative comments about another healthcare team member
- Outbursts of anger, including throwing or breaking of objects
- Bullying behaviour
- Non-clinical comments (including jokes) about race, religion, sexual orientation, age, physical appearance, socioeconomic status or educational background
- Refusal to adhere to established protocols or practice standards
What should be done?
Given the potentially negatively impact on patient care and safety, it is critical to address the problem of disruptive behavior at both the individual and organisational level.5 However, there may be less attention paid to disruptive behaviour where the harm caused is not overt. Similarly, while it is important to address patterns of such behaviour, it should be noted that single occurrences do also exert potential significant impact on members of the healthcare team. As disruptive behaviour may be endorsed as a rite of passage required to develop resilient trainees, it is important to highlight that the quality of a training programme is determined by its content, structure and rigour, not by fear and incivility.
A key first step to address disruptive behaviour would be to raise awareness of the issue, so people recognise that disruptive behaviour is a problem that requires identification and intervention8. For example, a survey of final year medical students (n=68) revealed that a majority (86.8%) of the respondents did not feel prepared to manage the problem of disruptive behaviour if they encounter it. Therefore, it is important to educate students and healthcare professionals so that they recognise disruptive behaviour and know how to respond. It is also important that institutions clarify their expectations of professional behaviour by describing ethical conduct policies, e.g., a code of conduct.8
A second step to address the problem of disruptive behaviour would be to enable open and effective interprofessional communication, e.g., through interprofessional education. As it is specifically designed to promote collaboration between the different healthcare professions, interprofessional education enables a better understanding of other people’s perspectives and roles, fostering empathy for both patients and fellow healthcare team members, and equipping them with skills in emotional intelligence.
Finally, it is important to inculcate appropriate values to promote respect, collegiality, collaboration and teamwork among members of the healthcare team. The “EnRICH” programme currently under development at the Yong Loo Lin School of Medicine is part of a key new initiative to support the personal and professional development of our students. It is a longitudinal mentorship programme that complements the five-year medical curriculum, and aims to nurture the School values of respect, integrity, compassion and humility. To facilitate their transition from student to professional, the EnRICH programme provides students with the opportunity for facilitated discussion and guided reflection with peers and mentors.
These three steps are just the beginning of a long process needed to effect the necessary changes in our healthcare system, to mitigate the impact of disruptive behaviour on patient care and healthcare teams at the individual, group and institutional level.
REFERENCES
1 American Medical Association. Opinion 9.045. Physicians with disruptive behaviour. https://www.ama-assn.org/delivering-care/ethics/physicians-disruptive-behavior.
2 Rosenstein AH, Russell H, Lauve R. Disruptive physician behavior contributes to nursing shortage. Study links bad behavior by doctors to nurses leaving the profession. Physician executive 2002;28:8–11.
3 Davies M, Dinwoodie M. The disruptive doctor. BMJ 2018;351:h3553. doi:10.1136/bmj.h3553.
4 Leape LL, Shore MF, Dienstag JL, Mayer RJ, Edgman-Levitan S, Meyer GS, Healy GB. Perspective: a culture of respect, part 1: the nature and causes of disrespectful behavior by physicians. Acad Med. 2012 Jul;87(7):845-52. doi: 10.1097/ ACM.0b013e318258338d.
5 Felblinger DM. Bullying, incivility, and disruptive behaviors in the healthcare setting: identification, impact, and intervention. Frontiers of health services management 2009;25:13–23. doi:10.1097/01974520-200904000-00003.
6 Hu YY, Ellis RJ, Hewitt DB, Yang AD, Cheung EO, Moskowitz JT, Potts JR 3rd, Buyske J, Hoyt DB, Nasca TJ, Bilimoria KY. Discrimination, Abuse, Harassment, and Burnout in Surgical Residency Training. N Engl J Med. 2019 Oct 31;381(18):1741- 1752. doi: 10.1056/NEJMsa1903759. Epub 2019 Oct 28.
7 Kline R, Lewis D. The price of fear: estimating the financial cost of bullying and harassment to the NHS in England. Public Money & Management 2018;October:1–10. doi:10.1080/09540962.2018.1535044.
8 Oliveira RM, Silva LM, Guedes MV, Oliveira AC, Sánchez RG, Torres RA. Analyzing the concept of disruptive behavior in healthcare work: an integrative review. Rev Esc Enferm USP. 2016 Jul-Aug;50(4):695-704. doi: 10.1590/S0080- 623420160000500021
