About
25 – 50%
of OSA cases contribute to secondary hypertension
1 billion
adults are affected by obstructive sleep apnea

Issue 48
Nov 2023
AFFAIRS OF THE HEART
by Professor Ronald Lee Chi Hang, Department of Medicine, Yong Loo Lin School of Medicine, National University of Singapore and Senior Consultant, Department of Cardiology, National University Heart Centre, Singapore

Obstructive Sleep Apnea (OSA) is a persistent sleep disorder marked by recurrent instances of either partial or complete collapse of the upper airway during sleep. This disruption in normal breathing leads to fragmented sleep patterns, fluctuations in intrathoracic pressure, reduced oxygen levels (hypoxemia), and heightened sympathetic activity.
It’s estimated that a staggering one billion adults are affected by OSA, with a substantial proportion experiencing moderate-to-severe forms of the condition.
About
25 – 50%
of OSA cases contribute to secondary hypertension
1 billion
adults are affected by obstructive sleep apnea
Notably, OSA often intersects with hypertension, as around half of OSA patients simultaneously battle this cardiovascular concern. In fact, the 2017 Hypertension Guidelines jointly issued by the American College of Cardiology and American Heart Association indicate that OSA contributes to 25 – 50% of cases of secondary hypertension.
Although OSA is prevalent in individuals with obesity, its reach extends even further due to distinct craniofacial traits among the Asian population. This specific anatomical characteristic renders them particularly vulnerable to OSA. Strikingly, a significant number of Asian patients with OSA exhibit lower body mass indices compared to their Caucasian counterparts, highlighting the nuanced nature of the disorder across different ethnic groups.
The utilisation of continuous positive airway pressure (CPAP) to manage OSA does exhibit a modest reduction in blood pressure (BP). However, the challenge lies in the suboptimal acceptance and tolerance of CPAP treatment among OSA patients. As an alternative therapeutic avenue, mandibular advancement devices (MADs) have garnered endorsement as per guidelines. MADs are particularly recommended for OSA patients who cannot or do not tolerate CPAP.
Nonetheless, the existing body of evidence regarding the comparative efficacy of MADs versus CPAP in terms of blood pressure reduction is somewhat constrained. Current data primarily stem from short-term studies, and although randomised trials have undertaken a comparison between MADs and CPAP, their findings have suggested comparable effects on lowering blood pressure. It’s worth noting, however, that these trials grapple with certain limitations, such as relatively small sample sizes, the inclusion of patients lacking hypertension, the exclusion of severe OSA cases, and a relatively brief intervention period spanning one to three months.
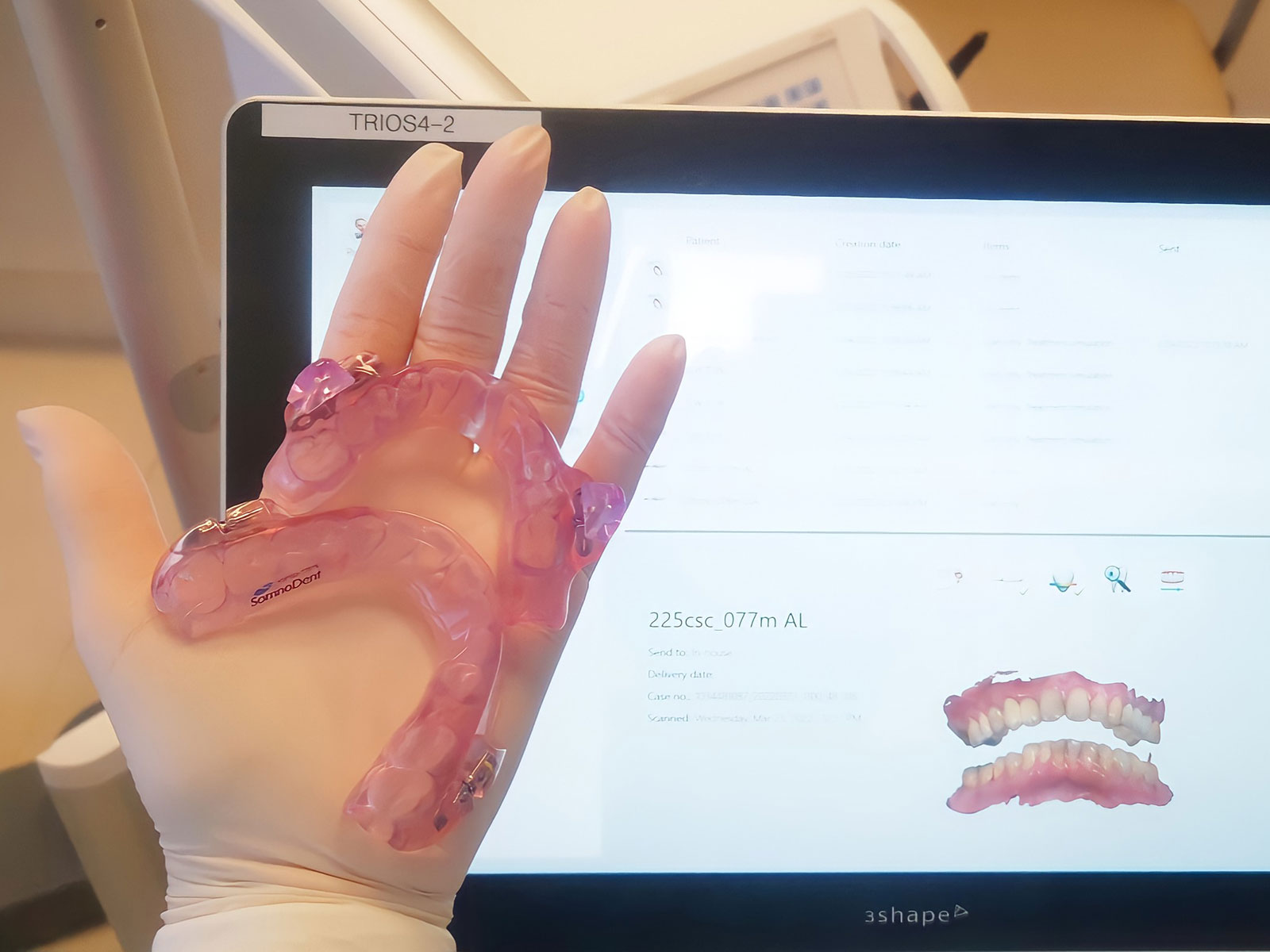
MADs are recommended as an alternative treatment tool for patients with OSA that cannot tolerate CPAP.
We hypothesise that by repositioning the lower jaw to enhance upper airway openness during sleep, the mandibular advancement device (MAD) could offer heightened effectiveness, especially among Asian patients whose OSA stems primarily from a restrictive craniofacial structure. In the CRESCENT study (Cardiosleep Research Program on Obstructive Sleep Apnoea, Blood Pressure Control, and Maladaptive Myocardial Remodelling – Non-inferiority Trial, registered at clinicaltrial.gov under NCT04119999), our objective is to assess whether the treatment of moderate-to-severe OSA through the application of MAD yields improvements in BP and other pertinent health-related outcomes in comparison to CPAP.

Participants of the CRESCENT trial were subjected to a rigorous treatment regimen, administered by specialised practitioners in the form of either MAD or CPAP interventions.
With the marked prevalence of OSA in the Asian population and the considerable advantages associated with significant BP reduction, including pertinent data from Chinese cohorts, the findings of the CRESCENT trial will play a pivotal role in shaping healthcare recommendations. The CRESCENT study, initiated by the National University Heart Centre Singapore with funding from the National Medical Research Council of Singapore in March 2019, underwent a meticulous evaluation process involving both international and Singaporean peer reviews. Our investigation concentrated on Chinese participants, identified with a documented history of physician-diagnosed hypertension and elevated cardiovascular risk. These individuals underwent comprehensive polysomnography screening overnight.
Subsequent to diagnosis, participants exhibiting OSA were subjected to a rigorous treatment regimen, administered by specialised practitioners in the form of either MAD or CPAP interventions, as per the stipulated study protocol, spanning a duration of 12 months. The operational backbone of this initiative is reinforced by a team of adept clinical research coordinators, ensuring smooth coordination and providing indispensable administrative support.
The observation window extends over a period of 12 months, with the primary focal point being the alteration in mean arterial blood pressure over a 24-hour cycle, juxtaposing baseline metrics against those obtained at the six-month juncture. Complementary to this pivotal metric, an array of secondary endpoints is assessed, encompassing systolic and diastolic BP measurements across a 24-hour spectrum, inclusive of daytime and nocturnal phases. Pulse pressure, nocturnal blood pressure dip (characterised by a nocturnal decrease of over 10% in BP), percentage of participants achieving systolic blood pressure levels below 130 mmHg and 120 mmHg at follow-up instances, arrhythmia evaluation through four-day electrocardiographic monitoring, meticulous biomarker and proteomic analysis, assessment of cardiovascular magnetic resonance-derived myocardial fibrosis and remodeling, in addition to comprehensive quality-of-life questionnaires, collectively contribute to the holistic evaluation of outcomes.
Subsequent to diagnosis, participants exhibiting OSA were subjected to a rigorous treatment regimen, administered by specialised practitioners in the form of either MAD or CPAP interventions, as per the stipulated study protocol, spanning a duration of 12 months.
Inception of participant recruitment took place on October 2019, culminating on 5 December 2022, thereby encapsulating a comprehensive recruitment phase spanning 38 months. The primary outcome of the CRESCENT trial will be available in the first quarter of 2024.

The research team behind the CRESCENT trial.
More from this issue
AFFAIRS OF THE HEART
Nipping Cardiovascular Disease in the Bud
A WORLD IN A GRAIN OF SAND
Antibodies, The Magic Bullets (Zauberkugel) in Medicine
THE BANYAN TREE
The Science (and Art) of Doing in Health
