Issue 48
Nov 2023
A WORLD IN A GRAIN OF SAND
By Associate Professor Paul A. MacAry, Department of Microbiology and Immunology, YONG LOO LIN SCHOOL OF MEDICINE, NATIONAL UNIVERSITY OF SINGAPORE (NUS MEDICINE), and Director, Life Sciences Institute
One of the key foundational principles of drug development in modern medicine is Zauberkugel, a German translation for magic bullets. This defines the ability of a medicine to target and treat disease-causing microbes and/or mechanisms without harming the human host.
In the late 1800s, Louis Pasteur’s epoch-making research established the ‘Germ Theory’ of disease. As a result of Pasteur’s observations, the prevalent dogma amongst physicians at the time was that all human disease could be linked directly to ‘toxins’ released by microbial pathogens that infect the blood and organs. At this time, human populations were afflicted by recurrent outbreaks of deadly infectious diseases such as diphtheria (caused by the Gram-positive bacilli Corynebacterium diphtheriae) and tetanus (caused by the Gram-positive anaerobe Clostridium Tetani), where secreted exotoxins drive the underlying pathology. This was at a time before the advent of toxoid vaccines or the discovery of Penicillin in the 1920s, and thus, there were no prophylactic or therapeutic interventions that could be used for these diseases.
In the 1890s, contemporaries of Pasteur, Emil Von Behring, a German physician, and Shibasaburo Kitasato, his Japanese student, published their discovery that graduated doses of heat-killed diphtheria bacilli derived from the cadavers of German children who died of this lung infection, could be injected into rabbits. These rabbits produced substances in their blood (antitoxins) that neutralised the toxins produced by Corynebacterium diphtheriae. As part of the same experiment, they also showed that the antitoxins produced by one animal could be passively transferred in serum to protect another animal showing early symptoms of diphtheria infection.
This great discovery was subsequently confirmed by peers like Robert Koch (the ‘grandfather’ of Microbiology). Von Behring concluded that this anti-toxin effect was mediated by undetermined substances that he called ‘immuno-bodies’. He combined the two words (Immuno-body and anti-toxin) to give us ‘Antibody’, which represents one of the earliest descriptions of immunisation.
Following experimentation in animals, Von Behring treated diphtheria infections in a group of German school children using 50ml of serum derived from immunised rabbits and showed that he could effect a reduction in their mortality. He then established a collaboration with the German bacteriologist Paul Erlich, a Nobel Laureate in 1908, who developed methods to enrich and quantify the anti-toxin effects in animal serum. Erlich described these antibodies as ‘Zauberkugel’ or Magic Bullets, because they target and treat the microbial pathogen without harming the human host.
What Erlich had in mind was a scene from his favourite opera Der Freischütz. In this opera, Max, a useless huntsman, forms a pact with the devil, who gives him magic bullets that will always hit their mark. Thus, this concept of Zauberkugel is one of the foundational principles that underlies all drug discovery in modern Medicine.
With Erlich’s help, the production of animal anti-serum was scaled up from rabbits to horses, and from the end of the 1890s to the 1930s, it became the principal treatment provided to patients with diseases like diphtheria and tetanus.
Building upon Erlich and Von Behring’s observations for infectious diseases, a French Physician, Charles Richet, removed tumour cells from a group of patients with sarcoma, and injected these cells into dogs to raise anti-serum, then treated the patients with the dog anti-serum. He observed that while several of the treated patients showed a transient improvement in their symptoms, none were cured. These findings were reported in a manuscript entitled “’Physiologie Pathologique’- de la serotherapie dans la traitment du cancer” Published in 1895 in Comptes Rendus Hebd Seane Acad Sci, this represents the first documented example of using immunotherapy to treat cancer.
Richet was treated with derision by the French medical establishment who either dismissed or caricatured his research. However, Richet’s efforts paid off and he had the last laugh when he was awarded the Nobel Prize for Medicine and Physiology in 1913, based on his description of anaphylaxis. He then went on to become one of Europe’s most respected physicians.
The magic bullet – Too good to be true?
While serum therapy proved efficacious for treating infections, it also came with significant risks. The horse serum used to treat infected patients was full of complement, stress factors, serum albumins and other contaminating proteins derived from the horse. These could cause severe rheumatic-like reactions in treated patients. Termed ‘serum sickness’, many of them suffered joint and renal inflammation. Thus, when alternative approaches for prophylaxis (Toxoid vaccines) or therapy (Penicillin) became widely available, serum therapy was dropped as a frontline treatment, and antibody-based magic bullets were largely shunned in Medicine for the next 60 years.
Development of antibodies into modern medicines
The development of antibodies into modern medicines required a number of new discoveries. The first of these was made in the 1950s, when a veterinarian from Ohio State University called Bruce Glick identified the cells that are the source of antibodies. Glick was interested in analysing the physiological role of an organ in the chicken that looks like a human appendix. This organ is termed the Bursa of Fabricus, which is named after an Italian anatomist, Hyronimus Fabricus (1533-1619), who produced volumes of illustrations of birds.
Many of the most important medicines developed in the last thirty years to treat malignant or inflammatory diseases are humanised antibodies and a significant proportion of ongoing efforts in drug discovery by global Pharma is based on making new antibody medicines.
The Bursa of Fabricus was described as a sac connected to the dorsal part of the cloaca. To define the role of this organ, Glick developed a surgical procedure termed a bursectomy, to excise the organ, and submitted these chickens to a battery of physiological tests. His key finding was that bursectomised chickens cannot make antibody responses, regardless of how strongly they are immunised. The cells that are prevalent in the Bursa of Fabricus, known as B cells, were identified and defined as the cells that make antibodies.
Glick’s attempts to have these findings published in top scientific journals were rejected and this pivotal discovery for Immunology ended up in ‘Poultry Science’ (published in 1954). The mammalian equivalent of the Bursa of Fabricus Cells were subsequently identified in the bone marrow and spleen of rodents and humans.
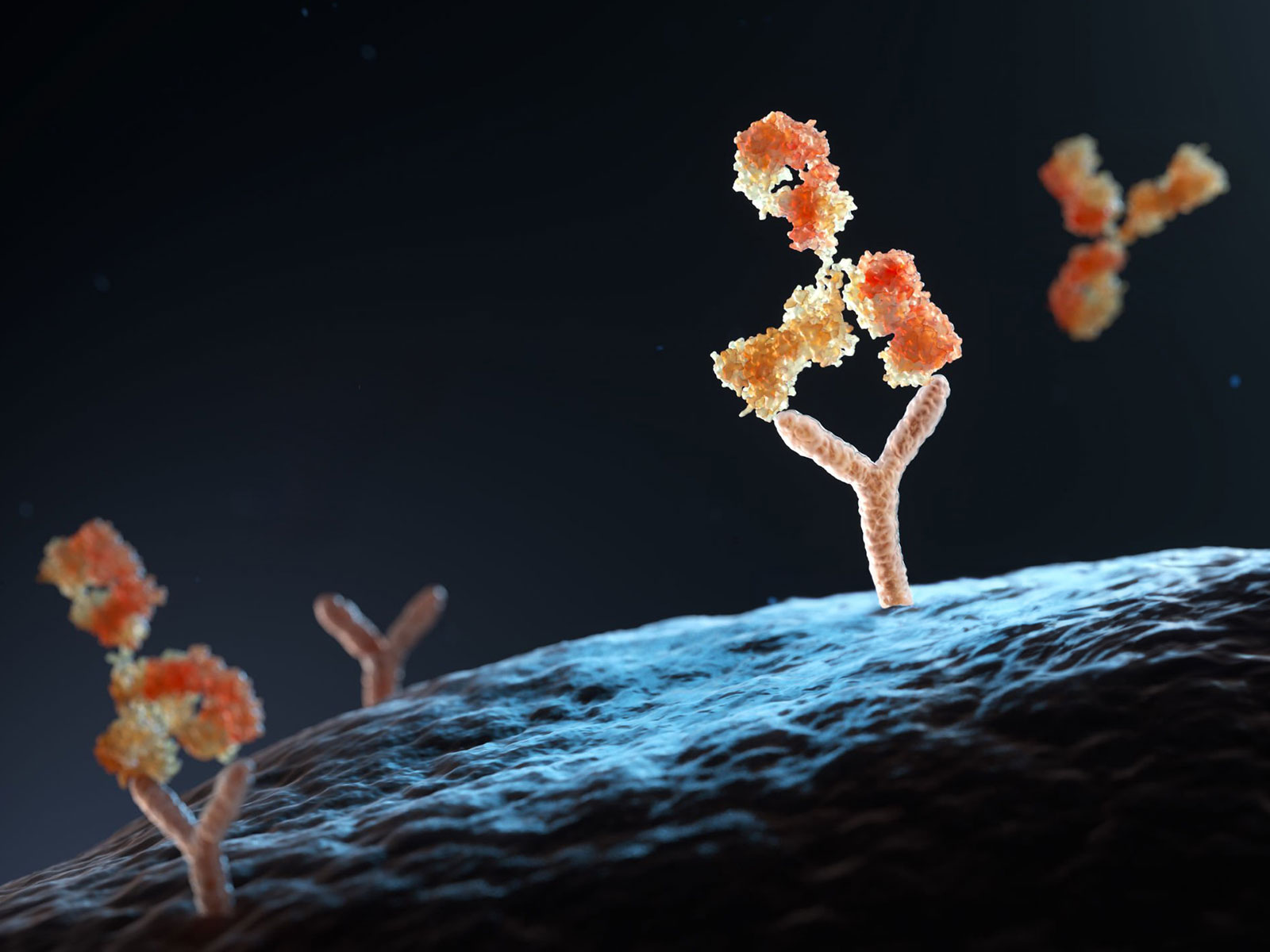
Twenty years after the discovery of B cells, Caesar Milstein and Jorges Köhler (Nobel Prize winners for Physiology and Medicine in 1984) invented a new method to immortalise B cells, through fusing them with tumor cell lines to form Hybridomas1. The resulting hybridoma cells can be diluted into single-cell cultures and expanded in vitro. The net result is a culture of immortalised cells derived from single-cell clones that produce an antibody of a single specificity, and this is termed as a monoclonal antibody.
The capacity to create antibodies of a single specificity that can be produced in large quantities in vitro created an explosion of interest in exploiting these molecules for human therapy. However, the method developed by Milstein and Kohler only worked for mice and rats. Thus, from 1975 through to the mid-1990s, mouse or rat monoclonal antibodies were raised against human disease markers by immunising them with the relevant human markers and proteins. This included receptors that can be targeted on human tumor cells or factors (such as cytokines) that drive inflammatory disease.
A further refinement that improved the safety and efficacy of antibody-based medicines was the development of methods to make rodent antibodies more suitable for humans. These methods involve exploiting principles of molecular engineering, where the small regions of rodent antibody proteins that provide the specificity for the therapeutic target are pasted onto human antibody scaffolds. The resulting proteins are 90 – 95% humanised with a small number of components retained from the original rodent antibody to ensure the required specificity2.
Many of the most important medicines developed in the last 30 years to treat malignant or inflammatory diseases are humanised antibodies (Humira, Remacade, Retuxan, Herceptin, Keytruda and Avastin as examples) and a significant proportion of ongoing efforts in drug discovery by global Pharma is based on making new antibody medicines. Thus, while it has taken over 100 years, the Zauberkugel has finally fulfilled the promise envisioned by Von Behring and Erlich.
Continuous cultures of fused cells secreting antibody of predefined specificity. Köhler G, Milstein C. Nature. 1975 Aug 7;256(5517):495-7. doi: 10.1038/256495a0.
Reshaping human antibodies for therapy. Riechmann L, Clark M, Waldmann H, Winter G (1988). Nature. 332 (6162): 323–7.
More from this issue
PEOPLE OF NUS MEDICINE
Discovering Coding’s Joys on an Internship

AFFAIRS OF THE HEART
Repositioning the Lower Jaw for Improved Sleep and Better Blood Pressure


