
Issue 47
Aug 2023
ALL IN THE FAMILY
by Dr Amrish Soundararajan, Family Physician (NUS Medicine '17), Co-founder, MedicHelix Pte Ltd, MBA Candidate, University of Chicago Booth School of Business ('25), DR Wayne Han Lee, Associate Consultant, National University Polyclinics and Assistant Group Chief Technology Officer at National University Health System

The popularity of artificial intelligence (AI), especially of ChatGPT and generative AI, has kindled interest in its applications in healthcare. The technology’s potential to revolutionise healthcare services has generated debate about how this may affect family physicians. However, we believe that the undifferentiated presentations that family physicians deal with on a daily basis as well as the relationship and communication-centric nature of our jobs mean that we are not at risk of losing our shirts in the near future.
In fact, we take a more expansive view—family physicians should play a critical role in driving healthcare innovation. Our ability to practise in diverse settings, our proximity to patients, and our intimate understanding of the spectrum of primary-to-tertiary care, make us well-placed to guide the development and implementation of digital-health technologies.
In this piece, we explore the need for innovation in primary care, share about digital-health projects in primary care that we have been involved in, and attempt to inspire fellow practitioners to play an active role in shaping the future.

Photo credit: National University Polyclinics
Our ability to practise in diverse settings, our proximity to patients, and our intimate understanding of the spectrum of primary-to-tertiary care, make us well-placed to guide the development and implementation of digital-health technologies.”
Technology in family medicine – The need and the promise
Family Medicine today is at an important crossroad. In Singapore and many other developed countries, primary care systems face immense and unprecedented stresses, due to ageing populations and burgeoning chronic disease epidemics. A US study published last year showed that primary care providers need a staggering 26.7 hours a day, over the course of a year, to render comprehensive care to an average-sized panel of 2,500 patients. This data-point illuminates the need for innovation across the primary care ecosystem in order to deliver the care that our patients deserve—be it care models, healthcare technology, or public health policy. At the same time, there is a growing abundance of technology platforms and data that the healthcare industry can draw on to innovate, experiment, and solve problems with.
Drawing parallels from other industries, we see great potential for technology to transform the “patient experience” in primary care. Consider Mr Tan, who manages to open a new multi-currency savings account with a few clicks online and has a seamless experience consulting a banker about investment products based on the information that the bank already knows about him. Mr Tan can also order biking gear online if he decides to pick up road-biking; he can try riding a new bicycle at a brick-and-mortar store, and have everything consolidated and delivered right to his doorstep in a few days.
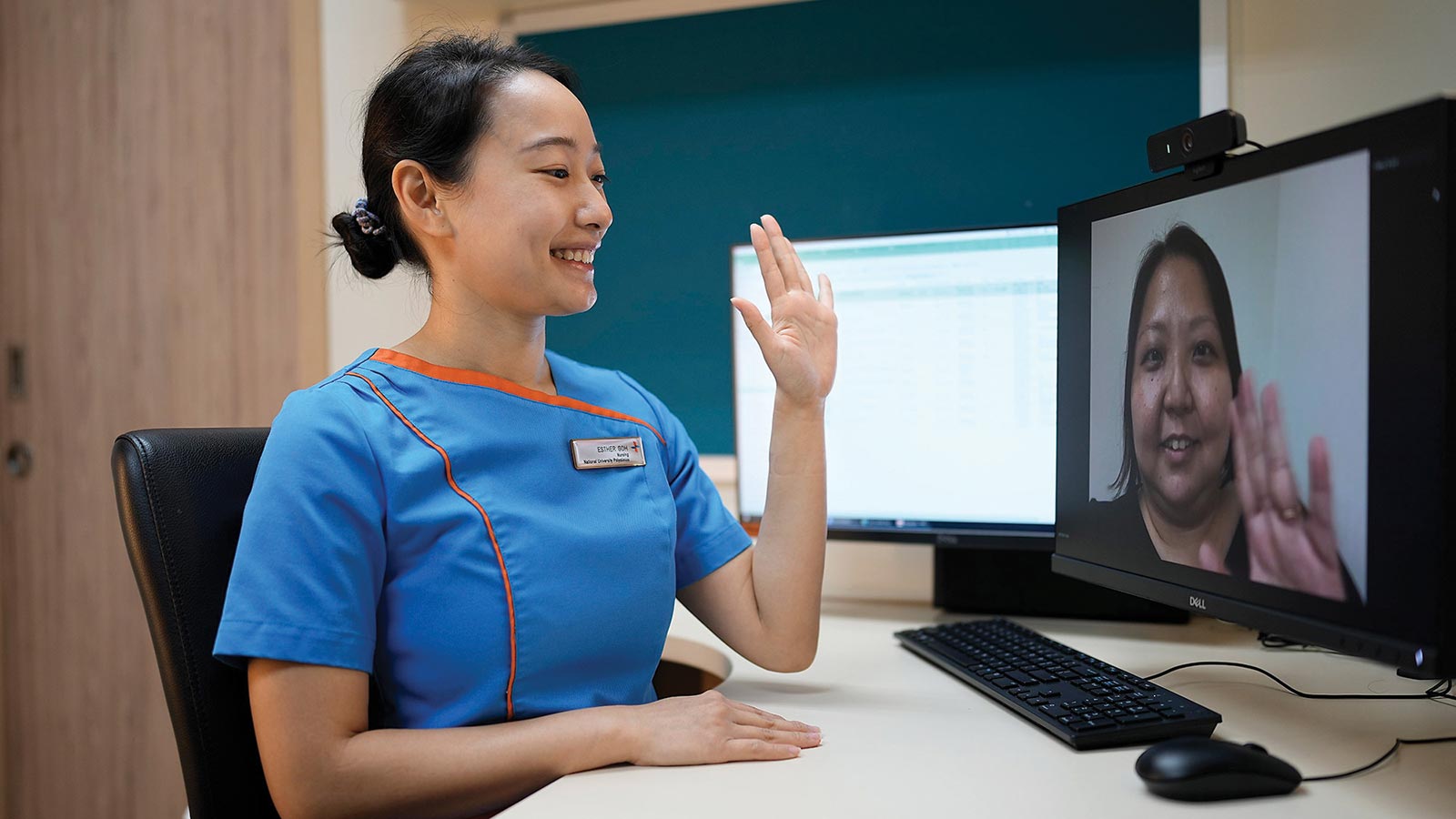
Photo credit: National University Polyclinics
Contrast that with Mr Tan’s experience as a patient. The week before an appointment, he makes a trip down to a crowded clinic for a fasting blood test, starving and waiting. During his last teleconsultation, half the time was spent recounting blood pressure and blood sugar readings that he had diligently recorded. On the day of his appointment, he queues again for an hour, and finally meets his physician. It’s a whirlwind discussion of lab results, self-monitoring, diet and exercise. An appointment with a dietitian? That’s another trip on another day! Feeling overloaded with information, he is told his next follow-up will be in three months’ time. Once again waiting in line (at the pharmacy now), Mr Tan wonders if one day his healthcare experience could be as seamless, tailored, and convenient as his banking and retail experiences.
We believe that in the near future, innovation in primary care will revolve around these key drivers: efficient personalisation, data integration and interoperability, and “omni-channel” care delivery. “Omni-channel” is an idea borrowed from other service industries like retail and banking. The goal of omni-channelling is to create a seamless patient-centred healthcare experience across multiple channels, from clinic-based to the home, from in-person to virtual, and from synchronous to asynchronous. In the following examples from Singapore, we highlight how some teams are trying to push the envelope on these fronts, to reimagine the “patient experience”.
We believe that in the near future, innovation in primary care will revolve around these key drivers: efficient personalisation, data integration and interoperability, and 'omni-channel' care delivery.”
CHAMP: An institution-based experience with big data integration & AI in primary care
The “Iron Triangle” of health care is the trade-off between access, cost and quality. By incorporating AI, the National University Health System (NUHS) aims to expand the boundaries of the Iron Triange—improving access to specialised expertise and enhancing the quality of care, at low marginal costs. “CHAMP”, NUHS’ Chronic Disease Management Programme, seeks to deliver the right type of care, to the right type of patients, by carefully considering care complexity and patients’ digital proficiency, leveraging data integration, and empowering the entire care team.
CHAMP has developed a WhatsApp chatbot, targeted at appropriate patient segments based on the categories illustrated in Figure 1. This benefits patients as they are able to interact with the chatbot to submit real time parameters (e.g. blood pressure readings), while the chatbot nudges, engages and motivates the patient towards a healthier lifestyle. As an institution, NUHS then leverages end-to-end integration of data like lab tests, prescriptions and medical histories. This enables personalised clinical decision support not only to primary care physicians, but also to the wider care team of allied health professionals, enabling them to deliver the right type of care to the right type of patients.
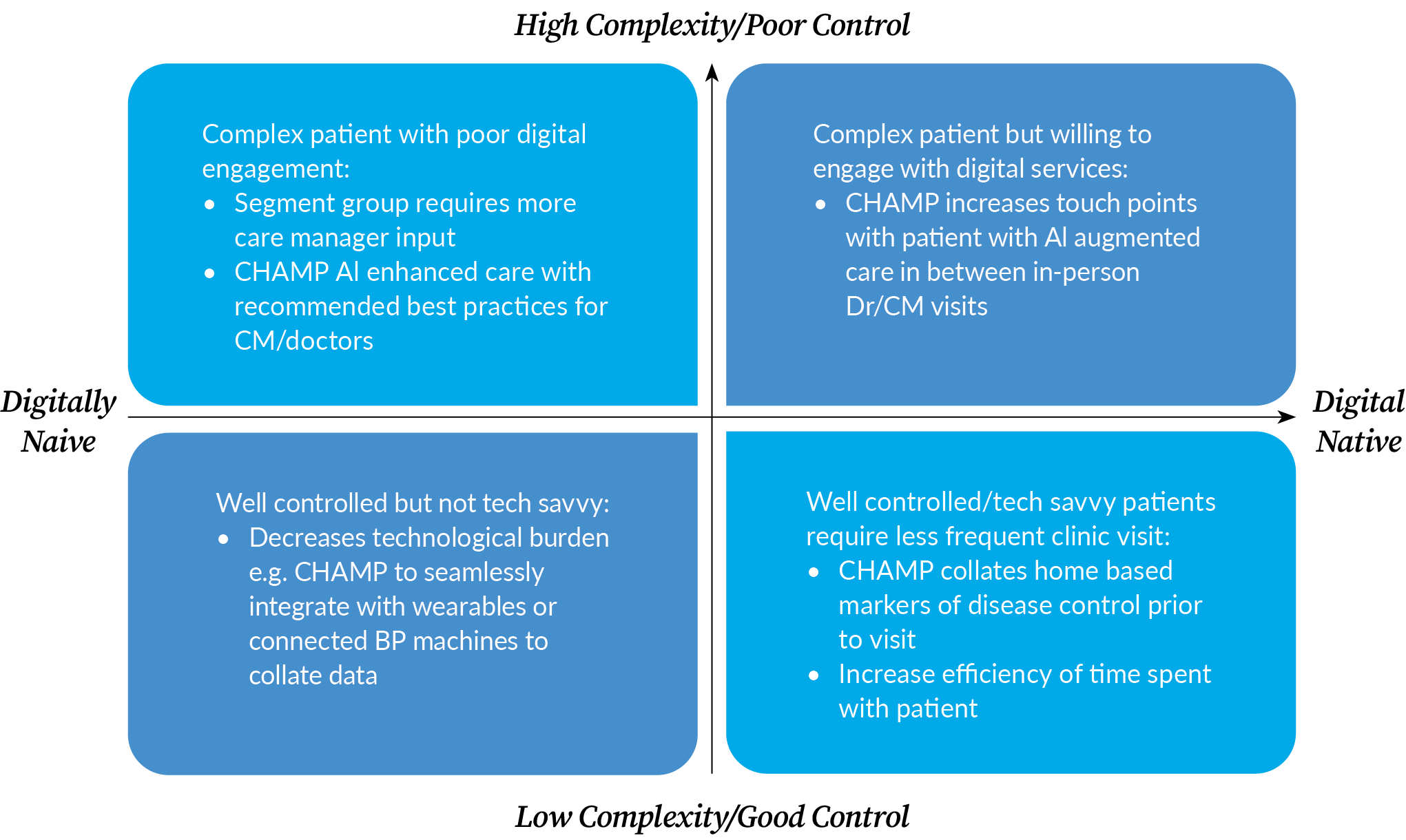
Figure 1: NUHS CHAMP sorts patients into categories such as digital natives vs. digitally naive and low complexity vs. high complexity.
HelixCare: Automated data integration and decision-support for primary care
In the more fragmented private healthcare sector, there is an unmet need for infrastructure that integrates decision-critical data from various sources, to create personalised management plans (such as the Health Plan under HealthierSG), which can then be drawn upon during any form of consultation. One team working on this area is MedicHelix, an early-stage startup born out of pain points observed by two young family physicians in their practice.
Personalising preventive and chronic treatment plans takes a lot of time. Family doctors have to assimilate data like lab test results, past prescriptions and self-monitored readings such as blood pressure, glucose and weight, and analyse that data in the context of the patient’s medical history in order to identify and communicate actionable insights. To make this process more efficient, MedicHelix has developed a cloud-based decision-support tool called HelixCare. By gathering parameters through an automated software interface or manual entry, HelixCare automatically generates guideline-adherent, personalised, chronic and preventive treatment plans. When integrated with a Clinic Management System, HelixCare can reduce the physician’s cognitive load by serving up relevant data during consultations. This frees up room for physicians to engage their patients more seamlessly, establish therapeutic alliances and focus on patient education and empowerment.
The implementation of any new technology in healthcare needs to show proofs of concept, feasibility, and value over time. Whether reviewing cost-effectiveness in public healthcare institutions, or testing business models in startups, we can be effective conduits between stakeholders and direct collaborative efforts towards these goals.”
Family Physicians as leaders, dreamers and collaborators
Having taken on active roles in projects like those mentioned above, we feel that there is a lot of potential for fellow family physicians to get involved in healthcare innovation. As a profession, we have the contextual understanding to identify areas for improvement and gaps in care delivery. As individuals, we can dream big and brainstorm for innovative solutions.

Photo credit: National University Polyclinics
Healthcare innovation is a complex, multidisciplinary effort, and we can try to bring stakeholders and the right technical talent to the same table to work together. In our various places of practice, we can try to inspire a shared vision, and leverage our communication skills to anchor collaboration. We can encourage our teams to innovate and take risks and embrace change. The implementation of any new technology in healthcare needs to show proofs of concept, feasibility, and value over time. Whether reviewing cost-effectiveness in public healthcare institutions, or testing business models in startups, we can be effective conduits between stakeholders and direct collaborative efforts towards these goals.
Family physicians need not be bystanders buffeted by the winds of change. By adopting an enterprising spirit, embracing uncertainty, and by playing to the strengths of our profession, we can be leaders, dreamers and collaborators. We can shape the future of Family Medicine, to get even better at doing what we do—addressing personal, primary and preventive needs of our patients through comprehensive, continuing and coordinated care.
More from this issue

AFFAIRS OF THE HEART
Obesity Will Be the Leading Risk Factor for Heart Attacks within Three Decades


