The Gel’s The Key: Eyeing Better Outcomes for Retinal Detachment
Senior Manager, Research Division
Imagine having to lie face down for weeks, as well as not being able to go on flights for months. This is the reality for many patients after surgery to repair a detached retina. Now, a discovery from researchers at NUS Medicine, A*STAR and Singapore Eye Research Centre (SERI) may one day lead to the end of such difficult post-surgery requirements.
The vitreous humor is a clear, gel-like substance that fills the space in the eye between the lens and retina. As we age, the vitreous becomes more liquid. This increases the risk of retinal detachment.1 In the surgical management of many retinal disorders, the vitreous often has to be removed and replaced postoperatively by a temporary substitute such as an inert gas or silicone oil. These agents serve as a tamponade agent, allowing the retina to be re-attached to the back of the eye.
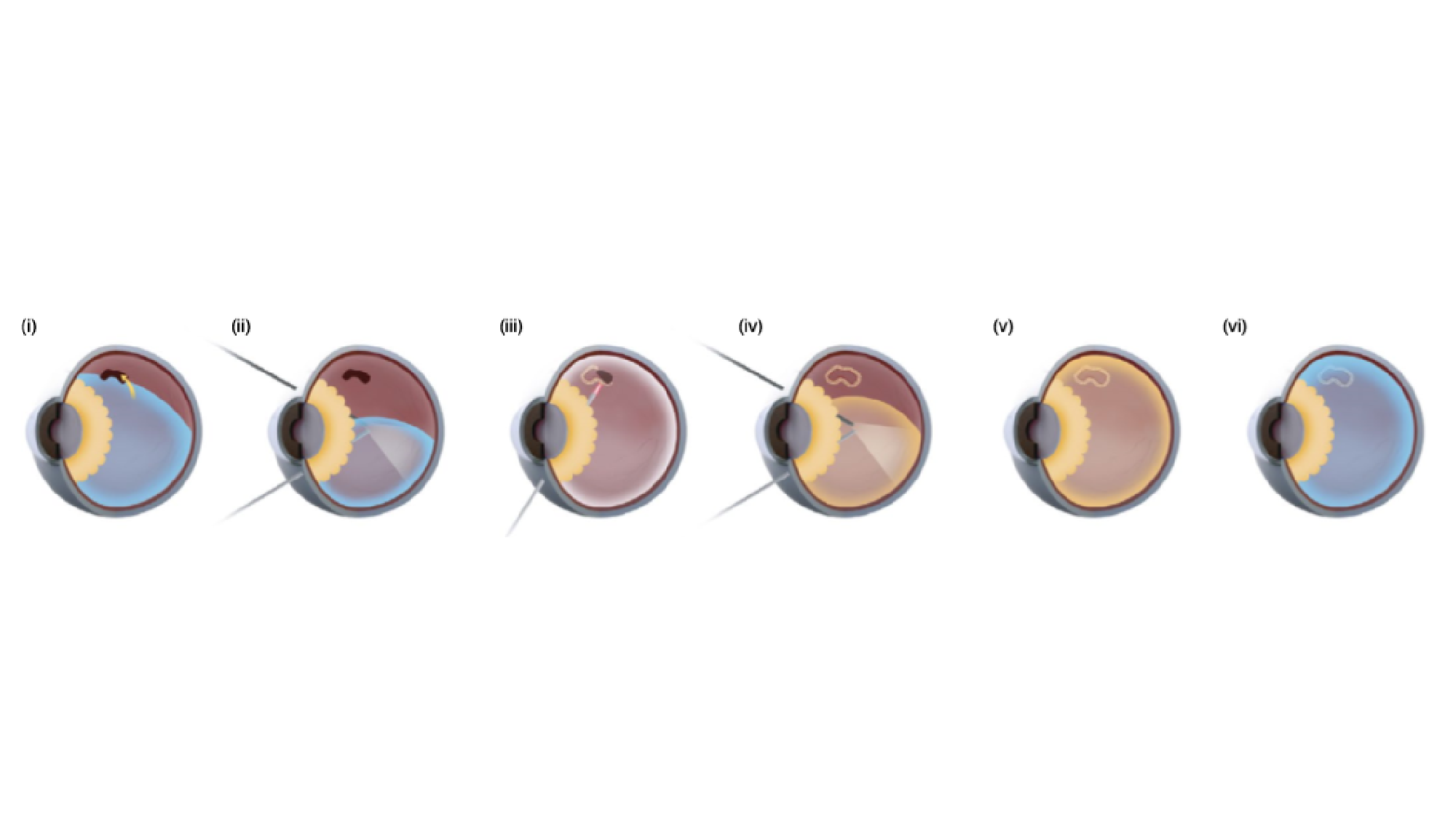
Figure 1
However, current tamponade agents have many drawbacks. Inert gases require patients to remain face-down for a prolonged period of time postoperatively. This allows the gas to provide sufficient support to the posterior part of the eye. Air travel is not recommended because low atmospheric pressure could cause the gas tamponade to expand and result in a vision-threatening rise in eye pressure. Gases are also associated with the formation of cataracts. Silicone oil is toxic to the eye if left for prolonged periods. Hence, an additional removal surgery is required after the retina has re-attached.1,2 Hence, a new tamponade agent without these disadvantages will be an attractive alternative for patients who are undergoing surgery for retinal detachment repair.
Working together with researchers from the Institute of Materials Research and Engineering (IMRE) and the Institute of Molecular and Cell Biology (IMCB), A*STAR, NUS Medicine researchers tested a new temperature-sensitive hydrogel as an alternative tamponade agent. This hydrogel was previously created by Dr Xian Jun Loh, Head of the Soft Materials Department at A*STAR, and has since been commercialised for applications such as cosmetic fillers. When clinician scientist, Assistant Professor Su Xinyi, from the Department of Ophthalmology at NUS Medicine was looking for a novel material capable of solving the disadvantages of current endotamponade agents, Dr Loh’s hydrogel presented an intriguing possibility.
“The thermogel has the potential to transform vitreo-retinal surgery. This is the first description of using advanced biomaterials to facilitate the replacement of ocular tissues in-vivo to form a vitreous-like body.” — Assistant Professor Su Xinyi, Department of Ophthalmology
The hydrogel consists of a thermosensitive, biodegradable polymer called EPC. At 25°C the polymer is in a liquid state, and can be injected easily through a small bore needle. Once injected into the eye, it quickly changes into a gel state due to the exposure to body temperature, mimicking the surface tension and consistency of the natural vitreous./span>
In the study, the team demonstrated the biocompatibility of EPC-7% gel for up to 6 months after injection into the vitreous cavity (Figure 1). In those eyes, the cornea remained clear with no cataract formation, and retina function was preserved (Figure 2). In addition, they also demonstrated that the gel was able to function as an endotamponade agent to support the detached retina for up to 1 year. These findings were published in the August issue of Nature Biomedical Engineering.3
Another, very surprising finding was as the EPC-7% gel biodegrades, it was able to facilitate the reformation of a vitreous-like body by 3 months post-surgery. This reformed vitreous-like body is rich in vitreous structural proteins such as collagen and hyaluronon-binding proteins. The researchers hypothesise that the hydrogel may act as a scaffold structure, which enables the newly-synthesised proteins produced by the eye, to organise into a structure that closely resembles the vitreous body.
Earlier in May 2019, the researchers started a spin-off company, Vitreogel Innovations Pte Ltd, with an aim to bring this technology to the clinic. If successful, the technology will be a disruptive innovation in vitreo-retinal surgery, and will revolutionise patient care.
As Dr Su says, “The thermogel has the potential to transform vitreo-retinal surgery. This is the first description of using advanced biomaterials to facilitate the replacement of ocular tissues in-vivo to form a vitreous-like body.”
References
1. Los LI, van der Worp RJ, van Luyn MJ, Hooymans JM. Age-related liquefaction of the human vitreous body: LM and TEM evaluation of the role of proteoglycans and collagen. Invest Ophthalmol Vis. Sci. 2003;44:2828-2833.
2. Su, X. et al. Recent progress in using biomaterials as vitreous substitutes. Biomacromolecules. 2015;16:3093-3102.
Acad Sci. 2012;109:E2579-E2586.
3. Stappler T, Morphis G, Irigoyen C, Heimann H. Is There a Role for Long-Term Silicone Oil Tamponade for More than Twelve Months in Vitreoretinal Surgery? Ophthalmologica. 2011;226(suppl 1):36–41.
4. Liu Z, Liow SS, Lai SL, et al. Retinal-detachment repair and vitreous-like-body reformation via a thermogelling polymer endotamponade. Nat Biomed Eng. 2019;3:598-610.
