New Gastric Cancer Programme Combines Most Promising Research and Clinical Avenues
The SGCC, which comprises scientists and clinicians from various disciplines who work on gastric cancer (GC), has already made considerable inroads in the scientific understanding, screening and prevention of the disease. The programme has also established large cohorts for studying GC and developed a blood test for early GC detection that is currently being marketed in Europe.
GC is the fifth most common cancer and the third leading cause of cancer death worldwide.1 It is more prevalent in East Asia than other parts of the world, with 60 per cent of new cases occurring there. In Singapore, it is responsible for nearly six per cent of deaths in men and women.2
The high mortality rate associated with GC is due to the fact that the cancer is often diagnosed at a late stage, when effective treatment options are scarce. Early-stage GC is actually curable, either by removal of cancer cells during endoscopy or via “keyhole” surgery involving small incisions in the abdomen. If the cancer is detected and treated while it is still restricted to the stomach, five-year survival rates are approximately 70 per cent. Survival drops considerably (down to 5 to 30 per cent) for later-stage cancers that have spread to other sites beyond the stomach.3
Given these facts, one of the focuses of the SGCC programme is the early detection and prevention of GC.
The research team will continue to optimise the blood test for early GC (which detects small RNA tumour markers called microRNA), and evaluate the performance of a new genetic test for identifying patients infected with Helicobacter pylori, a major risk factor for GC. These efforts will help to stratify people who are at higher risk for GC, and who can then be followed up with endoscopy and more frequent monitoring. If cancer is detected, it can be treated with less invasive methods, with a relatively good prognosis. “This non-invasive blood test will greatly simplify the diagnosis of gastric cancer and allow for early intervention. Currently there is no reliable blood test for the diagnosis of gastric cancer. Our test, if approved, will be the first blood-based test for detection of gastric cancer in the world,” Associate Professor Yeoh Khay Guan told reporters recently.
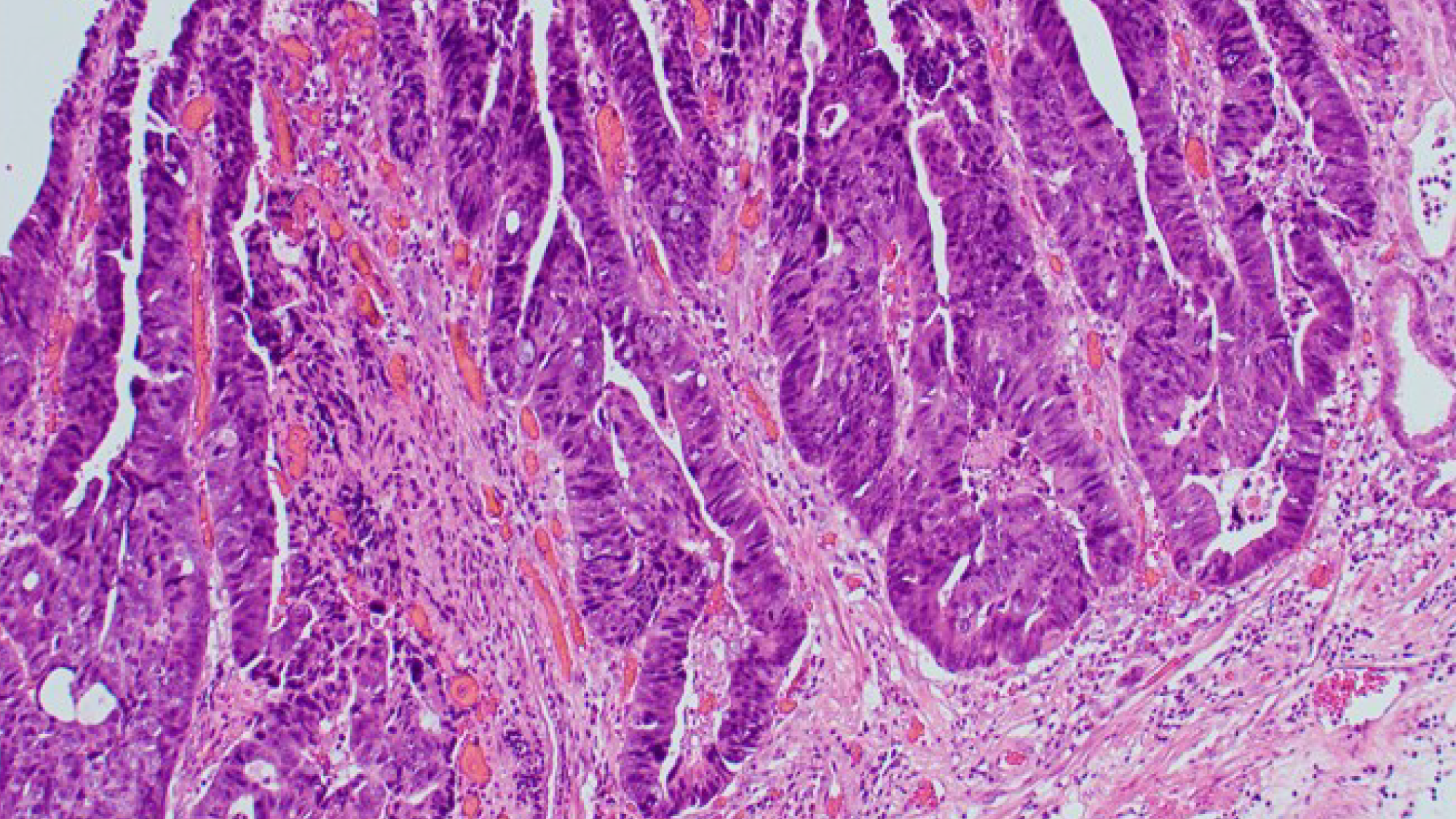
An image of Gastric Cancer cells
Another research theme involves the development of precision GC therapies that target different forms of GC called molecular subtypes. After establishing three-dimensional cultures of GC cells (“gastric organoids”) with unique molecular subtypes, the research team will test the efficacy of various combinations of cancer treatments for the different GC subtypes represented by the organoids.
A particularly severe complication of GC is peritoneal carcinomatosis (PC), in which cancer cells spread from the stomach to the abdominal cavity. Untreated patients with this condition have a terrible prognosis, surviving for only one to three months.4, 5 Current treatments improve survival but, even with treatment, only 40 to 60 per cent of patients survive for one year.6
The third research area aims to address this problem by evaluating the clinical efficacy of a new delivery method, pressurised intraperitoneal aerosol chemotherapy (PIPAC). The PIPAC method delivers chemotherapy and immunotherapy to the abdominal cavity via an aerosolised spray, which could provide better coverage of the affected area.
Since developing new preventions and therapies for GC will hinge on having a better understanding of the disease, the programme will also focus on basic scientific research on the pathogenesis of GC. The fourth and fifth research themes will involve studying GC stem cells, which the SGCC researchers have already isolated and identified. The researchers will drill down to the level of a single stem cell and determine its genetic sequence. The idea is to characterise the molecular changes in the cells from which the cancer originates, and understand how these changes contribute to the heterogeneous gastric tumour and its response to cancer drugs.
Ultimately, the goal of the ambitious, multidisciplinary programme is to use the best anticancer weapons available to move the needle of survival for this deadly cancer.
References
1. World Health Organization. Global Cancer Observatory. Cancer Fact Sheets: Stomach.
http://gco.iarc.fr/today/data/factsheets/cancers/7-Stomach-fact-sheet.pdf.
Accessed April 17, 2019.
2. National Registry of Diseases Office. Singapore Cancer Registry Annual Registry Report 2015
3. National Cancer Institute. Surveillance, Epidemiology, and End Results Program (SEER). Cancer Stat Facts: Stomach Cancer.
https://seer.cancer.gov/statfacts/html/stomach.html.
Accessed April 17, 2019.
4. Okines A, Verheij M, Allum W, Cunningham D, Cervantes A; for the ESMO Guidelines Working Group. Gastric cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2010;21 Suppl 5:v50-v54.
5. Yonemura Y, Elnemr A, Endou Y, et al. Multidisciplinary therapy for treatment of patients with peritoneal carcinomatosis from gastric cancer. World J Gastrointest Oncol. 2010;2:85–97.
6. Glehen O, Gilly FN, Arvieux C, et al. Peritoneal carcinomatosis from gastric cancer: a multi-institutional study of 159 patients treated by cytoreductive surgery combined with perioperative intraperitoneal chemotherapy. Ann Surg Oncol. 2010;17:2370-2377.

Members of the SGCC team. Front row: Prof Patrick Tan from Duke-NUS Medical School, Assoc Prof Yeoh Khay Guan, Prof Yoshiaki Ito. Backrow: Dr Yong Wei Peng, Adj Prof Melissa Teo from the National Cancer Centre, Singapore, and Prof Jimmy So
