Recreating Liver Tumours as Organoids for Faster, More Accurate Drug Screening
Hepatocellular cancer (liver cancer) is the second leading cause of cancer deaths in the world, responsible for almost 750,000 mortalities in 2012.1 In Singapore, it ranks as the third and fourth leading cause of cancer death for men and women, respectively. Liver cancer claims so many lives because diagnosis often occurs only when the cancer has already advanced. Available treatments are also sorely lacking, with only three approved drugs besides chemotherapy.2
An essential part of developing new treatments is to test potential candidate drugs in preclinical models; only the most effective candidates will move on to being tested in humans. For liver cancer, a big challenge is that current preclinical tumour models do not closely reflect features of the liver tumour and the tumour environment in humans. This causes many potential drugs to fail when they are tested in humans.
To more closely mimic the features of human tumours, researchers have developed models of liver tumours called patient-derived xenografts (PDX). This involves taking a small tissue sample from patients. Although these models provide a more accurate picture of how effective potential cancer drugs would be in humans, they are also expensive and time-consuming to create. Growing these PDX cancer cells in culture would be more cost effective for drug screening. However, so far, attempts to culture these cells fail to reflect the 3D tumour structure and the tumour environment.
“These tumour avatars have the potential to revolutionise the development of liver cancer drugs.”
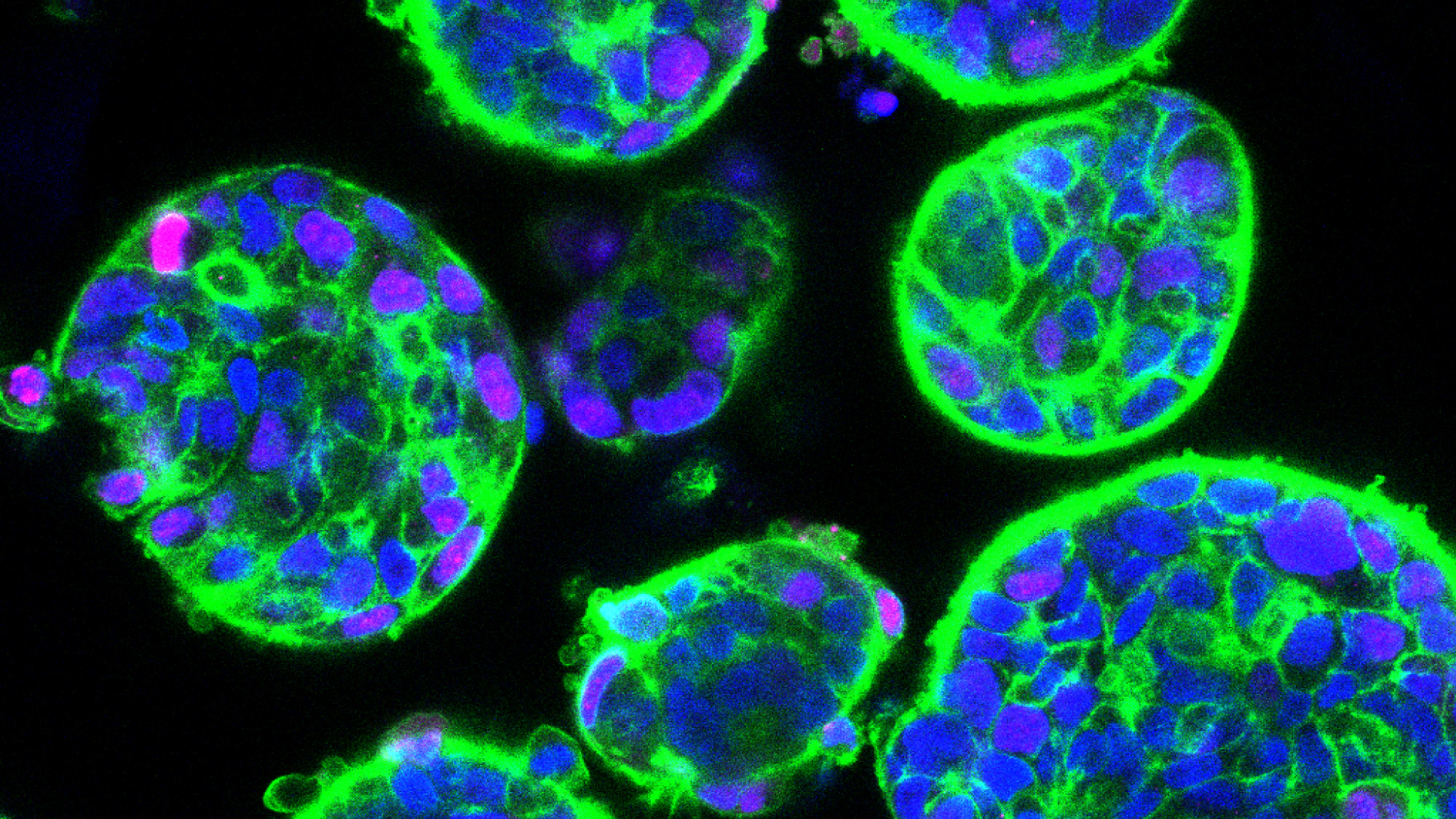
HCC organoids in culture
Led by Dr Eliza Fong and Dr Toh Tan Boon, an interdisciplinary team of researchers at the NUS Departments of Physiology and Biomedical Engineering, the Cancer Science Institute of Singapore, the Institute of Bioengineering and Nanotechnology, A*STAR and the National Cancer Centre Singapore has now devised a new method to grow PDX liver cancer cells in culture.
As described in their recent paper in the leading bioengineering journal Biomaterials, this method involves growing the cells on synthetic 3D scaffolds made of a plant-based porous hydrogel. By optimising the biochemical and mechanical properties of the spongy scaffolds, the researchers developed a framework to help the liver cancer cells maintain their proper shape and function and grow as organoids. The team grew organoids from PDX taken from 14 liver cancer patients.
After growing the organoids for between one and three weeks, the team verified that the liver cancer cells in the organoids were alive and reproducing. Liver cancer cells usually contain specific genetic changes that are absent in normal liver cells. Most of the 14 organoids retained the same key genetic changes that were in the source PDX cells. They also maintained an important feature of liver tumours called intra-tumour heterogeneity, in which distinct populations of liver cancer cells are present within the same tumour and affect its response to treatment. The presence of this feature was another advantage for drug screening that the organoids possess over traditional cell culture methods, in which all cells are identical.
As a bioengineer, Dr Fong finds the success of the engineered organoids to be particularly rewarding. “This study truly epitomises the positive synergy we can achieve in growing patient tumours outside the body by marrying advances in tissue engineering with cancer biology,” she said.
Another attractive feature is the small size of the 3D scaffolds containing the organoids – a mere 100 microns. That is the diameter of a human hair. The tiny scaffolds can easily fit inside the well of a 96-well microtiter plate, a standard platform for high-throughput drug screening, which involves testing many drugs at the same time. Through this technology, one PDX can be used to produce tens to hundreds of such organoid-containing scaffolds. Combined with their ability to retain the genetic features and heterogeneity of the original liver tumours, these tumour avatars have the potential to revolutionise the screening and development of liver cancer drugs.
Dr Hanry Yu, Professor of Physiology at NUS Medicine and Group Leader of Tissue Engineering at the Institute of Bioengineering and Nanotechnology at A*STAR, as well as the last author of the study, pointed out that “the spongy scaffolds developed to keep normal liver cells happy also preserve the important properties of liver cancer for drug testing. This allows patients to choose the best treatment based on the drug testing results on their own liver cancer cells.”
Dr Toh echoed these words. “Having a reliable platform to grow liver cancer patient-derived cells is a major step in personalized medicine as we can now use them for increased throughput drug sensitivity testing,” he said.
Commenting on the clinical impact of the team’s work, Associate Professor Dan Yock Young, Head, Department of Medicine at the Yong Loo Lin School of Medicine and the National University Hospital said, “Liver cancer is the second most lethal cancer in the world with few chemotherapy options. This is in part due to our inability to customise effective therapy for individual cancers. The ability to grow cancer cells in vitro gives us the ability to conduct high-throughput drug testing to validate drug efficacy before they are used on patients. This is a key step in guiding the use of effective chemotherapy and minimising treatment futility.”
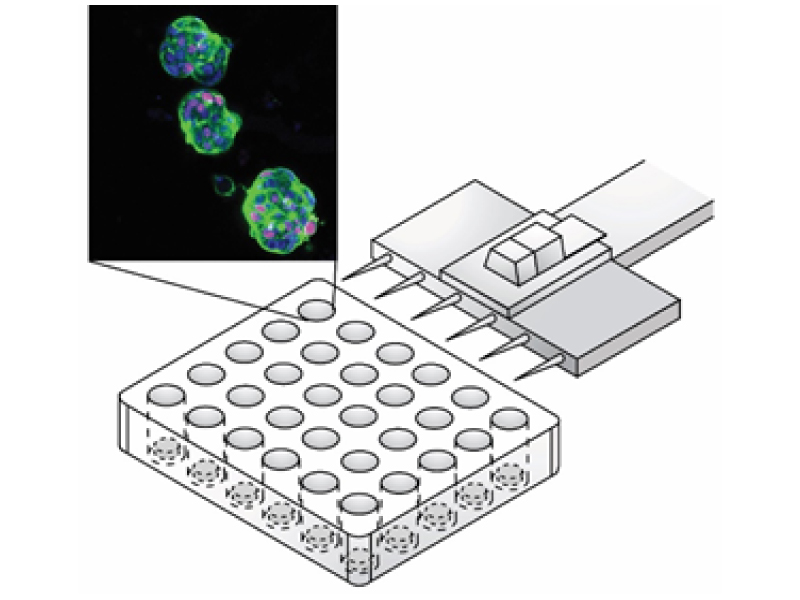
Liver cancer organoids amenable for personalised drug testing.
References
1. World Health Organization. GLOBOCAN Fact Sheets: Liver Cancer – Estimated Incidence, Mortality and Prevalence Worldwide in 2012. http://globocan.iarc.fr/old/FactSheets/cancers/liver-new.asp. Updated 2015. Accessed March 14, 2018.
2. American Cancer Society. Treating Liver Cancer. https://www. cancer.org/cancer/liver-cancer/treating.html. Updated 2018. Accessed March 14, 2018.
