Technology’s Role in Training Safer Doctors
Learning in clinical medicine has evolved over the past century and in leaps and bounds in the past two decades in congruence with advancements in information technology. Gone are those days of experimentation in caring for patients, with the practice largely guided by the dictum, ‘see one, do one, teach one’. We have come a long way from there and medical practice is well-established through the structured research, publishing and sharing of lessons learnt.
The art of medicine has evolved from bringing the students from the bench to the bedside through initiatives by pioneers of clinical medicine like William Osler. In Singapore, clinical medicine was taught and learnt through ‘cognitive apprenticeship’ and ‘student internship programs’ as early as the 1960s. Learning was opportunistic, limited to the range of clinical case exposure, availability and interest of faculty and clinical context. This brought in issues with poor generalisability and inadequate preparedness when diseases, people and cultures met, facilitated and hastened by the speed, convenience and ease of global air travel. Information and medical knowledge need to be shared in a time-efficient and succinct way. Students who lack sufficient contact time with patients do not gather adequate core clinical knowledge and skills and this may place them and their patients in dangerous situations.
From basic skills training
The introduction of computers in education in the late 1980s and the advent of the internet revolutionised technology-enabled learning (TEL) and addressed the majority of these lacunae in medical education by facilitating accessibility and increasing options for review of core content. In the basic science years, the educational content is now regrouped into modular themes: for instance, the cardiovascular system includes basic anatomy, functional physiology, relevant pathology and the pharmacology of medications. These foundational aspects are identified as core concepts and tagged into web based repositories for the clinical years, providing students who interact with patients with a systems-based approach
after they have revised the relevant applied basic medical literature. To offset the lack of time and opportunity for students to practice basic skills like history and structured examinations, learning in early years in medicine now features history taking sessions with standardised patients, who are trained volunteers that are able to provide structured feedback to learners. Web-based virtual patient platforms are now in vogue. These feature patient profiles, with options to trigger the appropriate history, emotions and clinical information pertinent to the case chosen and in response to learners’ decisions and actions. These offer offline learning with personalised feedback, where students practice adequately in their own time to achieve a level of expertise that would deem them fit to meet patients in the clinical years.
To immersive, acute scenarios that test and hone clinical skills
While to ‘err is human’, it is fatal in the context of caring for the acutely ill. Learning the science of acute care requires the right knowledge, dynamic decision making, initiating timely interventions and a stoic frame of mind. Necessary skills can now be developed through part-task trainers such as the airway trainer, CPR, cannulations and procedural trainers. These allow ‘deliberate adequate practice’ to provide the level of skills and confidence enabling learners to focus on clinical data interpretation, critical thinking and decision-making. Not all learners develop the necessary skills and acquire applied core knowledge in conventional didactic teaching sessions. Hence, the need for better platforms featuring a safe learning environment that would benefit the learner and eventually, the patient.
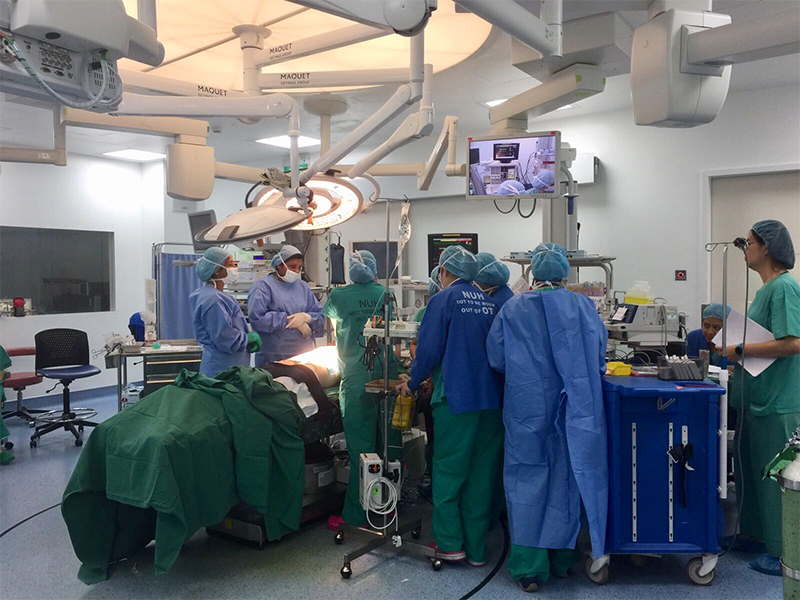
The introduction of high-technology, full-scale simulations have enhanced team-based participatory learning in acute care with near-real pathophysiological transitions and interventions, such as needle decompressions and surgical airway access. These have enabled learners to feel empowered to deploy these skills in safe reproducible ways without any patient harm and facilitate higher-order learning, such as demonstrations in a congenial atmosphere of peer-assisted learning with structured formative feedback.

Simulation training helps save lives
There is now evidence to show that introduction of simulation-based structured teaching programmes has enhanced the safety of clinical procedures, resulting in fewer complications. Technology-enabled learning however does not adequately address the bewilderment and helplessness that newly graduated healthcare professionals grapple with when they are thrown into the turbulent ocean of clinical medicine, with the need to make prompt, on-the-ground decisions independently while they acclimatise themselves to concepts of working with fellow nursing and allied health care teams. All these, as they also seek to understand and navigate hierarchical structures as newbie house officers.
Hospital sentinel event data has consistently shown that preventable errors are chiefly in the category of ‘delayed recognition and absence of early escalation’ of deteriorating situations. While high-technology manikin-based simulations prepared them reasonably well in team decision-making, interns and junior doctors are discovering that they need to make independent decisions in most instances. In response, virtual simulation offers training scenarios on a range of interactive platforms.
Such simulation can be computer/tablet-based, with two or three-dimensional scenarios offering positive feedback incentives and ‘punishment’ for mishaps or losses and missed cues. App or game-based scenarios have revolutionised the learning of basic and applied clinical concepts in an amazingly engaging and interactive way.
With the learners being digital natives, simulation and education have embraced wearable technology such as virtual reality (VR) where the learners enter an imaginary scenario through an ‘avatar’ and perform appropriate calibrated tasks with inbuilt feedback upon completion.
The promise of augmented reality (AR) is in overlaying advanced basic and clinical situations onto learners’ own clinical environments with a blend of virtual and high-technology simulations.
The AR and VR platforms could be a promise of the future in which learners independently participate in clinical scenarios and repeat these exercise in their own time, to practice their decision-making skills to the level of expected standards, thereby developing ‘cognitive dexterity’ or the ability to think and act smart when exposed to grave situations with rapid pattern recognition skills. Preparing them to handle such states ‘offline’, we hope, would help young doctors to practice safely.
It is imperative that we understand the needs of our learners, choose the appropriate platforms for the right content, provide the optimal exposure and adequate time on task and finally, give structured timely constructive feedback so that they are current and well-equipped to be better practitioners of compassionate, state-of-the art healthcare.
