The Future of Singapore Healthcare

Associate Professor Benjamin Ong, Director of Medical Services, Ministry of Health, delivered the NUS Medicine Keynote Address to students and staff of the NUS Yong Loo Lin School of Medicine, Duke-NUS Medical School and Lee Kong Chian School of Medicine on September 9.
This is an exciting and challenging time to be part of the Singapore healthcare system. I am encouraged to see so many of you here with the desire to serve our nation in healthcare into the future.
The Changing Healthcare Landscape in Singapore – Setting the Context
You are about to enter the Singapore healthcare system as a healthcare professional at a crucial time. Many of you will look back at this time as an inflexion point as the landscape of our healthcare system is changing rapidly, and upon graduation you will be at the forefront of these changes. Our healthcare sector has been lauded as probably amongst the best globally. One such measure is our life expectancy which stands at 82.8 years on average now, making it among the highest in the world. We expect this to increase further. But we have another leading statistic – the percentage of our population aged 65 and above is expected to double to 20% by 2030. That means one in every five of you in this auditorium.
This is not a new phenomenon. Developed countries all over the world are ageing. What makes the situation here slightly more acute is our low fertility rate. According to the World Bank, Singapore’s Total Fertility Rate in 2014 is 1.25, making it 196 out of the 200 countries ranked. Here we are near the bottom of the table!
But I want us to realise what an increased lifespan implies. It means that more Singaporeans will be living longer with chronic conditions. For example, the number of persons aged 65 and above with dementia is projected to more than double from about 20,000 today, to more than 50,000 in 2020. The ageing population will increase the healthcare needs of the nation significantly, and we have to be prepared well in advance to meet these needs.
What all these numbers are trying to impress upon us is that there will be increasing burden on the working population to support the elderly.
Healthcare 2020 – Addressing Capacity and Affordability
Our existing healthcare system was built to serve the population needs of the past. Our acute hospitals have, for a long time, been rightly the centrepiece of care delivery, and served the more acute, episodic healthcare needs of a younger population well. This model also guided our manpower planning and our health professional training. However, the system is increasingly strained in the current context as this configuration is hard put to deal with an increasing proportion of patients not amenable to a single curative intervention.
One of the main thrusts of the Healthcare 2020 Masterplan is to increase overall healthcare capacity. But, while we are still building more acute hospitals, we also broadened our capacity to increase community hospitals, nursing homes and other healthcare facilities to meet the changing demands. Just to list a few examples, Ng Teng Fong General Hospital, Jurong Community Hospital and Yishun Community Hospital were opened last year. By 2020, there will be an additional 6,600 places in community care, home care, and palliative care sectors. Marine Parade Polyclinic has just been expanded and further plans for the primary care sector are in the pipeline to 2020 as part of our initiatives to strengthen community care.
On manpower, the residency programme was started in 2010 in part to introduce training structure, reliability and efficiency in specialist training. There are now more doctors entering specialty and Family Medicine training. The number of medical students in our three medical schools has also increased over the years. Nonetheless, the training of healthcare professionals takes years and more so for specialists, who may require more than a decade to train. This makes it inherently challenging to calibrate the training pipeline and constantly maintain an appropriate number of healthcare workers in the system. Occasionally, we have needed healthcare professionals from overseas to augment our teams.
The Ministry has been taking steps to further improve the quality of healthcare delivery. To ensure that we do not sacrifice quality for quantity, the Ministry is reviewing the training of our healthcare professionals, taking into consideration the current practice and learning environment. For local specialist training specifically, residency has provided a framework to anchor our training even though there are areas that need improvement. The first batch of residents has just completed training. We will continue to monitor and improve the system. For healthcare professionals from abroad, the professional boards and councils have put in place supervisory frameworks to ensure that they can practice safely and competently here.
The Ministry has also been implementing the recommendations of the Nursing Taskforce since 2012 to strengthen the development of the nursing profession in the areas of Career progression, Autonomy, Recognition and Education. Some of these initiatives include providing bridging courses for our Enrolled Nurses to become Registered Nurses and the nurturing of more Advanced Practice Nurses.
The third focus of Healthcare 2020 is affordability. Apart from the Community Health Assist Scheme (CHAS) and the Pioneer Generation Package, MOH launched the MediShield Life in November last year. MediShield Life provides better protection and higher payouts, so that patients pay less Medisave/cash for large hospital bills; it covers all Singapore Citizens and Permanent Residents, including the very old and those who have pre-existing conditions; and it is protection for life.
Beyond Healthcare 2020 – Ensuring Effective Sustainability
However, to truly prepare ourselves for the change in the healthcare needs, we have to put the patients back at the centre of healthcare delivery and better appreciate how they journey through their stages of health and illness, and across different care settings. Optimising these care journeys requires us to develop a system perspective and not, myopically, a single care setting focus. We will have to go upstream to focus on resource utilisation, disease prevention, and home and community care. All these have to be done in a sustainable way, bearing in mind the constraints on resources we will increasingly face in the future. These are encapsulated in the Beyond Healthcare 2020 plan as “from hospital to community”, “from quality to value” and “from healthcare to health”.
From Hospital to Community
The transition from a traditional hospital-centric model to a broader community-based one will require building stronger links between tertiary institutions and the primary, intermediate, long-term and home care sectors, to better deliver care to Singaporeans. Much has been said about the Regional Health Systems (RHS). Each RHS will have oversight of the acute hospital, community hospitals, nursing homes, polyclinics and home care providers under its purview, ensuring that patient flow is seamless and care is coordinated. This can be done in many ways, one of which is integrated care pathways. Private primary care providers like the GPs should also come under this framework for the benefit of their patients.
Primary care is the foundation of any healthcare system. We are strengthening its place in our healthcare system as the first and continuous line of care. Our goal is to realise the vision of “One Singaporean, One Family Doctor”. Our Family Physicians and general practitioners, and not the specialists, should be the first point of contact for most Singaporeans, both the ill and well.
Healthcare Manpower
As we reshape our health delivery system, we will have to re-look the whole care process ecosystem and reduce duplicative and unproductive clinic visits and tasks as well as tests. However, there is also a need to modify the way we train our healthcare workforce. First, we need to re-balance the tide of sub-specialisation and bring back generalist skills to reduce care fragmentation. Too many times, we hear of patients with multiple specialist appointments in different places, a long shopping list of medications that seems to grow with every appointment, and no one doctor to take overall responsibility. A diabetic patient with stable cardiac and neurological complications does not need to be separately seen by the endocrinologist, cardiologist and neurologist. Siloed, episodic models of care will become increasingly unsustainable as life expectancy becomes longer and more Singaporeans live with multiple chronic conditions. This is where generalist disciplines such as Internal Medicine, Family Medicine and Geriatric Medicine come in. Doctors in these areas are overall in-charge and coordinate the care for patients with multiple co-morbidities. Unfortunately, these are not as popular among doctors as we would like them to be.
To further strengthen primary care, MOH has introduced training subsidies to encourage our primary care colleagues to undergo postgraduate training in
Family Medicine for continued upskilling. As the prevalence of chronic diseases and complexity of cases increase, with more people having multiple co-morbidities, the MBBS alone may become insufficient for independent professional practice. These efforts will take time but I hope with this, the public can slowly appreciate the professional value-add that Family Physicians can bring to their care.
This generalist approach applies not only to doctors but also the nurses and pharmacists. As we train more Advance Practice Nurses (APNs) who can specialise in areas such as critical care and psychiatry, all nurses should still be able to provide good basic nursing care. Similarly for the pharmacists, though the numbers are much smaller than the APNs, specialist pharmacists should still be able to, if I may quote from the Department of Pharmacy’s website, “tackle challenging human health problems” and maintain “clinical acumen and scientific mastery that translate to applications in clinical practice, pharmaceutical research and service”.
Here, I should make a special mention about our medical social workers (MSWs). You are an integral and important part of the healthcare team and I say this from personal experience. Singapore may be affluent but changing family structures possibly mean more elderly living alone and with their co-morbidities. This is where our MSWs will become more important. You bridge patient care across sectors and it is not just from the acute hospitals to step down care but also within the community. As we mourn the passing of Mr S. R. Nathan, take pride in the achievements he has accomplished, academically and professionally, in the area of medical social work and build on it, exemplify it.
Demand for healthcare will continue to grow with an ageing population and the supply of local manpower will shrink due to falling birth cohort sizes. As such, innovation and productivity must increase to take on the challenge ahead. Productivity and efficiency efforts by healthcare workers are for a noble purpose,
as they enable us to serve patients and residents better. Each of us can lead in this effort, by reviewing workflow and eliminating waste, deploying equipment and technology that extend manpower, expanding our skills with training to meet changing care needs and empowering patients, caregivers, volunteers to support the care delivery. At the systems level, we are reviewing policies and regulations and are prepared to change if they no longer serve their intended purpose. We are also designing for efficiency and automation upfront when planning new healthcare facilities. There have been many good ideas that have been implemented and we must continue to strive to create ways to do more with less manpower.
From Quality to Value
I mentioned ensuring sustainability in the face of re-modelling our healthcare delivery. With so many new drugs and medical devices coming out of the market, what is the most appropriate for our patients and that is sustainable for the healthcare system? The Ministry has recently set up the Agency for Care Effectiveness to (1) guide the proper use of such treatments and technology, and (2) encourage providers to manage costs while providing quality care.
From Healthcare to Health
While I have been expounding on what we are doing to provide care for the ill, we need to remove the causes of ill-health early and reduce the progression of long-term chronic diseases. This is a challenging task for it not only involves our colleagues in the Health Promotion Board, everybody from outside the healthcare sector must be engaged. A mindset change, to move away from the current lifestyle, must be embraced.
The World Health Organization recently announced that the global number of adults living with diabetes is over 400 million in 2014. Of these 400 million, 400,000 are in Singapore. The Minister for Health has
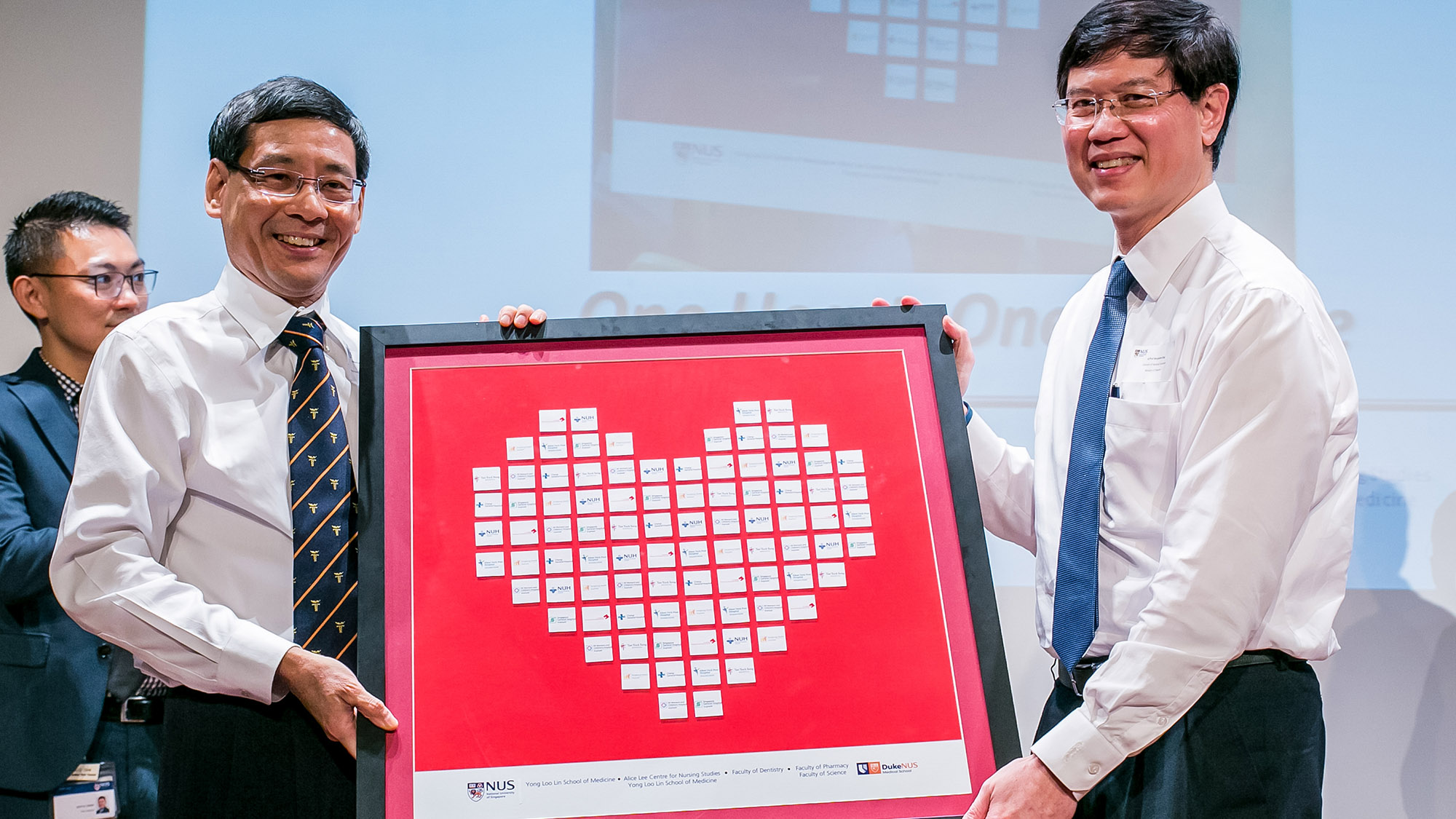
Assoc Prof Benjamin Ong receiving a token of appreciation from Dean of NUS Medicine, Assoc Prof Yeoh Khay Guan at the Keynote Address
therefore recently declared War on Diabetes. You are certainly aware of the many risk factors and complications related to this one single condition. Tackling diabetes will have collateral benefits on the prevention and management of other chronic conditions such as diseases of the heart, nerves, and kidneys. However, rather than a campaign against one specific disease, may I urge you to see this as an anchor upon which the entire healthcare sector – health promotion, primary care, acute care and rehabilitation need to come together to reduce the rate of increase in diabetes, and support and empower patients with diabetes to manage their condition well. This is going to require the sustained efforts of everyone here.
Expect the Unexpected – Infectious Diseases
Singapore is a global travel hub, with about 60 million travellers passing through Changi Airport last year. Some of these travellers may bring with them communicable diseases. SARS was brought into Singapore through air travel. Zika may also have come in from the region in the same manner. We are preparing for the importation of MERS. Thailand, Malaysia and the Philippines have already experienced imported MERS cases. A single imported case can result in a huge outbreak and national crisis as we saw in South Korea last year. We also have to contend with endemic diseases such as tuberculosis, HIV and dengue. The principle is simple: prevent or stop outbreaks through early detection and disruption of the chain of transmission. Even as we strengthen our national surveillance systems, the Zika outbreak has illustrated to us the importance of vigilant healthcare workers – to pick up the unusual. Early detection of SARS, chikungunya and Zika was all effected through such vigilance. If we are able to detect an outbreak early, we would have a better chance of minimising its impact.
Your Role
I have highlighted the main areas which we have identified as high priority for Ministry development, such as primary care, intermediate and long-term care and public health. I also covered infectious diseases and the response that needs epidemiologists, infectious diseases physicians and public health experts. I encourage you to consider careers in these sectors in future. Not only will you be moving Singapore healthcare forward, you will also find yourselves genuinely fulfilled as you touch the lives of everyday Singaporeans.
We will need skilled healthcare professions to lead the charge in the community. Patient care will be more complex and challenging. It is therefore even more important that you see yourselves as part of one public healthcare system. The relationships that you build in school now will allow you to have a shared goal and camaraderie. More importantly, the relationship you build with your patients will enrich your professional lives ahead.
Conclusion
All systems must evolve and adapt to changes. Changes present opportunities for us to grab. I very much hope you will all embrace this time of change and lend your talent to the healthcare system to ensure Better Health, Better Care and a Better Life for all Singaporeans.
