Uncovering Bacteria’s Achilles Heel

Over the last two decades, there has been a dramatic worldwide increase in the prevalence of type 2 diabetes, including in the Asia-Pacific region. Associate Professor Gan Yunn Hwen from the Department of Biochemistry looks into how bacteria evade the host immune system and establish infections, and why people with type 2 diabetes are more susceptible to disease than healthy people.
A bacterial pathogen that A/Prof Gan has worked on extensively is Burkholderia pseudomallei, which is endemic in Southeast Asia and northern Australia. Infection with the bacterium causes melioidosis, a disease with wide-ranging symptoms, such as severe pulmonary distress, that may progress to septicaemia and death if untreated. B. pseudomallei can also cause chronic infections and remain latent for many years without causing symptoms.
A/Prof Gan and her research team are trying to understand how B. pseudomallei causes disease. Their research has shown that two secretory systems in B. pseudomallei, the Type III (T3SS) and the Type VI Secretion Systems (T6SS), play an important role in disease. Bacteria with mutated T3SS or T6SS do not cause disease. T6SS mutants also fail to induce host cells to fuse, a feature of their non-mutated counterparts. The team is now investigating how the bacteria trigger cell fusion and why this is important for causing disease.
To further understand how bacteria circumvent the host immune response, A/Prof Gan is studying infections with the K1 and K2 serotypes of Klebsiella pneumoniae bacteria. These pathogens can cause liver abscesses, especially in people with diabetes in China, Hong Kong, Taiwan, Korea, and Singapore. A possible explanation for the increased susceptibility of type 2 diabetics to such infections is the decreased ratio of reduced glutathione to oxidized glutathione in poorly-controlled diabetes. This redox environment appears to suppress the killing of bacteria that have been phagocytosed by macrophages (see Facts Box). Its effect on other immune responses, such as the antimicrobial activity of neutrophils, remains to be determined. A/Prof Gan, together with Assistant Professor Sophia Archuleta and Professor Lee Kok Onn from the Department of Medicine, were recently awarded an Aspiration Fund grant to study such mechanisms of immune susceptibility in type 2 diabetes.
Today, a major challenge in controlling bacterial infections is the emergence of multidrug-resistant (MDR) or extensive drug-resistant (XDR) bacterial strains. Another focus of A/Prof Gan’s research is Acinetobacter baumanii, an increasingly drug-resistant bacterium that is responsible for a rising number of infections in Singaporean hospitals. Infections can be either hospital-acquired or community-acquired (acquired outside the hospital and long-term care facilities). With the help of seed funding from the National University Health System, A/Prof Gan is currently collaborating with other researchers to develop immunotherapies for these drug-resistant pathogens.
Facts
Effect of Glutathione Ratio (GSH/GSSG) on Immune Response in Type 2 Diabetes
- Decreased glutathione ratio in type 2 diabetes causes decreased IL-12 production.
- Decreased IL-12 production in turn causes reduced IFN-γ production by immune cells.
- Less IFN-γ leads to poorer killing by macrophages of Burkholderia pseudomallei and Mycobacterium tuberculosis bacteria.
- Need to determine whether the reduced ratio also suppresses other types of immune responses to Klebsiella pneumoniae in type 2 diabetes.
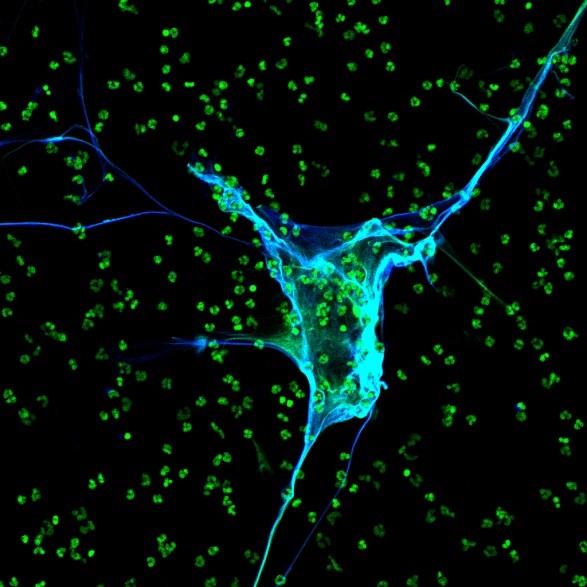
A neutrophil forming neutrophil extracellular traps (NETS) that bind Klebsiella pneumoniae bacteria (bacterial DNA stained green) and release substances such as neutrophil elastase (stained blue) that kill the bacteria.
