Issue 49
Feb 2024
SCIENCE OF LIFE
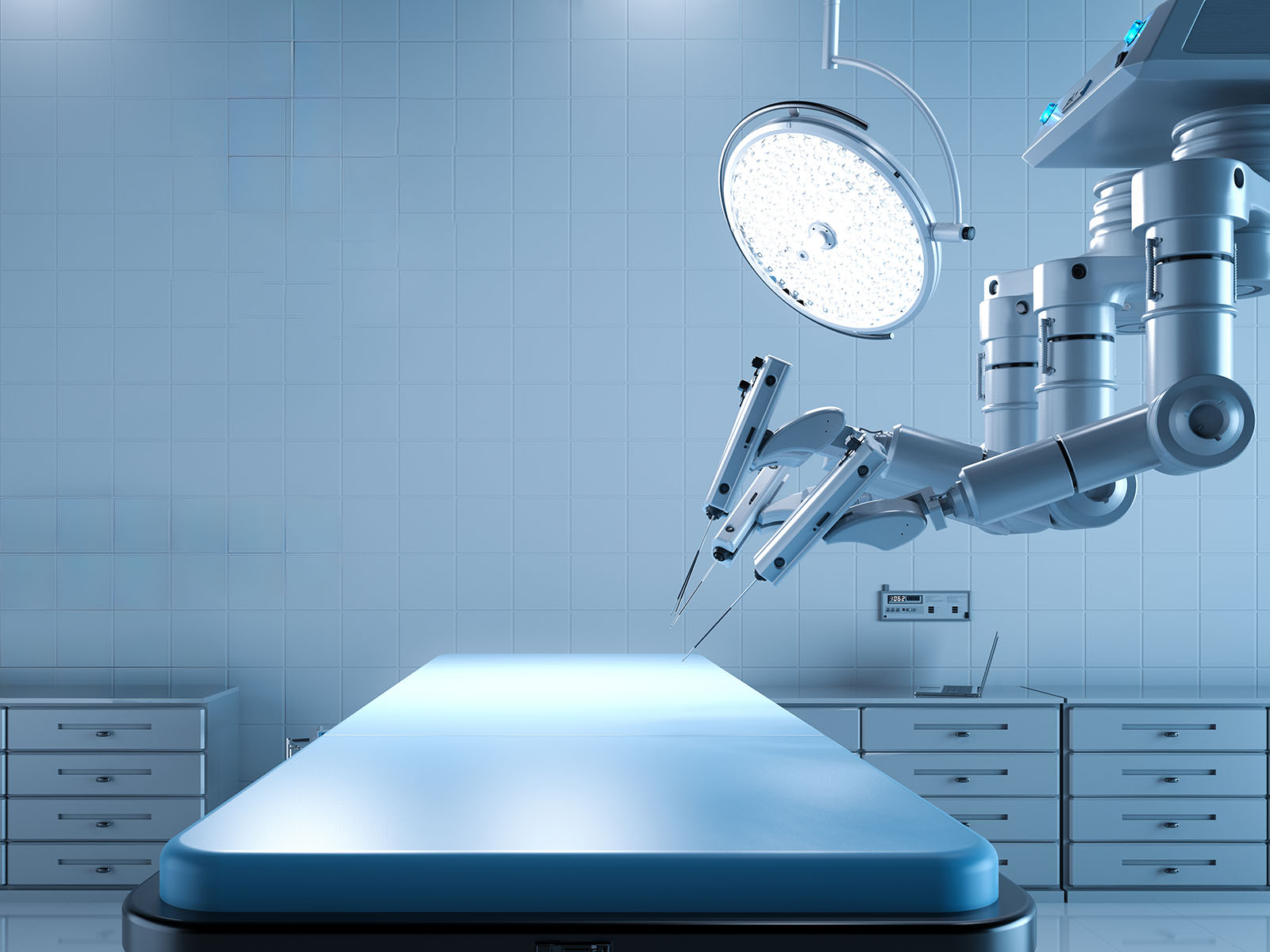
In an extraordinary fusion of technology and medical expertise, clinician-scientists from Singapore and Japan embarked on an exciting new collaboration—robotic telesurgery, aided by recent developments in advanced surgical robots and network telecommunication technology.
Picture this: in a sterile operating room in Nagoya, Japan, robotic arms move with astonishing precision as they prepare to perform a complex laparoscopic surgical procedure.
What makes this scenario truly remarkable is the surprise twist—it’s not the surgical team in Nagoya controlling these robotic arms. Instead, they are being orchestrated by surgeons located over 5,000km away in the Advanced Surgery Training Centre at Singapore’s National University Hospital (NUH), the teaching hospital of the Yong Loo Lin School of Medicine, National University of Singapore (NUS Medicine).
NUS Medicine and NUH collaborated with Fujita Health University (FHU) in its first robotic telesurgery trial between Singapore and Japan, from 9 to 11 October 2023. Leveraging Japan’s first surgical robot, clinician-scientists from NUH and NUS Medicine remotely performed a gastrectomy (stomach surgery performed for cancer) on a simulated organ from a surgeon cockpit in Singapore. The surgeons’ movements were transmitted, directed, and replicated by a robotic operation unit located in Japan via a dedicated international fiber-optic network.
This collaboration follows the Memorandum of Understanding (MOU) signed in August 2023 between NUS Medicine and FHU, one of Japan’s leading universities with a strong research focus in robotic surgery and telesurgery. The MOU aims to deepen academic partnership through active joint collaborations, including the execution of remote surgical experiments, and promote mutual exchange activities such as student exchange programmes.
Remote telesurgery offers immense potential to enhance global access to specialised care, reduce travel and wait times for patients, minimise health risks during emergencies and pandemics, and foster training and collaboration among medical professionals worldwide. It also contributes to improved surgical expertise for complex cases, particularly benefitting underserved areas.”
Harnessing the potential of telesurgery
The two gastric surgeons leading the demonstration in Singapore are Professor Jimmy So from the Department of Surgery, NUS Medicine, and Senior Consultant in the Department of Surgery, NUH, as well as Assistant Professor Kim Guowei from the Department of Surgery, NUS Medicine, and Consultant in the Department of Surgery at the NUH.
In Japan, the surgical team is led by Professor Ichiro Uyama and Professor Koichi Suda from FHU.
The preclinical trial—involving a series of complex gastrectomy procedures conducted by both teams—aims to prove that long-distance robotic telesurgery for technically demanding procedures can be safely conducted using a robotic system connected by high-speed fiber-optic communication.
While robotic surgery is not new in Singapore, this collaboration between NUS Medicine, NUH and FHU marks a critical step towards making remote surgeries an accessible option to patients in the near future.

(From left) Prof Koichi Suda, Prof Ichiro Uyama, Dr Kim Guowei and Prof Jimmy So (seated) are the four gastric surgeons leading the gastrectomy demonstration, a collaboration between NUS Medicine, NUH and Fujita Health University. (Photo Credit: National University Health System)
“Remote telesurgery offers immense potential to enhance global access to specialised care, reduce travel and wait times for patients, minimise health risks during emergencies and pandemics, and foster training and collaboration among medical professionals worldwide. It also contributes to improved surgical expertise for complex cases, particularly benefitting underserved areas,” said Prof Jimmy So, lead of the surgical team in Singapore.
During public health crises, such as a global pandemic, remote telesurgery helps minimise the risk of disease transmission between patients, healthcare workers, and surgical teams. Surgeons can perform surgeries from a safe location, reducing the potential for infection spread. Such forms of surgery also help promote tele-mentoring or distance learning in medical education, allowing young doctors and medical students to learn surgical techniques and skills from lecturers and medical experts based not only in a different part of Singapore, but also anywhere in the world.
Assistant Prof Kim Guowei added, “In partnering with our Japanese colleagues, we hope to advance and unlock the potential of telesurgery for patients and doctors alike. This continuous exchange of knowledge, advanced surgical techniques, and best practices across borders contributes to improving surgical expertise and outcomes.”
Click here to watch the surgery in action.
More from this issue