Mother’s Antibodies May Worsen Dengue Infection in Children
A dengue vaccine that stimulates a strong T cell response in babies has been found to provide better and broader protection than vaccines which induce the production of mainly antibodies. An NUS research team that made this finding also found that a mother’s antibodies which help to protect her babies against dengue virus infection can also be detrimental in some situations, as these maternal antibodies can enhance the severity of dengue infection in babies or interfere with their immunisation.
These discoveries were made by a team led by Associate Professor Sylvie Alonso and her team from the Department of Microbiology and Immunology at NUS Medicine. The study was published in the scientific journal JCI Insight in December 2017.
The researchers’ findings show that maternal antibodies which circulate in babies born to dengue vaccinated mothers can protect against dengue only if the infecting dengue strain is very similar to the strain that is present in the vaccine. However, maternal antibodies will not be able to protect against a dengue strain that is different from the strain used in the vaccine. And in fact, they may make the disease even worse.
In addition, the team has generated experimental evidence which indicates that maternal antibodies can interfere with the baby’s vaccination. That is when antibody production will be completely prevented (a phenomenon known as “maternal antibody interference”).
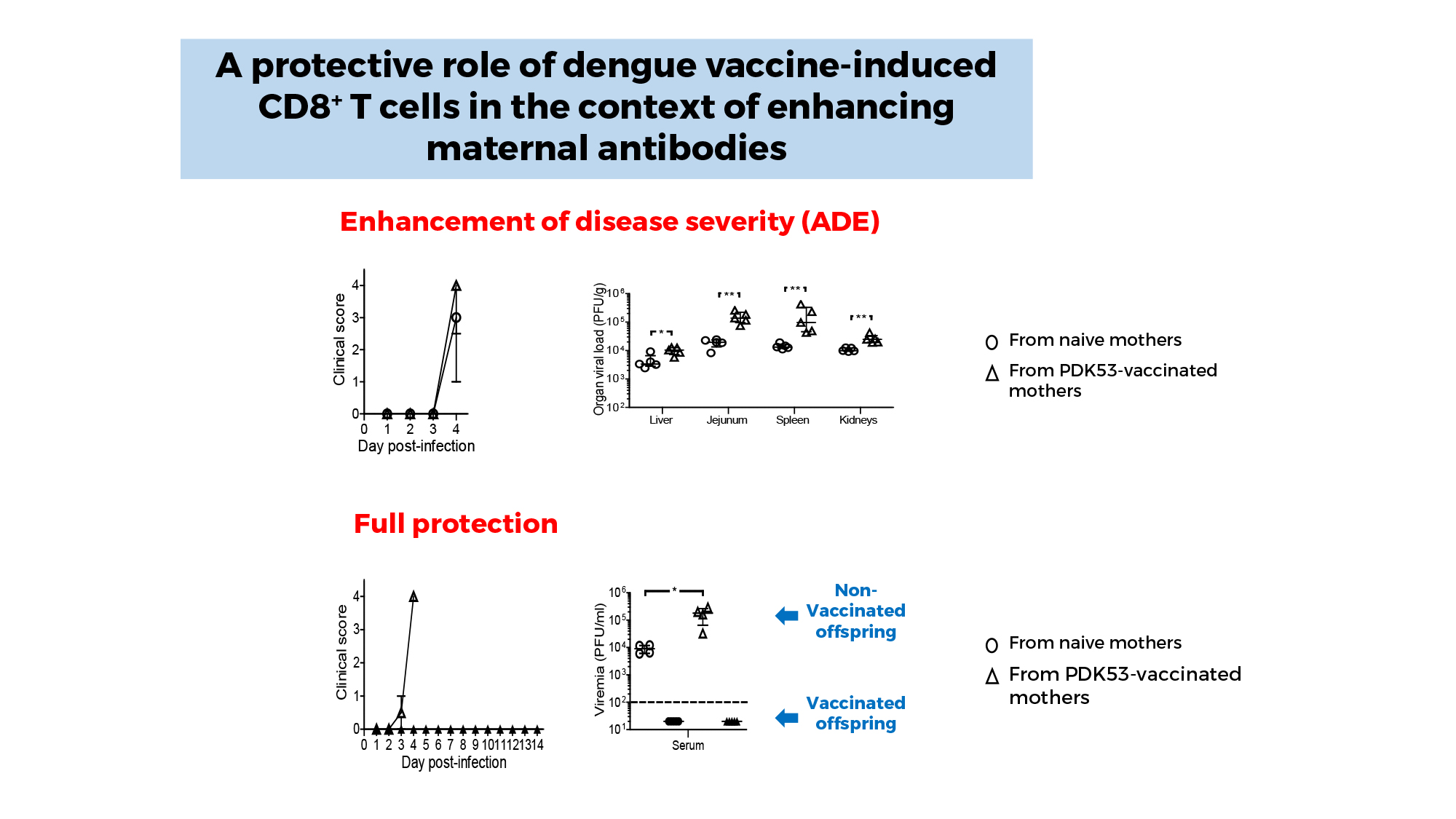
However, vaccination of babies born to dengue vaccinated mothers will still be able to induce a T cell response, the other arm of our immune system. A/Prof Alonso and her team showed that this T cell response is able to protect against dengue, even when the infecting strain is different from that used in the vaccine.
These findings therefore show that a dengue vaccine which induces an effective killer T cell response could provide better and broader protection for children born to vaccinated mothers, than vaccines which rely mainly on antibodies, such as Dengvaxia, the only dengue vaccine that is currently on the market.
The impact of these findings on vaccination strategies in humans is significant, as more children are born to mothers who have been vaccinated against dengue infection.
“We hope that our work will further convince the dengue vaccine community that it is of utmost importance to include a protective T cell response in their vaccine design. Too many efforts are currently being devoted to looking at an antibody-mediated protection
while the T-cell responses are being overlooked,” said A/Prof Alonso.
She added, “We hope that the team currently taking care of the clinical development of the DENVax candidate will measure the T cell responses in the vaccines. Lastly, we hope that our work will entice clinical trial teams to include monitoring of children born to vaccinated mothers as well as vaccination efficacy in these children.”
Commenting on the importance of these findings, Professor Paul Anantharajah Tambyah, Senior Consultant at the National University Hospital’s Division of Infectious Diseases said, “These findings are very interesting because they help us to better understand the role that the different parts of our immune system play in our response to dengue and other viral infections. They emphasise the fact that we cannot just look at one measure (for example the antibody levels) but need to comprehensively ensure that individuals who are vaccinated by any candidate vaccine are truly protected from infection. It would be unfortunate if a vaccine actually made the situation worse by triggering off one part of the immune system to over-react instead of completely eliminating the virus.”
