The Future of Medical Education
I. The Future of Medical Education
Imagine….
The year is 2026. It is 7.30am during a typical day in the life of a 1st year medical student, somewhere in the world….
“Good morning P.A.T! Tell me what my learning schedule is today….”
P.A.T. stands for Personalised Augmented Tutor and is introduced to us on the first day of medical school. Together with our tutors, P.A.T. ensures an active and seamless medical education for budding medical doctors.
“Good day TP, today you will continue to learn about the cardiovascular system….”
P.A.T. gives an overview of the learning objectives, key learning points, essential skills and knowledge which I need to acquire (eventually) and a summary of my day’s activities.
“You will start by talking to Mrs Lee in Ward 24.
She has a history of heart conditions and was recently admitted because of increasing breathlessness.”
P.A.T: “Would you like me to download your learning material?”
“Yes please…”
I spend the rest of my journey to school re-watching a short interactive video on how I can take a focus cardiac history from a patient.
Arriving at the clinical training site, I meet up with my peer group after seeing Mrs Lee in the ward. For the next two and a half hours, we review our learning materials, which is based on our interaction with our designated patients, together. Each member of the team interacts with P.A.T. which summarises key learning points for us. Based on my scores and the way I enquired and answered the questions, P.A.T. is able to accurately identify areas I need to improve upon. A detailed plan to get me up to scratch is then formulated. During the session, we also clarify our queries and doubts with each other. Throughout this period of time, we know that our tutor is on hand to answer any questions which we may have.
We spend the last half hour answering specially crafted questions together as a group. These questions generally focus on application of knowledge and answering them is a good way for us to know if we have truly grasped the essential concepts. P.A.T. again is with us and easily accessible to provide feedback on our answers. After the peer group learning session, we proceed to join the emergency medical response team as junior team members.
This experiential clinical learning is scaffolded, i.e. scaled to progress from the basics to the complex. Although I would very much like to get into the thick of the action, the focus of the formative years in medical education is to observe and learn as I gather the required knowledge and skills. After the clinical attachment, I then “prove my worth” by demonstrating my competencies in a virtually simulated environment. I can then join the medical team in “real” clinical care as a junior member to gather more experience, something I am very much looking forward to.
The rest of the day is spent on self-study and part-task training. I get to practice my central line insertion on ultra-real simulators and P.A.T. guides me along the process. Throughout the practice, I am shown relevant anatomical information which I need for this skill. I get to practise this skill in my own time and will progress to setting a CVP on a real patient when I have fulfilled the requirements as stated in an Entrustable Professional Activities (EPAs) document (administered by P.A.T.). My first insertion of CVP on a real patient will be supervised by my clinical tutor and I believe I will be able to do a good job with the kind of medical training I am receiving.
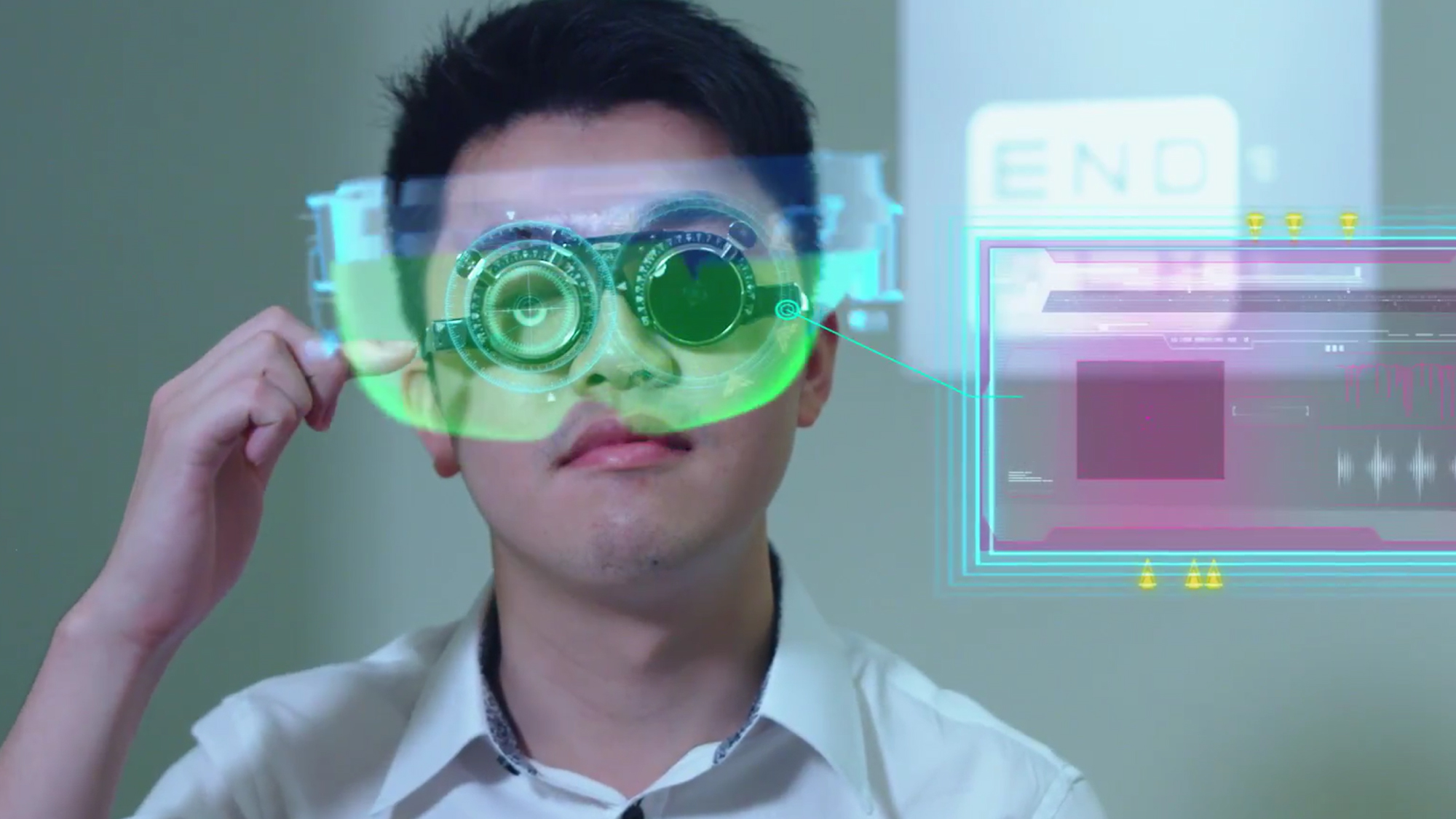
During the evening, as I am doing my self-learning, I get a call from a fellow classmate. He is intrigued by a “discovery” he made of the blood supply to the heart and is keen to show me on a 3D virtual model of the heart. Through my Augmented Reality (AR) glasses, I am able to interact with him and tilt the AR heart model to see exactly what he means, even though we are physically at different locations.
“Time to take a break, TP…” reminded P.A.T.
“It looks like you have had quite a fruitful learning day.”
“Yes, I did… please help me put a mental note on what I need to revise tomorrow. I am also going to write a short reflection before I go to bed.”
“That’s great TP. Have a good rest and we can start afresh tomorrow morning!”
II. Future Perfect
In an article published in Issue 22 of MediCine, we imagined what medicine and healthcare might look like in the not-too-distant future. In this article, we explore the medical education required to complement this future healthcare system.
1. Personalised medical education with the help of artificial intelligence
We learn differently. Each of us has our own unique way of learning and acquiring information – how we process information, retrieve prior knowledge, and adding on to them, before embedding them into our long-term memory (cognitive load theory). With the advent of technology, much of the information can be stored in “external hard drives” which may serve as repositories and extensions of our internal memory. We need the relevant triggers and links to draw out this information, which is tailored for the individual. Through the use of artificial intelligence enabled chatbots, students may have just in time learning via mixed reality portable and mobile devices.
It is now known that machines can be taught to learn. Some disciplines such as Computing and Engineering are already using ChatBots as teaching assistants. (https://mishtalk.com/2016/05/16/teachers-assistants/) and students have found it hard to distinguish a virtual tutor from a real one. In such a learning environment, students will no longer be confined to classrooms and will be active through the use of technology that assists them to visualise basic biomedical and clinical entities, while giving access to the best learning material sourced by super computers. Appropriate use of artificial intelligence will ensure that these learning materials are customised to the individual student’s level of understanding.
Faculty tutors, with the help of A.I., will be able to monitor students’ learning development closely as they interact with the material presented with increasing complexity. This would reduce the need to group students in batches as well as conduct hugely resource-intensive examinations.
These concepts align well with constructivist learning principles, where adult learners construct their own learning based on prior experience and interaction with peers and the learning environment. This is a powerful learning approach, which current “mass market” medical training will never be able to achieve effectively.
With personalised medical education, it is important to determine the key roles which define medical doctors and healthcare providers and the core competencies which are required for each role. The recent movement towards Entrustable Professional Activities (EPAs) may be a step towards this. An Entrustable Professional Activity is a set of activities which a qualified medical doctor can be entrusted to perform independently. Clear descriptions of EPAs, with the underlying required competencies, can form the backbone of future medical curriculum. EPAs can be the targets which medical students work towards and also be the assessment criteria for competencies achieved.
2. Medical school without “borders”
With the advent of the internet and the digital age bringing about unparalleled connectivity and digital repository capabilities, which are highly accessible and scalable, a medical school with no borders is a distinct possibility. With such disruptive changes to healthcare, the training of health professionals will also need to evolve and transform. The student or the resident, based on his or her individual capabilities, could transition seamlessly from one phase to the next, ensuring efficiency in time and resource. By being borderless, the learner can collaborate with peers, seniors and teachers not only in his or her locality but globally, tapping into leading edge expertise within that discipline. Already, it is possible for two learners who are physically separate, to interact purposefully with a shared learning medium. In the near future, it is very likely that surgical procedures are undertaken at a particular location, with real-time guidance (verbal and actual tactile guidance through the use of advanced robotics) provided by experts far away.
These are all disruptive changes, which will change the future design of the medical schools as well as specialty training. AI-enabled humanoid robots can help with repetitive training in a safe environment to refine physical examination techniques, procedures (especially the more invasive or painful ones) and difficult communication such as breaking bad news. This deliberate practice will help students and trainees interact effectively and gain confidence with patients at their own pace. With clear outcomes and an adaptive and personalised teaching and accreditation system, future students may truly be able to be free from time-based education and be accredited at different times relevant to their own progress.
We need to rethink how we would design health professional training programs and retrain faculty to add value to 2050 health professional education!
3. Role of Educators – Getting ready for the future
Technology will play a major role in future medical education and the adoption of technology in healthcare education needs to be by design. Faculty needs first to review the curriculum and identify current gaps and shortfalls in the current teaching and assessment. Some of these gaps may be addressed by technology adoption. When dealing with large groups of learners, appropriate use of artificial intelligence may help medical educators better tailor their efforts to individual learning, while also helping teachers to predict and identify potential at-risk students and provide necessary guidance. Digital technology may also be helpful in linking prior knowledge to current practice, explain hard-to-understand concepts through visualisation, and providing instant access to curated up-to-date resource material. A blended learning approach ensures that advantages of both face-to-face human interactive teaching and technology-enhanced learning are optimised in the complex healthcare learning. Furthermore, tutors with technological capabilities will develop new material to be uploaded and distributed amongst the learners. This group will have both the domain knowledge and specialist skills in areas such as coding, computing and big data analysis. In essence, the tutor helps the learner “deep dive” into the realms of healthcare practice.
The desire to provide quality and safe healthcare to our patients should always be at the heart of our healthcare education. As educators, we play key roles in training and shaping the younger generation of healthcare providers. This needs to be done with an open and adaptive mind, with genuine and collaborative communication, especially in the face of ever-changing technological advances in healthcare provision. Higher administration within a school also plays a crucial role in providing adequate support and resource in this transformational process. Together we will be able to continuously achieve quality and empathetic healthcare education with the appropriate and purposeful adoption of technology.
——————————————————————————————————————–
References
1. Brown, G., & Manogue, M. (2001). Refreshing lecturing:a guide for lecturers. Dundee, Scotland: AMEE
