Potency and Potential
In this final instalment of our series, we take a look at cancer vaccines.
Cancer vaccines work by activating the immune system to attack cancer cells. There are two types of vaccines – the first fights cancer that already exists, while the second type (more like the vaccines most people think about) protects against getting cancer or prevents the cancer from growing.
Therapeutic Vaccine
The first type of cancer vaccine (called therapeutic vaccines because they work against existing cancer) can take several forms. One version involves antigen-presenting cells (cells that present bits of foreign organisms to the immune system, priming it to recognise and attack these alien intruder). An example of this is sipuleucel-T
for certain types of metastatic prostate cancer; it is also the only U.S. Food and Drug Administration-approved cancer vaccine. Here at NUS Medicine, a vaccine developed by Associate Professor Herbert Schwarz, of the Department of Physiology is being tested together with Associate Professor Goh Boon Cher, Department of Haematology-Oncology, National University Cancer Institute, Singapore. This is being done through a phase I clinical trial for treatment of nasopharyngeal cancer.
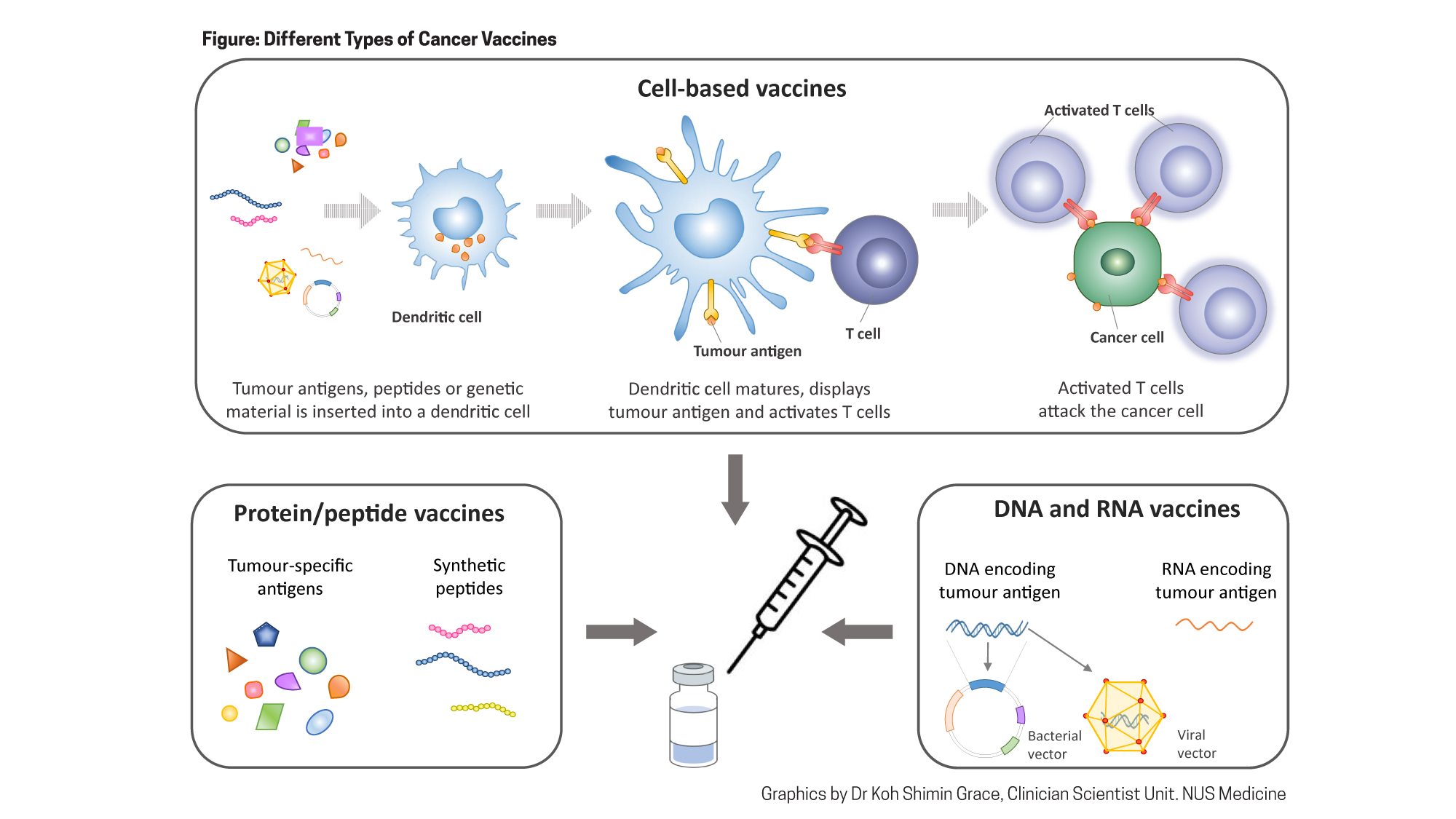
Other forms of therapeutic vaccines are at different stages of development. For example, one promising vaccine consists of an extract from the ground-up tumour, which has the advantage of containing all of the different antigens in that specific tumour. This approach works best in melanoma, which is more easily recognised by the immune system than other cancers. Another vaccine uses peptides (short pieces of proteins) that are then presented on antigen-presenting cells. A third type of vaccine in development comprises genetic material (DNA or RNA) that is taken up by cells, which are instructed to make cancer-specific antigens to stimulate an immune response.
Preventive Vaccines
The second type of cancer vaccine, preventive vaccines, involves either treating viral or bacterial infections that are known to cause cancer, or actually preventing the development of cancer itself.
Several treatments for infections are also effective at preventing cancer. For example, Gardasil prevents HPV infection and cervical cancer, HIV drugs prevent Karposi’s sarcoma, and H pylori drugs prevent gastric cancer. Preventive vaccines that act on the cancer itself are still unavailable, though the hope is that someday vaccines against cancers with very well-defined risk factors, such as BRCA1 or BRCA2 mutations that carry a high risk of breast cancer, will be added to clinical treatment options. Vaccines can also be developed that target cancer proteins normally present in childhood, but which are later lost in healthy adults, or seek out proteins found in early-stage cancer cells that are absent in normal tissue. This will train the destructive power of the immune response specifically to on to cancer cells, reducing side effects.
Unfortunately, the cost of cancer vaccines is high – four shots of sipuleucel cost $100,000. Two promising cost-saving approaches have been proposed. One involves off-the-shelf production of antigen-presenting cells, e.g. a vaccine that can be used generally for Caucasians and another for Asians. These vaccines could target antigens
Thus far, the cancer vaccines that have been developed provoke relatively few adverse effects. These tend to be relatively minor, such as reactions at the injection site and flu-like symptoms. Says Assoc Prof Schwarz, “Right now, cancer vaccines are not associated with many side effects, but that could be because they are not very effective. In future, we should see more side effects as the vaccines become more effective.”
Although serious side effects are uncommon with current cancer vaccines, one potentially fatal side effect is a cytokine storm, whereby the immune system is so strongly activated that an over-abundance of cell-activating proteins called cytokines is released, wreaking havoc in the body.
Like antibodies and cell therapy, cancer vaccines make use of the immune system to prevent and treat cancers. As more effective and affordable vaccines are developed, this type of immunotherapy will become an even more important weapon in the fight against cancer.
