Narratively Speaking
Tracing his journey in family medicine as a student and educator, Dr Cheong Pak Yean, Adjunct Associate Professor at NUS Medicine (Class of 1974) was instrumental in developing family medicine as a specialty, and shares how the discipline has evolved since its early days.
Family medicine (FM) is perhaps the earliest form of medicine practised by pioneering doctors, yet the specialisation was only officially recognised a few decades ago. Family medicine was not available as a course of study over forty years ago, when Dr Cheong Pak Yean graduated from the University of Singapore’s then Faculty of Medicine in 1974. “There was no Masters in Family Medicine back in those days. Many doctors who aspired to be leaders in the medical profession did internal medicine (IM) as it is a generalist discipline. So I did the same,” recalled Dr Cheong.

The office above Dr Cheong’s clinic today. The shophouse was built by Dr Cheong’s grandfather in the 1920s, which was occupied by the Japanese during WWII.
Plugging in the Gaps in Practice
After completing his housemanship and postgraduate studies, Dr Cheong started his clinic in 1980 in a shophouse built by his grandfather in Bukit Timah and began his practice as an internal medicine physician. Facing the challenges of practice, he saw the need for clinical assistants in hospitals and clinics to improve the healthcare delivery in Singapore. He championed Healthcare Assistants’ training to enable professional clinic and hospital assistants to bridge the gap between doctors, nurses and patients. The training was taken up by the Institute of Technical Education (ITE), and later expanded into a full-fledged national programme. He also started a drug distribution and computerisation cooperative for private practitioners.
Addressing national needs, Dr Cheong assumed leadership positions in several healthcare institutions then. He was president of the Singapore Medical Association (SMA), the College of Family Physicians and also sat on the board of the ITE and the National Healthcare Group (NHG).
Establishing a Masters Programme for Private Practitioners
Developing family medicine as a specialty became a lifetime passion for Dr Cheong. “Most specialities focus on depth, but family medicine is a generalist discipline that requires a breadth of knowledge and practice. It does not matter where you are — whether in community hospitals, nursing homes, hospice care, or polyclinics — family medicine sees to the preventive, personalised, comprehensive and continuing care of the whole patient.”
When the Masters of Medicine (Family Medicine) course was first introduced in 1990, the programme was largely administered by the Ministry of Health (MOH), and doctors were attached to various government hospitals and polyclinics as part of its curriculum. The fraternity realised that there was a large demand coming from existing private general practitioners who were serving the community. Together with Associate Professor Goh Lee Gan and Dr Julian Lim, he developed the Private Practitioners’ Stream (PPS) of the Masters of Medicine (Family Medicine) in 1994. Part-time courses were conducted in the office above his clinic, and the first candidate in the programme graduated in 1995.
Subsequently, the office was officially established as the Graduate Family Medicine Centre in 1998, and its training was accepted by the College of Family Physicians and the University of Singapore as pre-requisites for taking the MMed (FM) examination. Assoc Prof Goh, Dr Matthew Ng and Dr Cheong then went on to develop the Graduate Diploma in Family Medicine (GDFM) in 2000 as the Masters training was found to be onerous. Today, the GDFM programme has expanded to take in more than 200 doctors a year and is an entry prerequisite for the Family Physicians Register.
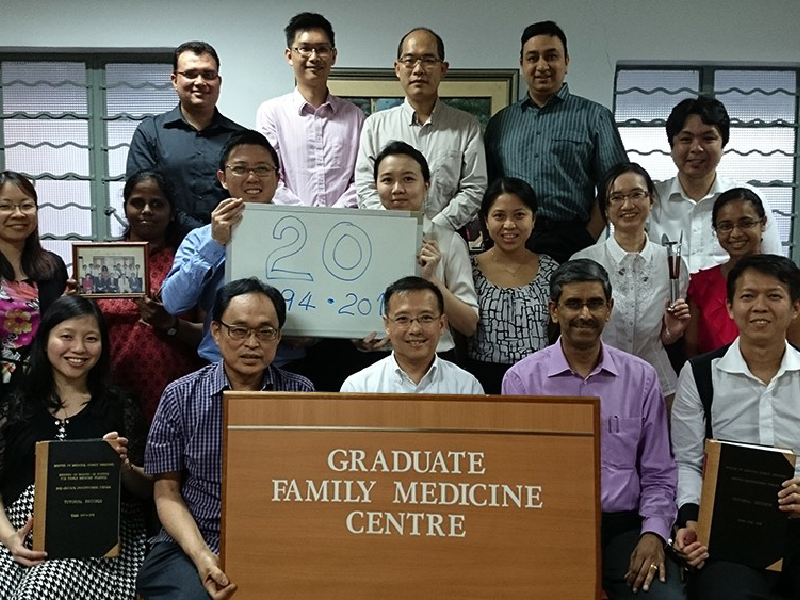
Dr Cheong with a group of postgraduate doctors at the office above Cheong Medical Clinic in 2014, commemorating 20 years since the centre was established.

Guests at the official opening of the Graduate Family Medicine Centre on 9 October 1998, a training centre recognised by the College of Family Physicians and the National University of Singapore post-graduate school in family medicine.
Teaching Humanism with Narratives
Dr Cheong was appointed Adjunct Associate Professor at NUS Medicine in 2000. To enhance his own knowledge and teaching of the humanistic dimension of medicine, he read a Masters in Psychotherapy, an area in line with his interest in medical communication. Dr Cheong fervently relates to a particular note in an MOH publication Outcome and Standards in Undergraduate Medical Education in Singapore, which highlights that, ‘As an overarching goal, medical education must seek to equip every graduate with all the requisite knowledge, technical skills, behavioural and communication skills (verbal, written and body language), empathy, compassion and professionalism in order to provide holistic, patient-centred care.’
In a series of his teaching workshops, Dr Cheong gets medical students to recall the most memorable clinical experience during their posting in family medicine, and express their reflection through drawings. He found their drawings insightful, despite studies that showed the level of apathy in students increases when they reach their third year of studies.
“Many people like to talk about evidencebased medicine when it comes to diagnosis. But I find that it may not be enough; we need to relate to the person in front of us. Are humanistic values teachable?” asked Dr Cheong.
He used these student drawings for reflective sessions with experienced family doctors, who then wrote corresponding personal vignettes and commentaries based on the illustrations. These personal, reflective drawings and narratives were compiled into a book, Being Human, Stories from Family Medicine, which he co-edited with Dr Ong Chooi Peng and published recently.
In one of the stories, titled ‘Doing Good and (not) Harm’, Dr Cheong reflected on the passing of his mother, and a situation that he came across in a hospital attachment. They depict how respecting the patient’s and family members’ wishes, and putting oneself in the patients’ shoes are forms of empathy. Should a doctor or tutor continue to teach at the bedside when a patient is agitated and hurling expletives? Could he have taught empathy and compassion by calming the patient?
Through this book, Dr Cheong hopes to cultivate the illness narrative as an experiential learning tool to teach compassion and other values to both medical students and doctors.
Read extracts of “Being Human, Stories from Family Medicine” here.