Trainee doctor clinics after 24-hour shifts: Effects on patient satisfaction and prescription errors
Submitted: 17 October 2020
Accepted: 12 April 2021
Published online: 5 October, TAPS 2021, 6(4), 26-36
https://doi.org/10.29060/TAPS.2021-6-4/OA2420
Chee Yang Chin1, Si Qi Tan2, Swee Leng Kui1,2, Kurugulasigamoney Gunasegaran1 & Jill Cheng Sim Lee3
1Department of Cardiovascular Medicine, National Heart Centre Singapore, Singapore; 2Ministry of Health Holdings, Singapore; 3Department of Obstetrics and Gynaecology, KK Women’s and Children’s Hospital, Singapore
Abstract
Introduction: Sleep deprivation impacts clinical performance. However, literature is conflicting, with insufficient focus on patient outcomes. The aim of this study was to assess if patient satisfaction and prescription errors in outpatient clinics were adversely affected when consulting post-call versus non-post-call registrars.
Methods: This prospective, quantitative study was set in a large teaching hospital in Singapore. Between November 2015 and February 2016, patients from clinics run by a registrar after 24-hour shift were recruited to post-call group. Patients from non-post-call clinics run by the same registrar were controls. Outcome measures were patient satisfaction, using 5-item 4-point Likert scale questionnaire, and prescribing error rate, defined as number of errors over number of orders. Differences were analysed using chi-squared test.
Results: 103 of 106 (97%) patients in 9 post-call clinics and 93 of 105 (90%) patients in 9 non-post-call clinics were recruited. Questionnaire completion rate was 99%. 536 and 526 prescriptions were ordered in post-call and non-post-call groups, respectively. Percentage of top-box responses (greatest satisfaction) was higher in post-call group overall (79.3% versus 62.4%, p<0.001), and for each questionnaire item. There was no significant difference in prescribing errors (1.31% versus 2.28%, p=0.23).
Conclusion: Patient satisfaction and prescribing error rates in outpatient clinics were not detrimentally affected. This provides some objective evidence that patients may safely consult post-call registrars. True impacts of sleep deprivation remain poorly understood, and larger, longer term, multicentre studies would inform generalisability. Qualitative studies of fatigue may shed light on complex interactions of emotions that compensate for tiredness.
Practice Highlights
- Studies of sleep deprivation and work-hour restrictions are conflicting, with few on patient outcome.
- We compared patient satisfaction and prescribing errors of clinics post-call, versus non-post-call.
- We demonstrate quantitative evidence that patients may safely consult post-call registrars in clinic.
- Impairment may be mitigated by adaptive effort to be conscientious and post call euphoria.
- No recommendations were made to change the current practice of registrars running post-call clinics.
I. INTRODUCTION
Sleep deprivation and fatigue are thought to have detrimental effects on trainee doctors’ performance. It was previously shown that the Epworth Sleepiness Scale score in junior doctors was equivalent to that of patients with sleep apnoea and narcolepsy (Mustafa et al., 2005). Indeed, cognitive psychomotor performance after 24 hours of sustained wakefulness was found to be equivalent to a blood alcohol concentration twice the prohibited level of alcohol intoxication (Dawson & Reid, 1997). The performance and safety to practise of fatigued trainee doctors, especially at the end of a long shift, is thus of utmost concern.
Increasing awareness of fatigue-related medical errors has led to reforms in trainee doctor working hours. Work hours were limited by the Accreditation Council for Graduate Medical Education (ACGME) in the USA in 2003 to 80 hours per week, and by the European Working Time Directive (EWTD) in 2009 to 48 hours per week. A subsequent ACGME stipulation in 2017 further restricted work periods to 24 consecutive hours for first‐year residents (Rosenbaum & Lamas, 2012). Still, doubts remain as to the clinical impact of these restrictions (Baldwin et al., 2011; Fletcher et al., 2005). A systematic review of ACGME’s 2011 work hour restrictions found no improvements in patient care or resident well-being, and in fact revealed unintended negative impacts on resident education (Bolster & Rourke, 2015). Indeed, low job satisfaction was found to be associated with a higher rate of attrition from training (Lee et al., 2019). Thus, the optimal working hours and working patterns for trainee doctors remain ill-defined.
Studies on the impact of sleep deprivation and fatigue on trainee doctors’ performance and wellbeing have yielded mixed results. Chronic sleep deprivation was shown to be particularly detrimental to tasks requiring sustained concentration (Bertram, 1988). After an extended night shift, intensive care unit physicians made 36% more serious medical errors (Landrigan et al., 2004), were 61% more likely to suffer a percutaneous injury (Ayas et al., 2006) and 2.3 times more likely to have a motor vehicle collision (Barger et al., 2005). Hostility and anger in trainee doctors were also more prevalent after a night’s sleep loss (Saadat et al., 2016; Samkoff & Jacques, 1991). Cardiologists were particularly prone to sleep deprivation due to frequent call coverage responsibilities, and in a recent 2019 survey of 481 cardiologists, 46% felt work performance hindrance and 8.6% described sleep-deprivation related adverse events (Lobo et al., 2019).
Yet, other studies have not observed a similar impairment of ability amongst fatigued trainee doctors. There were fewer errors in cognitive tests and cardiopulmonary resuscitation (CPR) manoeuvres in residents after on-call duty (Domínguez et al., 2009; Hamui-Sutton et al., 2013), and psychomotor performance and acquisition of laparoscopic and robotic simulator skills in post-call trainee doctors were also found to be no different from non-post-call trainee doctors (Robison et al., 2018; Yi et al., 2013).
Notably, the outcome measures in the vast majority of these published studies were either subjective through interviews with the trainee doctors themselves, which introduces bias in results, or based on performance on robotic surgical simulators, which is not reflective of true patient contact. Few studies focused on actual patient outcome measures.
Trainee doctors (“registrars”) at our institution, a high volume tertiary referral centre for cardiovascular medicine in Singapore, may be expected to run busy outpatient clinics after a 24-hour continuous in-hospital shift. Typically, up to 20 patients are seen within 4 hours in these clinics. Concerns linger regarding the suitability of post-call registrars running these high-intensity clinics, both in terms of psychomotor ability as well as proneness to error.
With the lack of published literature on the impact of fatigue on trainee doctor performance in outpatient clinics, we aimed to study for ourselves whether patient outcomes were adversely affected if they consulted a post-call registrar, versus a non-post-call registrar. To achieve this, we decided on two practical and measurable outcomes: patient satisfaction and prescribing error rates. Quantifying patient satisfaction allowed an assessment of the registrars’ ability to communicate and show empathy despite their fatigued state. Prescribing error rates allowed an objective evaluation of patient safety. Using two very different outcome measures was a means to allow some triangulation of results and to reduce bias.
Our hypothesis was that both patient outcome measures – patient satisfaction and prescribing error rate – would be worse off in the clinics run by registrars when they were post-call versus when they were not post-call.
II. METHODS
A. Study Setting and Population Design
This study was set in a high volume, specialised Cardiology clinic in a large teaching hospital in Singapore. Registrars, who are trainee doctors in the final stages of training prior to specialist accreditation, work overnight in-hospital shifts as part of service and training commitments. “On-call” duties last from 7am to 1pm the following day (30 continuous hours), during which they are responsible for all urgent inpatient and Emergency department Cardiology referrals. “Post-call” refers to the last 6 hours of the continuous 30-hour shift, during which they may be posted to run busy outpatient clinics.
B. Patient Recruitment
Between November 2015 and February 2016, all patients who attended clinics run by a post-call registrar were recruited to the post-call group. Patients who attended clinics run by the same registrar on a non-post-call day were recruited as controls into the non-post-call group. This provided internal control by comparing performances by the same registrar post-call and non-post call. Patients were approached for participation after their clinic consultation so as not to bias the consultation. They were informed of the purpose of the study but not informed whether the registrar they had just consulted was post-call or not, so as not to bias their responses. All patients, whether new or established, were approached.
C. Patient Satisfaction Questionnaire
Patient satisfaction was evaluated using a 5 item questionnaire (Appendix A). These questions were adapted from the Hospital Consumer Assessment of Healthcare Providers And Systems (HCAHPS), a well-established standardised instrument for the measurement of patient perspectives on hospital care (Giordano et al., 2009; Goldstein et al., 2005).
1) During today’s consultation, did the doctor treat you with courtesy and respect?
2) During today’s consultation, did you feel the doctor listened carefully to you?
3) During today’s consultation, were you given the opportunity to ask your questions?
4) During today’s consultation, did the doctor explain things in a way you could understand?
5) How would you rate your overall satisfaction with today’s consultation?
For each item, as per the HCAHPS questionnaire format, patients were asked to rate responses on a 4-point Likert scale. Smiley faces were incorporated to provide visual representations. The questionnaire was in English and Chinese text, which would have been understood by the vast majority of the patient population. Relevant translations in Chinese, Malay or Tamil languages were provided by research assistants for illiterate patients or those who required further clarification, with care not to influence the patients’ responses. Only fully completed questionnaires were included in the data analysis.
D. Prescribing Error Rates
All prescription orders entered electronically were logged. As is standard procedure for our outpatient clinics, all prescriptions are reviewed by the Pharmacy Department prior to dispensing. All suspected prescription errors will be verified via a phone call to the prescribing doctor, who will confirm whether that prescription was intended or if it truly was an error. All verified prescription errors, including medication name, dose or frequency, or omission of a necessary drug, were recorded regardless of severity. The Pharmacy Department conducts regular internal audits to ensure that this process is accurate and consistent.
The total number of medications ordered and total number of errors were retrospectively summed. Prescribing error rate was calculated by dividing total number of prescribing errors by total number of medications ordered.
E. Consent and Ethics
In accordance with local Institutional Review Board (IRB) guidelines, the study protocol was exempted from full IRB review as it was non-interventional and intended primarily for medical education. All recruited patients provided informed consent to participate. All data were anonymised, with no personal identifiers recorded.
F. Data Analysis
For the patient satisfaction questionnaire, the “top-box” response was defined as the most positive response on the Likert scale (for example “all of the time” or “very satisfied”). The proportions of “top-box” responses were calculated and reported for each questionnaire item and overall items. Only “top-box” responses were sought, to target a higher quality of performance.
For both patient satisfaction and prescribing error outcomes, comparisons between post-call and non-post-call groups were tested for statistical significance with p<0.05 using the chi-squared test. All statistical analyses were reviewed by a biostatistician.
III. RESULTS
The recruitment period consisted of 9 outpatient clinics run by 8 post-call registrars. Two of these clinics were run by the same registrar who was post-call on separate days. We then identified a further 9 clinics run by the same registrars during days when they were not post-call. Thus, 7 registrars had one post-call clinic and one non-post-call clinic studied, while 1 registrar had two post-call clinics and two non-post-call clinics studied.
All patients seen were invited to participate. 103 of 106 (97%) patients in the post-call group and 93 of 105 (90%) in the non-post-call group consented. The number of patients seen per clinic ranged from 7 to 20 (median 11) in the post-call group, and 7 to 17 (median 10) in the non-post-call group.
Basic demographic data on the registrars and the distribution of patients in these clinics were summarised in Table 1.
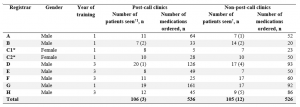
Table 1: Basic demographic data of registrars and distribution of patients seen and number of medications ordered per clinic.
Note: [1] †Numbers in brackets indicate number of patients who declined participation. *C1 and C2 refer to the same registrar, who had 2 post-call and 2 non-post-call clinics from whom patients were recruited for the study.
A. Patient Satisfaction Questionnaire
Questionnaire completion rate was 99% in both groups. Percentages of top-box responses were higher in the post-call group as compared with non-post-call group for item 1 (86% versus 65%, p<0.001), item 2 (82% versus 64%, p=0.003), item 3 (81% versus 65%, p=0.012) and item 4 (79% versus 63%, p=0.01). There was no statistical difference in the percentage of top-box responses for item 5 (64% versus 54%, p=0.184). Overall, percentage of top-box responses was higher in the post-call group compared to non-post-call group (79.3% versus 62.4%, p<0.001).
Percentages of top-box responses for each questionnaire item were illustrated in Figure 1. Individual registrars’ ratings were shown in Appendix B.
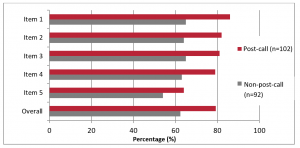
Figure 1: Summary of patient questionnaire responses according to registrars’ post-call status. Questionnaire items were shown on the y-axis and percentage of top-box responses were shown on the x-axis.
B. Prescribing Error Rates
536 and 526 medications were ordered in the post-call and non-post-call group respectively. Seven prescribing errors were made in the post-call group and 12 in the non-post-call group (Table 2).
Overall, there was no significant difference in prescribing error rates (1.31% versus 2.28%, p=0.231).

Table 2: Distribution of medications ordered and prescribing errors made according to registrar.
IV. DISCUSSION
To our knowledge, this is one of very few studies on post-call trainee doctor performance in the context of a realistic outpatient setting, centred on patient outcomes. In our study, the results of both patient satisfaction and prescription errors were congruent in demonstrating that these measurable patient outcomes were not adversely affected when patients were seen by a post-call registrar in an outpatient clinic setting.
A. Patient Satisfaction
Patient satisfaction is an important measure as it demonstrates a doctor’s ability to communicate, which is a key element of any patient-doctor encounter. Fatigue leading to increased stress levels and hostility could have negatively influenced this.
In our study, rather than create a novel and unvalidated questionnaire, we adapted the HCAHPS, a well-established standardised instrument for the measurement of patient perspectives on hospital care (Giordano et al., 2009; Goldstein et al., 2005). As per HCAHPS, only the proportions of top-box responses (i.e., the percentage of patients who rated a particular questionnaire item the most positively) were taken into account in the analysis. This was a means of assessing and aiming for the highest quality of care possible.
The results from overall and individual item top-box responses in our questionnaire demonstrated that patient satisfaction was statistically significantly (p-value <0.001) higher in the post-call group. Indeed, 6 out of 8 registrars had higher percentages of overall top-box responses when post-call, adding consistency to this finding. Nonetheless, given the small cohort of registrars surveyed, there were still the likelihood that this was a chance finding, and previous studies in this area had shown only subtle differences in patient satisfaction (Hoellein et al., 2004; Liu & Wissow, 2011). The key take away point was that patient satisfaction in our study was not adversely affected when patients saw a post-call registrar.
There were two other studies examining post-call trainee doctors in outpatient clinics. In Liu and Wissow’s study (2011), 170 pre-recorded paediatric clinic consultations were analysed to reveal that parents were twice as likely to request a post-call doctor to repeat explanations, both post-call doctors and parents used paraphrasing more frequently to check that they understood each other, and trainee doctors were perceived as less willing to help the patient accomplish their goals during the visit. This suggested that communication was less effective when trainee doctors were post-call. The earlier study by Hoellein et al. (2004), using a 7-item 10-point Likert scale questionnaire, found that patients were significantly less satisfied (mean score 8.99) when seen by a post-call trainee doctor than when seen by a non-post-call trainee doctor (mean score 9.31). Differences in study design and clinic setup could explain the discrepancy between our findings and those of these 2 previous studies. In these 2 studies, patient volume was low at 3 to 7 per clinic, trainee doctors and patients were aware that they were being recorded, and some clinics surveyed were the trainee doctors’ “continuity clinics” where visits were more likely returning patients with already established rapport. In our clinic setting, patient volumes were higher, patients were only approached after the consultation, and none of the clinics were “continuity clinics”.
Another possible explanation for the lack of reduction in patient satisfaction in our study was the phenomenon of “post-call euphoria”, where trainee doctors experience an upbeat mood associated with being able to look forward to the end of a long 30-hour shift and finishing work earlier than usual, at 1 p.m. instead of at 6 p.m. They may be emotionally less stressed in clinic than if they had a long day of work ahead, particularly if they were just starting an on-call shift. In Liu and Wissow’s study (2011), trainee doctors reported more anxiety and frustration when running morning clinics when they still had the rest of the day’s work ahead of them. Additionally, they described themselves as tired, but not more unhappy, when they were post-call as opposed to when they had left on time the day before. Furthermore, post-call trainee doctors made attempts to cope with their fatigue, adaptively or maladaptively, and were seemingly able to compensate for compromised abilities. This counter-intuitive psychological effect warrants further study.
B. Prescribing Error Rates
Prescribing errors were evaluated as a marker of patient safety. Errors have been shown to be provoked by situations of high workload, stress and fatigue (Keers et al., 2013; Tully et al., 2009). Overall case volume in particular was associated with increased rate of major diagnostic discrepancies for junior residents (Hanna et al., 2016), which is relevant to our high-volume clinic setting. The questionnaire among anaesthesiologists from Santa Catarina by Erdmann et al. (2016) revealed that most respondents committed more than one error in drug administration, with distraction and fatigue being the highest contributing factor of 64.9%. Interns made substantially more serious medical errors in the intensive care unit when they worked frequent shifts of 24 hours or more, than when they worked shorter shifts (Landrigan et al., 2004). There was only one other study that dealt specifically with medication errors in the post-call setting. In a retrospective study of 8,195 inpatient prescriptions, trainee doctors were found to be significantly more likely to commit an error on-call and post-call, than when they were off-call, by 2.16%, with odds ratio 1.44 (Hendey et al., 2005).
Our study in the outpatient setting revealed no statistically significant difference in prescribing error rates between patients who had seen a post-call registrar (1.31%) and those who had seen a non-post-call registrar (2.28%) across 536 and 526 prescriptions respectively. The overall prescribing error rate seen in our study was comparable to that of Hendey et al. (2005) (1.79% versus 2.16%, respectively), supporting the validity of our results. Importantly, prescribing error rates were low in both groups, providing reassurance for patient safety.
Previous studies on the impact of fatigue on clinical performance show mixed results. Surgical trainees awake the previous night made 20% more errors in stimulators (Taffinder et al., 1998). Gastroenterologists who performed emergent procedures the previous night had a significant 24% decrease in adenoma detection rates on colonoscopies performed post-call (Benson et al., 2014). While long work hours may contribute to mistakes, the lack of supervision, faulty handovers and large patient caseloads were important factors that further compounded these errors.
Yet, other studies have observed that performance was no worse amongst fatigued trainee doctors. Yi et al. (2013) found no significant difference in psychomotor performance of general surgery residents performing laparoscopic simulator tasks after a 24-hour call work shift versus a 12-hour night-float shift. Robison et al. (2018) reported no significant difference in acquisition of robotic simulator skills between pre-call and post-call general surgery residents despite higher levels of fatigue, and Domínguez et al. (2009) and Hamui-Sutton et al. (2013) observed fewer errors in cognitive tests and CPR manoeuvres in residents after on-call duty. This paradox of improved execution might be explained by an increased motivation to execute tasks as efficiently as possible, even if cognitive processes were theoretically impaired by sleep deprivation (Ayas et al., 2006; Barger et al., 2005; Taffinder et al., 1998).
Additionally, it was postulated that alertness and task performance were impaired immediately in the first 2 hours of awakening due to sleep inertia, but these detrimental effects dissipate with time (Jewett et al., 1999). Post-call residents in our study might therefore have had a chance to recover by the time clinic started.
C. Strengths and Limitations
A particular strength of our study was that registrars who had post-call clinics surveyed also had a non-post-call clinic surveyed. This enabled them to act as controls for themselves and reduced potential bias that may be introduced as a result of differences in registrar demographics, such as age, gender and training experience. Second, there was a high patient participation rate in both the post-call group (97%) and non-post-call group (90%), with a high questionnaire return rate (99% in both groups). This increased the validity of our findings. Third, our study measured two different patient outcomes as a means of triangulation, and both were congruent in showing better outcomes in the post-call group. Fourth, we approached patients for their participation only after their clinic consultation, so as not to have influenced their interaction with the doctor. Fifth, patients were not informed if the registrar that they had just consulted was post-call or not, so as not to influence their questionnaire responses.
Nonetheless, being a single-centre study, caution should be exercised when attempting to generalise these findings to other healthcare settings. Second, only 8 of 18 eligible registrars in the department had clinics surveyed during the study period; thus the findings may not be reflective of the entire cohort. Third, there may have been factors outside the doctor-patient encounter that affected overall patient satisfaction, such as waiting times. Fourth, we did not quantify how busy each registrar’s on-call shift was and what amount of rest they obtained; the results might have been influenced by the amount of rest obtained. Fifth, we could not control for the complexity of the patients seen in the clinics; it is perceivable that a clinic with more straightforward patients would have been more easily managed by a fatigued registrar and vice versa.
For future studies, increasing cohort size of registrars over a longer period of time, and at more categories of call status (such as post-call, on-call and neither post- nor on-call) could improve the generalisability of the findings and reveal influences of call status on performance. In addition, incorporating qualitative data on registrars’ emotions and perceptions of their own performances in clinic would improve understanding of potential factors that may influence performance.
V. CONCLUSION
Our study showed that patient satisfaction and prescription error rates were not adversely affected when patients consulted a post-call registrar versus a non-post-call registrar in an outpatient clinic. This provides reassurance that the current practice of post-call trainee doctors running clinics is not harmful to patients. Complex interactions of associated positive and negative emotional factors could possibly compensate for any physical and mental tiredness. Impairment may be mitigated by adaptive effort to be conscientious. In our institution, no recommendations were made to change the current practice of registrars running post-call clinics. Ultimately, the relationship between being post-call with physician performance and patient outcomes remains poorly understood.
Notes on Contributors
Dr. Chin Chee Yang is a Consultant in Cardiology at the National Heart Centre Singapore and Clinical Assistant Professor at Duke-NUS Medical School. He has a Master of Science in Clinical Education. CCY designed and directed the study, implemented the research, data analysis and writing of the manuscript.
Dr. Tan Si Qi is a Medical Officer with the Ministry of Health Holdings, Singapore. TSQ contributed to the data analysis and writing of the manuscript.
Dr. Kui Swee Leng is a senior resident in Cardiology at Singhealth. She is an Adjunct Research Fellow with Singhealth Duke-NUS Cardiovascular Sciences Academic Clinical Programme (ACP) and Singhealth Associate in Education. KSL contributed to design and implementation of the research.
Assistant Professor Kurugulasigamoney Gunasegaran is a Senior Consultant at the National Heart Centre Singapore. KG contributed to the design and overall supervision of the research.
Dr. Jill Cheng Sim Lee is a Consultant in Obstetrics and Gynaecology and Associate Programme Director to the SingHealth Obstetrics and Gynaecology Residency Programme. She has a Master of Science in Clinical Education. JCSL contributed to the design of the research and writing of the manuscript.
All authors have read and approved the final manuscript.
Ethical Approval
The study was categorised as an educational study hence formal Institutional Board Review (IRB) was exempted. We have attached the Local IRB Exception waiver document.
Funding
No funding source was utilised in this study.
Declaration of Interest
Authors report no declaration of interest.
Data Availability
In our study, all raw data from questionnaires was collected on hard copies and not scanned into a repository. All other data are presented in the direct manuscript.
References
Ayas, N. T., Barger, L. K., Cade, B. E., Hashimoto, D. M., Rosner, B., Cronin, J. W., Speizer, F. E., & Czeisler, C. A. (2006). Extended work duration and the risk of self-reported percutaneous injuries in interns. Journal of the American Medical Association, 296(9), 1055–1062. https://doi.org/10.1001/jama.296.9.1055
Baldwin, K., Namdari, S., Donegan, D., Kamath, A. F., & Mehta, S. (2011). Early effects of resident work-hour restrictions on patient safety: A Systematic review and plea for improved studies. The Journal of Bone and Joint Surgery-American Volume, 93(2), e5(1)-e5(9). https://doi.org/10.2106/JBJS.J.00367
Barger, L. K., Cade, B. E., Ayas, N. T., Cronin, J. W., Rosner, B., Speizer, F. E., & Czeisler, C. A. (2005). Extended work shifts and the risk of motor vehicle crashes among interns. New England Journal of Medicine, 352(2), 125–134. https://doi.org/10.1056/NEJMoa041401
Benson, M., Grimes, I., Gopal, D., Reichelderfer, M., Soni, A., Benson, H., Austin, K., & Pfau, P. (2014). Influence of previous night call and sleep deprivation on screening colonoscopy quality. The American Journal of Gastroenterology, 109(8), 1133–1137. https://doi.org/10.1038/ajg.2014.28
Bertram, D. A. (1988). Characteristics of shifts and second-year resident performance in an emergency department. New York State Journal of Medicine, 88(1), 10–14.
Bolster, L., & Rourke, L. (2015). The Effect of Restricting Residents’ Duty hours on patient safety, resident well-being, and resident education: An updated systematic review. Journal of Graduate Medical Education, 7(3), 349–363. https://doi.org/10.4300/JGME-D-14-00612.1
Dawson, D., & Reid, K. (1997). Fatigue, alcohol and performance impairment. Nature, 388(6639), 235–235. https://doi.org/10.1038/40775
Domínguez, P., Grosso, M. L., Pagotto, B., Taliercio, V., & Allegri, R. (2009). Efectos de la privación de sueño en el desempeño de los médicos residentes de pediatría [Effects of sleep deprivation on medical performance of pediatric residents]. Archivos Argentinos De Pediatria, 107(3), 241–245.
Erdmann, T. R., Garcia, J. H. S., Loureiro, M. L., Monteiro, M. P., & Brunharo, G. M. (2016). Profile of drug administration errors in anesthesia among anesthesiologists from Santa Catarina. Brazilian Journal of Anesthesiology (Elsevier), 66(1), 105–110. https://doi.org/10.1016/j.bjane.2014.06.011
Fletcher, K. E., Underwood, W., Davis, S. Q., Mangrulkar, R. S., McMahon, L. F., & Saint, S. (2005). Effects of work hour reduction on residents’ lives: A systematic review. Journal of the American Medical Association, 294(9), 1088–1100. https://doi.org/10.1001/jama.294.9.1088
Giordano, L. A., Elliott, M. N., Goldstein, E., Lehrman, W. G., & Spencer, P. A. (2009). Development, implementation, and public reporting of the HCAHPS survey. Medical Care Research and Review, 67(1), 27–37. https://doi.org/10.1177/1077558709341065
Goldstein, E., Farquhar, M., Crofton, C., Darby, C., & Garfinkel, S. (2005). Measuring hospital care from the patients’ perspective: An overview of the CAHPS® hospital survey development process: Measuring hospital care from the patients’ perspective. Health Services Research, 40(6p2), 1977–1995. https://doi.org/10.1111/j.1475-6773.2005.00477.x
Hamui-Sutton, L., Barragán-Pérez, V., Fuentes-García, R., Monsalvo-Obregón, E. C., & Fouilloux-Morales, C. (2013). Efectos de la privación de sueño en las habilidades cognitivas, psicomotoras y su relación con las características personales de los médicos residentes [Sleep deprivation effects on cognitive, psychomotor skills and its relationship with personal characteristics of resident doctors]. Cirugia Y Cirujanos, 81(4), 317–327.
Hanna, T. N., Loehfelm, T., Khosa, F., Rohatgi, S., & Johnson, J. (2016). Overnight shift work: factors contributing to diagnostic discrepancies. Emergency Radiology, 23(1), 41-47. https://doi.org/10.1007/s10140-015-1355-0
Hendey, G. W., Barth, B. E., & Soliz, T. (2005). Overnight and postcall errors in medication orders. Academic Emergency Medicine, 12(7), 629–634. https://doi.org/10.1197/j.aem.2005.02.009
Hoellein, A. R., Feddock, C. A., Griffith, C. H., Wilson, J. F., Barnett, D. R., Bass, P. F., & Caudill, T. S. (2004). Are continuity clinic patients less satisfied when the resident is postcall? Journal of General Internal Medicine, 19(5p2), 562–565. https://doi.org/10.1111/j.1525-1497.2004.30165.x
Jewett, M. E., Wyatt, J. K., Ritz-De Cecco, A., Khalsa, S. B., Dijk, D. J., & Czeisler, C. A. (1999). Time course of sleep inertia dissipation in human performance and alertness. Journal of Sleep Research, 8(1), 1–8. https://doi.org/10.1111/j.1365-2869.1999.00128.x
Keers, R. N., Williams, S. D., Cooke, J., & Ashcroft, D. M. (2013). Prevalence and nature of medication administration errors in health care settings: A Systematic review of direct observational evidence. Annals of Pharmacotherapy, 47(2), 237–256. https://doi.org/10.1345/aph.1R147
Landrigan, C. P., Rothschild, J. M., Cronin, J. W., Kaushal, R., Burdick, E., Katz, J. T., Lilly, C. M., Stone, P. H., Lockley, S. W., Bates, D. W., & Czeisler, C. A. (2004). Effect of reducing interns’ work hours on serious medical errors in intensive care units. New England Journal of Medicine, 351(18), 1838–1848. https://doi.org/10.1056/NEJMoa041406
Lee, J. C. S., Kee, X. L. J., Wiener-Ogilvie, S., Chern, B. S. M., & Chin, C. Y. (2019). What drives attrition amongst obstetrics and gynaecology residents in Singapore. The Asia Pacific Scholar, 4(1), 34–41. https://doi.org/10.29060/TAPS.2019-4-1/OA2005
Liu, C.-C., & Wissow, L. (2011). How post-call resident doctors perform, feel and are perceived in out-patient clinics: Post-call residents seeing outpatients. Medical Education, 45(7), 669–677. https://doi.org/10.1111/j.1365-2923.2010.03912.x
Lobo, A. S., Sandoval, Y., Burke, M. N., Sorajja, P., Mooney, M., Traverse, J., Henry, T. D., Chavez, I., Gössl, M., Lips, D. L., Bradley, S. M., Poulose, A., Wang, Y., & Brilakis, E. S. (2019). Sleep deprivation in cardiology: A multidisciplinary survey. The Journal of Invasive Cardiology, 31(6), 195–198.
Mustafa, M., Erokwu, N., Ebose, I., & Strohl, K. (2005). Sleep problems and the risk for sleep disorders in an outpatient veteran population. Sleep and Breathing, 9(2), 57–63. https://doi.org/10.1007/s11325-005-0016-z
Robison, W., Patel, S. K., Mehta, A., Senkowski, T., Allen, J., Shaw, E., & Senkowski, C. K. (2018). Can fatigue affect acquisition of new surgical skills? A prospective trial of pre- and post-call general surgery residents using the da Vinci surgical skills simulator. Surgical Endoscopy, 32(3), 1389–1396. https://doi.org/10.1007/s00464-017-5820-6
Rosenbaum, L., & Lamas, D. (2012). Residents’ Duty hours — Toward an empirical narrative. New England Journal of Medicine, 367(21), 2044–2049. https://doi.org/10.1056/NEJMsr1210160
Saadat, H., Bissonnette, B., Tumin, D., Thung, A., Rice, J., Barry, N., & Tobias, J. (2016). Time to talk about work-hour impact on anesthesiologists: The effects of sleep deprivation on Profile of Mood States and cognitive tasks. Pediatric Anesthesia, 26(1), 66–71. https://doi.org/10.1111/pan.12809
Samkoff, J. S., & Jacques, C. H. (1991). A review of studies concerning effects of sleep deprivation and fatigue on residents’ performance. Academic Medicine, 66(11), 687–693. https://doi.org/10.1097/00001888-199111000-00013
Taffinder, N., McManus, I., Gul, Y., Russell, R., & Darzi, A. (1998). Effect of sleep deprivation on surgeons’ dexterity on laparoscopy simulator. The Lancet, 352(9135), 1191. https://doi.org/10.1016/S0140-6736(98)00034-8
Tully, M. P., Ashcroft, D. M., Dornan, T., Lewis, P. J., Taylor, D., & Wass, V. (2009). The causes of and factors associated with prescribing errors in hospital inpatients: A Systematic Review. Drug Safety, 32(10), 819–836. https://doi.org/10.2165/11316560-000000000-00000
Yi, W. S., Hafiz, S., & Sava, J. A. (2013). Effects of night-float and 24-h call on resident psychomotor performance. Journal of Surgical Research, 184(1), 49–53. https://doi.org/10.1016/j.jss.2013.03.029
*Chin Chee Yang
National Heart Centre Singapore
5 Hospital Drive, Singapore 169609
Tel: +65 6704 8962
E-mail: chin.chee.yang@singhealth.com.sg
Announcements
- Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Volume 9 Number 1 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors. - Volume 8 Number 3 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2021
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2021.
Refer here for the list of recipients. - Most Accessed Article 2021
The Most Accessed Article of 2021 goes to Professional identity formation-oriented mentoring technique as a method to improve self-regulated learning: A mixed-method study.
Congratulations, Assoc/Prof Matsuyama and co-authors. - Best Reviewer Awards 2020
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2020.
Refer here for the list of recipients. - Most Accessed Article 2020
The Most Accessed Article of 2020 goes to Inter-related issues that impact motivation in biomedical sciences graduate education. Congratulations, Dr Chen Zhi Xiong and co-authors. - Scopus
TAPS has been accepted for inclusion in Scopus! - Best Reviewer Awards 2019
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2019.
Refer here for the list of recipients. - Most Accessed Article 2019
The Most Accessed Article of 2019 goes to A two-edged sword: Narrative inquiry into Japanese doctors’ intrinsic motivation. Congratulations,
Professor Hiroshi Nishigori and co-authors!









