The associates of Emotional Intelligence in medical students: A systematic review
Submitted: 23 November 2021
Accepted: 10 May 2022
Published online: 4 October, TAPS 2022, 7(4), 59-70
https://doi.org/10.29060/TAPS.2022-7-4/OA2714
Deepthi Edussuriya1, Sriyani Perera2, Kosala Marambe3, Yomal Wijesiriwardena1 & Kasun Ekanayake1
1Department of Forensic Medicine, Faculty of Medicine, University of Peradeniya, Sri Lanka; 2Medical Library, University of Peradeniya, Sri Lanka; 3Department of Medical Education, Faculty of Medicine, University of Peradeniya, Sri Lanka
Abstract
Introduction: Emotional Intelligence (EI) is especially important for medical undergraduates due to the long undergraduate period and relatively high demands of the medical course. Determining associates of EI would not only enable identification of those who are most suited for the discipline of medicine but would also help in designing training strategies to target specific groups. However, there is diversity of opinion regarding the associates of EI in medical students. Aim of the study was to determine associates of EI in medical students.
Methods: The databases MEDLINE, CENTRAL, Scopus, EbscoHost, LILAC, IMSEAR and three others were searched. It was followed by hand-searching, cited/citing references and searching through PQDT. All studies on the phenomenon of EI and/or its associates with medical students as participants were retrieved. Studies from all continents of the world, published in English were selected. They were assessed for quality using Q-SSP checklist followed by narrative synthesis on selected studies.
Results: Seven hundred and ninety-two articles were identified of which 29 met inclusion criteria. One article was excluded as its full text was not available. Seven articles found an association between ‘EI and academic performance’, 11 identified an association between ‘EI and mental health’, 11 found an association between ‘EI and Gender’, 6 identified an association between ‘EI and Empathy’ while two have found an association with the learning environment.
Conclusion: Higher EI is associated with better academic performance, better mental health, happiness, learning environment, good sleep quality and less fatigue, female gender and greater empathy.
Keywords: Emotional Intelligence, Associates of Emotional Intelligence, Medical Students, Mental Wellbeing, Empathy
Practice Highlights
- Higher emotional intelligence is associated with better academic performance.
- Higher emotional intelligence is associated with better mental health.
- Higher emotional intelligence is associated with female gender.
- Higher emotional intelligence is associated with greater empathy.
I. INTRODUCTION
Emotional intelligence (EI) is defined as “the ability to perceive emotions accurately, appraise, and express emotion; the ability to assess and/or generate feelings when they facilitate thought; ability to understand emotions and emotional knowledge, and to regulate emotions to promote emotional and intellectual growth” (Mayer & Salovey, 1997). Studies have found that there is a positive effect between EI and academic as well as professional success (Suleman et al., 2019). It has been reported that people and college students with good EI show better social functioning and interpersonal relationship and peers have identified them as less antagonistic and conflictual (Petrovici & Dobrescu, 2014).
Several tests and instruments that have been used to assess the Emotional intelligence of medical students were identified through the literature. These include standard EI tests, modified versions of standard EI tests, and authors’ assessment methods of their own. Schutte self-report EI test, TEIQue questionnaire and Bar-on’s emotional intelligence questionnaire ((EQ-i) 2.0) have been used frequently. Each of these instruments has different advantages and disadvantages of their own.
The Emotional Quotient Inventory (EQ-i) 2.0 is a revision of the EQ-I (Bar-On, 2004). The Emotional Quotient Inventory (EQ-I) 2.0 measures the interaction between an individual and their environment. Since the EQ-i 2.0 is a revision of the original Emotional Quotient Inventory (EQ-I) the standard platform of the EQ-i validation remains intact.
The Schutte Self-Report Emotional Intelligence Test (SSEIT) is a method of measuring general Emotional Intelligence (EI), using four sub-scales: emotion perception, utilising emotions, managing self- relevant emotions, and managing others’ emotions (Schutte et al., 1998). The SSEIT model is closely associated with the EQ-I model of Emotional Intelligence. It has a reliability rating of 0.90. The EI score, overall, is fairly reliable for adults and adolescents. However, the utilising emotions sub-scale has shown poor reliability (Ciarrochi et al., 2001). Also, they report a mediocre correlation of the SSREI with self-estimated EI, the Big Five EI scale, and life satisfaction (Petrides & Furnham, 2000). However, SSREI correlated poorly with well-being and EI criteria.
The Trait Emotional Intelligence Questionnaire (TEIQue), is an openly accessible instrument developed to measure global trait emotional intelligence. Based on the Trait Emotional Intelligence Theory, a significant number of research has been conducted regarding emotional intelligence (EI) (Mikolajczak et al., 2007). The TEIQue is available in long form and short forms. Internal consistency and test-retest both indicated scale reliabilities of 0.71 and 0.76. High correlations between the TEIQue with Shrink’s Emotional Intelligence Scale showed validity in measuring emotional intelligence and the “Big Five” Personality Traits.
Apart from those assessment methods, Genos Emotional Intelligence Assessment, Mayer-Salovey-Caruso Emotional Intelligence Test, TMMS-24 data and DASS-21 scale, Bradbury-Graves’s Emotional Intelligence and Siberia Schering’s Emotional Intelligence Questionnaire have also been used by the authors to assess the EI.
A comprehensive survey in medicine states that EI had a positive contribution in doctor-patient relationship, increased empathy, teamwork, communication skills, stress management, organisational commitment and leadership (Arora et al., 2010). EI is invariably important to medical professionals as it is associated with self-monitoring which would not only ensure adapting to clinical situations appropriately and having desirable interpersonal relations but also result in a favorable outcome for the patient and the wellbeing of the practitioner.
Few studies suggest that EI training can help medical students to build their leadership and empathy skills, as they enter the clinical years (Austin et al., 2005; Dolev et al., 2019). Literature surveys on emotional intelligence and medicine, and physician leadership qualities concludes that EI correlates with many of the competencies that modern medical curricula seek to deliver including leadership (Mintz & Stoller, 2014; Reshetnikov et al., 2020). Other studies indicate that age and gender are associated with emotional intelligence. However, some studies showed that EI at medical school admission could not reliably predict academic success in later years (Reshetnikov et al., 2020). These studies have all looked at the associates in an isolated sense. However, it would also be interesting to reflect on the concept of EI in a broader sense as it is inevitable that there would be an interaction of factors.
The medical course extends over a period of five years as opposed to most undergraduate degrees which are shorter. Medical training involves close interactions with different categories of people including patients, doctors of different grades and the paramedical staff. Training includes long hours of work in stressful environments where some situations could be emotionally challenging. This long undergraduate period and relatively high demands of the medical course would require medical students to possess a high degree of EI. As findings of different studies on EI are sometimes diverse in opinion, it would be useful to conduct a systematic review to identify the associates of EI in order to design training strategies which target specific groups.
Even though EI is considered a trainable trait, the extent of trainability depends on many personal and institutional factors (Mattingly & Kraiger, 2019). Völker (2020) expresses that trainability in emotional intelligence is subjected to acquired knowledge which is situational and may depend on accumulating relevant experience.
In the Sri Lankan context, the sole criteria for selection of students to a medical course is the academic excellence at the Advanced level examination, which alone may not reflect their suitability to follow a profession like medicine (University Grants Commission, 2022).
However, since EI is an essential trait especially for medical practice many universities worldwide use different tools to assess EI in their applicants. Furthermore, different universities adopt varying techniques to develop EI of their students throughout the course. It is envisaged that this review would not only help determine what additional factors could be considered in the selection of applicants for a medical course but would also help teachers design training strategies to target specific groups of students and also ensure a more enjoyable and productive learning experience for the students as a whole. There is no doubt that these selection and intervention programs would produce doctors with more favourable qualities which would not only produce greater benefits to the patient but would prevent burn out among doctors.
A. Objective
The objective of this study is to find out, the associates of Emotional Intelligence in Medical students based on available literature in English from 2015 to 2020.
II. MATERIALS AND METHODS
The research question was defined based on the PICOS (Population, Intervention, Comparison, Outcomes and Setting) format. The review protocol was developed according to PRISMA-P 2015 (Preferred reporting items for systematic review and meta-analysis protocols) statement (Moher et al. 2015) by all three authors DE, KM and SP and was registered in the PROSPERO Registry (CRD42021227877). The methodology for the systematic review (SR) followed the guidelines and standards of IOM (Institute of Medicine) (Eden et al., 2011) and PRISMA-2015 for reporting.
A. Search Strategy
A Systematic and comprehensive search was conducted by SP in April 2020 and references were managed using the software Mendeley. The search explicitly aimed to identify all published and unpublished relevant studies in order to limit bias in the searching process. The key search terms were identified with the aid of a search-term-harvesting table by KM and DE. A combination of relevant medical subject headings and search terms tagged with other appropriate search fields were used in the literature search. The following databases were searched:
CDSR (Cochrane Database of Systematic Reviews), DARE (The Database of Abstracts of Reviews of Effects), MEDLINE (1950- 2020) via Pubmed (See supplemental Appendix 1 for search strategy), CENTRAL (The Cochrane Central Register of Controlled Trials, 1948 – 2020), Scopus, EbscoHost, LILAC, IMSEAR (Index Medicus for South East Asian region) and WHO International Clinical Trials Registry Platform (ICTRP). In addition to electronic searches, two key journals (2015-2020) were hand-searched, and cited & citing references of all included studies were screened for further relevant articles. Searches were limited to studies published between the years 2015-2020. Searching other resources included grey literature such as PQDT (ProQuest Dissertations and Thesis database) and Global health (via WHO).
B. Selection Criteria
After removal of duplicates from the retrieved articles, the remaining articles with abstracts were uploaded to the Web application, Rayyan (Quzzani et al., 2016) for the purpose of screening. The criteria for selection of articles were based on the PICOS elements. The studies were from all continents of the world and limited to those published in English. All studies focusing on the phenomenon of EI and/or its associates with medical students as participants were considered for inclusion in the review.
The authors DE, KM, SP and KE independently screened the uploaded articles in Rayyan, using the above eligibility criteria. In the first phase, title and abstract of each article were reviewed by any of the two authors independently for its candidacy. Following this initial evaluation, the full text of all those selected articles were retrieved and further examined by KM and DE independently (second phase), for the final verification before inclusion in the review. Any disagreements regarding eligibility of studies were resolved by consulting a third author (SP). Reviews, systematic reviews, editorials, letters and comments were removed. Articles which met the eligibility criteria were selected for inclusion in the review. Excluded studies were marked with the ‘reason’ in Rayyan.
C. Data Extraction and Quality Assessment
Data from all included studies were extracted by the review authors YW and KM using a data extraction table developed for the purpose of this review (Appendix 2). Data extracted were cross-checked by SP for any errors. Information recorded included: study details (author, year, country of origin), participants (number of participants, gender, level of undergrad program, etc.), methods (study aim, design, total study duration, tools used), study type (phenomenon /context studied) and outcomes (all relevant findings related to primary and secondary outcomes).
SP and YW independently assessed the quality of those selected studies using Quality Assessment Checklist for Survey Studies in Psychology (Q-SSP) (Protogerou & Hagger, 2020) Results of the quality assessments were compared (Appendix 3); any disagreements were resolved by consensus. Articles which met the required quality criteria were selected for inclusion in the review.
D. Strategy for Data Synthesis
Due to the heterogeneity between the included studies, a quantitative synthesis was not considered. A narrative synthesis of the findings from individual included studies was carried out by DE, based on the characteristics of the targeted populations and the type of outcome such as association/correlation of EI with academic performance, professional success, social functioning, interpersonal relationship, empathy, teamwork spirit, communication skills, stress management, organizational commitment, leadership quality, self-monitoring, mental health and emotional well-being.
III. RESULTS
A total of 792 articles were retrieved during the literature search. After removing the duplicates, 752 articles were considered for screening using the eligibility criteria. Initial evaluation of articles through title and abstract resulted in only 29 articles meeting the selection criteria. During the full-text evaluation, one article (Parijitham, 2018) was removed, as its full-text article could not be found even after contacting the author. The data that support the findings of this study are openly available at https://doi.org/10.6084/m9.figshare.15564210 (Edussuriya et al., 2021). Twenty-eight articles were finally selected for quality assessment. Flow diagram of the selection of studies is shown in Figure 1.
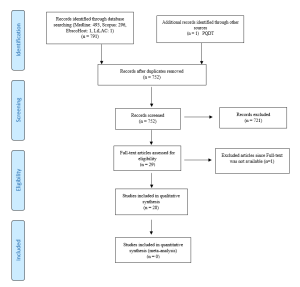
Figure 1. Flow diagram illustrating included and excluded studies in the systematic review
The study design of the selected studies comprised of 26 cross sectional (majority), one longitudinal and one quasi-experimental. However, all studies used standard validated survey questionnaires to collect data. Therefore, to assess the quality of selected studies, Quality Assessment Checklist for Survey Studies in Psychology (Q-SSP) was selected as the best, ‘applicable to all’ tool in this review, considering its relevance also to the trait emotional intelligence since emotions, thoughts and mental processes are aspects of psychology. The quality of the studies was determined by the extent to which the items on above checklist were met by each of the articles. There were 20 checklist items in the tool out of which one item (item-19 – Debriefing participants at the end of data collection) could be justifiably waived; one reason being none of the included studies used it in the methodology. Thus 19 items were considered to be applicable in this review (Appendix 4).
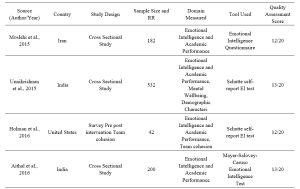



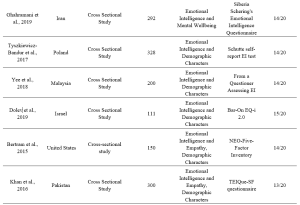

Table 1. Characteristics of included studies
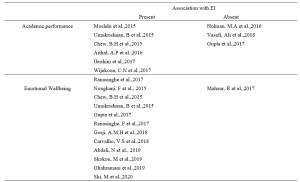

Table 2. Categorisation of findings of the studies
A. Findings of Studies and Data Analysis
1) EI and academic performance: According to studies, a positive correlation was identified between EI and academic performance (Aithal, et al., 2016, Ibrahim et al. 2017; Moslehi et al., 2015, Wijekoon et al., 2017) while (Ranasinghe et al., 2017; Unnikrishnan et al., 2015) also found a significant association between EI and academic performance. These studies indicated that students with higher EI intend to perform better in their academic work. A cross-sectional study done by Chew et al. (2015) showed that medical students with less emotional intelligence were largely unaware of their anxiety, which was associated with lower academic performance. According to studies done by Holman et al., 2016, Gupta et al., 2017 and Vasefi et al., 2018 there was no correlation of EI with academic performance. A study by Othman et al., 2020 revealed that EI showed a significant positive effect on intuitive decision-making style and a negative effect on avoidant and dependent decision-making styles which may explain better academic performance of medical students with high EI.
2) EI and mental health (emotional wellbeing): A direct relationship between EI and academic satisfaction was found in studies done by Rouhani et al., 2015, Unnikrishnan et al., 2015 and Carvalho et al., 2018. Further, Carvalho et al., 2018 reported that a positive relationship was observed between EI and academic-related well-being which accounts for both academic performance and mental health. It was seen that medical students with less emotional intelligence were largely unaware of their anxiety (Chew et al., 2015) and those with higher emotional intelligence perceived lesser stress (Gupta et al., 2017 and Ranasinghe et al., 2017). Shi and Du (2020) found that EI was strongly and negatively associated with Personal Distress. Heidari Gorji et al. (2018) identified a direct relationship between emotional intelligence and mental health while a study done by Mahaur et al. (2017) did not find a significant relationship between the two. Ghahramani et al. (2019) identified a significant positive relationship of EI with happiness while Abdali et al. (2019) showed a positive correlation with sleep quality and a negative correlation with general fatigue.
3) EI and demographic characters: Higher EI in females compared to males was found (Aithal et al., 2016, Bertram et al., 2015, Ibrahim et al., 2017, Khan et al., 2016, Raut & Gupta, 2019 Sundararajan and Gopichandran, 2018, Tyszkiewicz-Bandur et al., 2017, Unnikrishnan et al., 2015 and Wijekoon et al., 2017). Irfan et al. (2019) suggests that female medical students had significantly higher empathic behavior and emotional intelligence than male students. However, Skokou et al. (2019) did not find any difference in EI in males and females. Vasefi et al. (2018) and Abe et al. (2018) too did not find a significant relationship between EI and gender. However, Abe et al. (2018) revealed that females showed significantly higher Neuroticism, Agreeableness and Empathy scores than males. According to Ibrahim et al. (2017) increasing age resulted in higher EI. However, Yee et al. (2018) did not find a significant association of EI with age. According to Yee et al. (2018) there was no significant association of EI with ethnicity.
4) EI and empathy: Significant correlation between EI and Empathy was identified (Bertram et al., 2015, Irfan et al., 2019 Khan et al., 2016; Sundararajan & Gopichandran, 2018). Shi and Du (2020) suggests that EI helps medical professionals to establish a better association with the patient.
5) Learning environment: Relationship between EI and academic background was identified by both Irfan et al. (2019) and Sundararajan and Gopichandran (2018). According to Sundararajan and Gopichandran (2018), students who attended government schools for high school education had greater emotional intelligence than students from private schools. But Irfan et al. (2019) suggests that medical students of private medical schools showed higher level of empathy as compared to public medical schools. Dolev et al. (2019) reveals that there are no differences in EI levels between first-year and sixth-year medical students.
IV. DISCUSSION
The review included studies conducted in South and Southeast Asian, European, Arabian, North American and South American countries. Majority of studies on Asian students revealed a high association between EI and academic performance. However, two studies on Asian students and one on US students failed to observe such associations. The impact of EI on academic performance may be explained by the fact that being aware of one’s anxiety relieved stress and those with high EI experienced greater mental wellbeing and satisfaction with their programs; which may contribute to better academic performance. Furthermore, the fact that EI showed a positive correlation with better mental health/wellbeing, less perceived stress/distress, happiness, good sleep quality and less fatigue may account for the better academic performance of students with high EI.
Empathy is an important aspect in the delivery of high-quality healthcare. Several researchers from different regions of the world reported strong association between empathy and high EI scores. Therefore, assessment of EI may be useful in admitting students for medical degrees. However, since EI is considered as a “trainable trait”, the role that EI plays in admitting students to medical schools is debatable. Therefore, all efforts must be taken by medical schools to include activities that enhance EI, during the medical course, irrespective of the EI levels of students on admission. The fact that EI did not improve with seniority does not purely support the fact that EI is not trainable but it maybe those students were not exposed to and not sensitised to activities which enhance EI.
Evidence indicated a positive association between high EI scores and female gender. It maybe postulated that the “nurturing and caring” role assigned by society to the females influence their upbringing. Thereby improving their emotional intelligence.
In conclusion it must be stated that since a majority of studies revealed that higher EI is associated with better academic performance, better mental health and greater empathy and since EI is considered a trainable trait, curricular need to be developed with a view to improving EI.
In order to develop EI, curricular should contain programs on general leadership development, self-care/ wellness and burn-out prevention (Monroe & English, 2013). Small-group experiential learning activities and meeting with trained mentors throughout the years would be helpful. Debriefing sessions and maintaining a journal are some other techniques that need to be considered. It may be helpful to discuss change management and quality improvement with students (Audra et al., 2020). Exposure of students to skills of self-awareness and self-management through discussion, exposure to theories of conflict management, mindfulness practice, leadership training, discussions on learning styles, discussions on power and influence, identification of team dynamics, exposure to high-functioning inter-professional teams, peer coaching, health care leader interview and shadowing of experienced clinicians are some techniques that could be adopted in attempting to develop EI among students (Kozlowski & Ilgen, 2006). It would be beneficial to evaluate acquisition based on completion of an EI inventory, feedback from peers and staff, project presentations, reflective writing, measurement of achievement of professional and personal development benchmarks and milestones, performance on simulated scenarios and small-group exercises (Pan & Allison, 2010).
During the study it was observed that there is paucity of longitudinal studies on Associates of EI. Therefor it would be beneficial to conduct longitudinal studies which may help identify some aspects with regard to the trainability of EI in medical students.
V. CONCLUSION
Through this review it was revealed that higher EI is associated with
- better academic performance,
- better mental health including less perception of stress and distress, happiness, good sleep quality and less fatigue,
- female gender, and
- greater empathy.
No significant association was found between age, ethnicity, and seniority in the medical course, and emotional intelligence. No conclusions could be made about the association between the nature of the educational institute (private or state) and emotional intelligence.
A. Limitations
In this review, it was found that authors of included studies which used several different tools to assess the EI of medical students. Each of these tools have their own advantages and disadvantages which cause comparison difficult. It could not be assumed that, each and every one of these methods provide results in the same level.
B. Recommendation
Since high EI has shown a positive correlation with academic performance and better mental wellbeing of students and since it has been identified as a “trainable trait” all efforts should be made to enhance EI of medical students during their undergraduate training.
Notes on Contributors
Edussuriya D.H (DE) was the Principal Investigator of the study. Protocol drafting, study selection, analysis and interpretation of data, synthesis of findings of individual studies and the drafting of manuscript was done by the author.
Perera S. (SP) facilitated the methodology, involved in drafting the protocol and retrieved selected articles, since the author has previous experience in conducting systematic reviews. Reference management in Mendeley and Rayyan, cross-checking the extracted data, assessed quality of selected studies and final review of draft was also done by the author.
Marambe K.N (KM) was involved in drafting the protocol, involved in article selection and extracted data from the selected articles.
Wijesiriwardena W.M.S.Y (YW) extracted data from selected articles, assessed the quality of selected articles and finalised the manuscript.
Ekanayake E.M.K.B (KE) has screened the uploaded articles in Rayyan.
Ethical Approval
The review is registered in PROSPERO – The International Prospective Register of Systematic Reviews under the registration number CRD42021227877 for the systematic review.
Data Availability
Data set that support the findings of this study are openly available in Figshare repository https://doi.org/10.6084/ m9.figshare.15564210
Acknowledgement
The authors acknowledge Information Officers of National Science Library and Resources Center, National Science Foundation, Sri Lanka for support in Scopus searches and staff of Medical Library of Faculty of Medicine, University of Peradeniya for the assistance in finding full text articles of the included studies in the review.
Funding
No funding sources are associated with this study.
Declaration of Interest
No conflicts of interest are associated with this paper.
References
Abdali, N., Nobahar, M., & Ghorbani, R. (2019). Evaluation of emotional intelligence, sleep quality, and fatigue among Iranian medical, nursing, and paramedical students: A cross-sectional study. Qatar Medical Journal, 2019(3), 15. https://doi.org/10.5339/qmj.2019.15
Abe, K., Niwa, M., Fujisaki, K., & Suzuki, Y. (2018). Associations between emotional intelligence, empathy and personality in Japanese medical students. BMC Medical Education, 18, Article 47. https://doi.org/10.1186/s12909-018-1165-7
Aithal, A. P., Kumar, N., Gunasegeran, P., Sundaram, S. M., Rong, L. Z., & Prabhu, S. P. (2016). A survey-based study of emotional intelligence as it relates to gender and academic performance of medical students. Education for Health, 29(3), 255–258.
Arora, S., Ashrafian, H., Davis, R., Athanasiou, T., Darzi, A., & Sevdalis, N. (2010). Emotional intelligence in medicine: A systematic review through the context of the ACGME competencies. Medical education, 44(8), 749–764. https://doi.org/10.1111/j.1365-2923.2010.03709.x
Audra, V. W., O’Brien, T. C., Varvayanis, S., Alder, J., Greenier, J., Layton, R. L., Stayart,C. A., Wefes, I., & Brady, A. E. (2020). Applying experiential learning to career development training for biomedical graduate students and postdocs: Perspectives on program development and design. CBE—Life Sciences Education, 19(3), 1-12. https://doi.org/10.1187/cbe.19-12-0270
Austin, E. J., Evans, P., Goldwater, R., & Potter, V. (2005). A preliminary study of emotional intelligence, empathy and exam performance in first year medical students. Personality and Individual Differences, 39(8), 1395-1405. https://doi.org/10.1016/j.paid.2005.04.014
Bar-On, R. (2004). The Bar-On Emotional Quotient Inventory (EQ-i): Rationale, description and summary of psychometric properties. In G. Geher (Ed.), Measuring Emotional Intelligence: Common Ground and Controversy (pp. 115–145). Nova Science Publishers.
Bertram, K., Randazzo, J., Alabi, N., Levenson, J., Doucette, J. T., & Barbosa, P. (2016). Strong correlations between empathy, emotional intelligence, and personality traits among podiatric medical students: A cross-sectional study. Education for Health (Abingdon), 29(3), 186–194.
Carvalho, V. S., Guerrero, E., & Chambel, M. J. (2018). Emotional intelligence and health students’ well-being: A two-wave study with students of medicine, physiotherapy and nursing. Nurse Education Today, 63, 35–42. https://doi.org/10.1016/j.nedt.2018.01.010
Chew, B. H., Hassan, F., & Zain, A. M. (2015). Medical students with higher emotional intelligence were more aware of self-anxiety and scored higher in continuous assessment: A cross-sectional study. Medical Science Educator, 25(4), 421-430. https://doi.org/10.1007/s40670-015-0168-9
Ciarrochi, J., Chan, A. Y., & Bajgar, J. (2001). Measuring emotional intelligence in adolescents. Personality and Individual Differences, 31(7), 1105-1119. https://doi.org/10.1016/S0191-8869(00)00207-5.
Dolev, N., Goldental, N., Reuven-Lelong, A., & Tadmor, T. (2019). The evaluation of emotional intelligence among medical students and its links with non-cognitive acceptance measures to medical school. Rambam Maimonides Medical Journal, 10(2), e0010. https://doi.org/10.5041/RMMJ.10365
Eden, J., Levit, L., Berg, A., & Morton. S. (2011). Finding what works in health care: Standards for systematic reviews. National Academies Press. https://doi.org/10.17226/13059
Edussuriya, D., Perera, S., Marambe, K., Wijesiriwardena, Y., & Ekanayake, K. (2021). Emotional intelligence systematic review (Version 3) [Data Set]. Figshare. https://doi.org/10.6084/m9.figshare.15564210.v3
Ghahramani, S., Jahromi, A. T., Khoshsoroor, D., Seifooripour, R., & Sepehrpoor, M. (2019). The relationship between emotional intelligence and happiness in medical students. Korean Journal of Medical Education, 31(1), 29–38. https://doi.org/10.3946/kjme.2019.116
Gupta, R., Singh, N., & Kumar, R. (2017). Longitudinal predictive validity of emotional intelligence on first year medical students perceived stress. BMC Medical Education, 17(1), 139. https://doi.org/10.1186/s12909-017-0979-z
Heidari Gorji, A. M., Shafizad, M., Soleimani, A., Darabinia, M., Goudarzian, A. H. (2018) Path analysis of self-efficacy, critical thinking skills and emotional intelligence for mental health of medical students. Iranian Journal of Psychiatry and Behavioral Sciences. 12(4), e59487. https://doi.org/10.5812/ijpbs.59487
Holman, M. A., Porter, S. G., Pawlina, W., Juskewitch, J. E., & Lachman, N. (2016). Does emotional intelligence change during medical school gross anatomy course? Correlations with students’ performance and team cohesion. Anatomical Sciences Education, 9(2), 143–149. https://doi.org/10.1002/ase.1541
Ibrahim, N. K., Algethmi, W. A., Binshihon, S. M., Almahyawi, R. A., Alahmadi, R. F., & Baabdullah, M. Y. (2017). Predictors and correlations of emotional intelligence among medical students at King Abdulaziz University, Jeddah. Pakistan Journal of Medical Sciences, 33(5), 1080–1085. https://doi.org/10.12669/pjms.335.13157
Irfan, M., Saleem, U., Sethi, M. R., & Abdullah, A. S. (2019). Do we need to care: emotional intelligence and empathy of medical and dental students. Journal of Ayub Medical College, Abbottabad: JAMC, 31(1), 76–81.
Khan, M. A., Niazi, I. M., & Rashdi, A. (2016). Emotional intelligence predictor of empathy in medical students. Rawal Medical Journal, 41(1), 121-124.
Kozlowski, SWJ., & Ilgen. D.R. (2006). Enhancing the effectiveness of work groups and teams. Psychological Science in the Public Interest, 7(3), 77-124. https://doi.org/10.1111/j.1529-1006.2006.00030.x
Mahaur, R., Jain, P., & Jain, A. K. (2017). Association of mental health to emotional intelligence in medical undergraduate students: Are there gender differences? Indian Journal of Physiology and Pharmacology, 61(4), 383-391.
Mattingly, V., & Kraiger, K. (2019). Can emotional intelligence be trained? A meta-analytical investigation. Human Resource Management Review, 29(2), 140-155. https://doi.org/10.1016/j.hrmr.2018.03.002
Mayer, J. D., & Salovey, P. (1997). What is emotional intelligence? Emotional development and emotional intelligence: Educational implications (pp. 3-31). Basic Books.
Mikolajczak, M., Luminet, O., Leroy, C., & Roy, E. (2007). Psychometric properties of the Trait Emotional Intelligence Questionnaire: Factor structure, reliability, construct, and incremental validity in a French-speaking population. Journal of Personality Assessment, 88(3), 338–353. https://doi.org/10.1080/00223890701333431
Mintz, L. J., & Stoller, J. K. (2014). A systematic review of physician leadership and emotional intelligence. Journal of Graduate Medical Education, 6(1), 21–31. https://doi.org/10.4300/JGME-D-13-00012.1
Moher, D., Shamseer, L., Clarke, M., Ghersi, D., Liberati, A., Petticrew, M., Shekelle, P., Stewart, L. A., & PRISMA-P Group (2015). Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Systematic Reviews, 4(1), Article 1. https://doi.org/10.1186/2046-4053-4-1
Monroe, A. D., & English, A. (2013). Fostering emotional intelligence in medical training: The SELECT program. AMA Journal of Ethics, 13(6), 509-513. https://doi.org/10.1001/virtualmentor.2013.15.6.medu1-1306
Moslehi, M., Samouei, R., Tayebani, T., & Kolahduz, S. (2015). A study of the academic performance of medical students in the comprehensive examination of the basic sciences according to the indices of emotional intelligence and educational status. Journal of Education and Health Promotion, 4, 66. https://doi.org/10.4103/2277-9531.162387
Noughani, F., Bayat, R. M., Ghorbani, Z., & Ramim, T. (2015). Correlation between emotional intelligence and educational consent of students of Tehran University of Medical Students. Tehran University Medical Journal, 73(2), 110-116.
Othman, R., El Othman, R., Hallit, R., Obeid, S., & Hallit, S. (2020). Personality traits, emotional intelligence and decision-making styles in Lebanese universities medical students. BMC Psychology, 8(1), Article 46. https://doi.org/10.1186/s40359-020-00406-4
Ouzzani, M., Hammady, H., Fedorowicz, Z., & Elmagarmid, A. (2016). Rayyan- A web and mobile app for systematic reviews. Systematic Reviews, 5(1), Article 210. https://doi.org/10.1186/s13643-016-0384-4
Petrides, K., & Furnham, A. (2000). On the dimensional structure of emotional intelligence. Personality and Individual Differences, 29(2), 313-320. https://doi.org/10.1016/S0191-8869(99)00195-6
Petrovici, A., & Dobrescu, T. (2014). The role of emotional intelligence in building interpersonal communication skills. Procedia-Social and Behavioral Sciences, 116, 1405-1410. https://doi.org/10.1016/j.sbspro.2014.01.406
Protogerou, C., & Hagger, M. S. (2020). A checklist to assess the quality of survey studies in psychology. Methods in Psychology, 3, 100031. https://doi.org/10.31234/osf.io/uqak8
Ranasinghe, P., Wathurapatha, W. S., Mathangasinghe, Y., & Ponnamperuma, G. (2017). Emotional intelligence, perceived stress and academic performance of Sri Lankan medical undergraduates. BMC Medical Education, 17(1), Article 41. https://doi.org/10.1186/s12909-017-0884-5
Raut, A. V., & Gupta, S. S. (2019). Reflection and peer feedback for augmenting emotional intelligence among undergraduate students: A quasi-experimental study from a rural medical college in central India. Education for Health (Abingdon, England), 32(1), 3–10. https://doi.org/10.4103/efh.EfH_31_17
Reshetnikov, V. A., Tvorogova, N. D., Hersonskiy, I. I., Sokolov, N. A., Petrunin, A. D., & Drobyshev, D. A. (2020). Leadership and emotional intelligence: current trends in public health professionals training. Frontiers in Public Health, 7, 413. https://doi.org/10.3389/fpubh.2019.00413
Schutte, N. S., Malouff, J. M., Hall, L. E., Haggerty, D. J., Cooper, J. T., Golden, C. J., & Dornheim, L. (1998). Development and validation of a measure of emotional intelligence. Personality and Individual Differences, 25(2), 167–177. https://doi.org/10.1016/S0191-8869(98)00001-4
Shi, M., & Du, T. (2020). Associations of emotional intelligence and gratitude with empathy in medical students. BMC Medical Education, 20(1), Article 116. https://doi.org/10.1186/s12909-020-02041-4
Skokou, M., Sakellaropoulos, G., Zairi, N. A., Gourzis, P., & Andreopoulou, O. (2019). An exploratory study of trait emotional intelligence and mental health in freshmen Greek medical students. Current Psychology, 40, 6057–6066. https://doi.org/10.1007/s12144-019-00535-z
Suleman, Q., Hussain, I., Syed, M. A., Parveen, R., Lodhi, I. S., & Mahmood, Z. (2019). Association between emotional intelligence and academic success among undergraduates: A cross-sectional study in KUST, Pakistan. PloS one, 14(7), e0219468. https://doi.org/10.1371/journal.pone.0219468
Sundararajan, S., & Gopichandran, V. (2018). Emotional intelligence among medical students: A mixed methods study from Chennai, India. BMC Medical Education, 18(1), Article 97. https://doi.org/10.1186/s12909-018-1213-3
Tyszkiewicz-Bandur M., Walkiewicz M, Tartas M, Bankiewicz-Nakielska J. (2017). Emotional intelligence, attachment styles and medical education. Family Medicine & Primary Care Review, 19(4), 404–407. https://doi.org/10.5114/fmpcr.2017.70127
University Grants Commission, Sri Lanka. (2022). University Admissions. Retrieved April 21, 2022, from https://www.ugc.ac.lk/index.php?option=com_content&view=article&id=25&Itemid=11&lang=en
Unnikrishnan, B., Darshan, B., Kulkarni, V., Thapar, R., Mithra, P., Kumar, N., Holla, R., Kumar, A., Sriram, R., Nair, N., Juanna, Rai, S., & Najiza, H. (2015). Association of emotional intelligence with academic performance among medical students in South India. Asian Journal of Pharmaceutical and Clinical Research, 8(2), 300-302.
Vasefi, A., Dehghani, M., & Mirzaaghapoor, M. (2018). Emotional intelligence of medical students of Shiraz University of Medical Sciences cross sectional study. Annals of Medicine and Surgery, 32, 26–31. https://doi.org/10.1016/j.amsu.2018.07.005
Völker, J. (2020). An examination of ability emotional intelligence and its relationships with fluid and crystallized abilities in a student sample. Journal of Intelligence, 8(2), 18. https://doi.org/10.3390/jintelligence8020018
Wei, P., & Joseph, A. (2011). Implementing and evaluating the integration of critical thinking into problem based learning in environmental building. Journal for Education in the Built Environment, 6(2), 93-115. https://doi.org/10.11120/jebe.2011.06020093
Wijekoon, C. N., Amaratunge, H., de Silva, Y., Senanayake, S., Jayawardane, P., & Senarath, U. (2017). Emotional intelligence and academic performance of medical undergraduates: A cross-sectional study in a selected university in Sri Lanka. BMC Medical Education, 17(1), Article 176. https://doi.org/10.1186/s12909-017-1018-9
Yee, K. T., Yi, M. S., Aung, K. C., Lwin, M. M., & Myint, W. W. (2018). Emotional intelligence level of year one and two medical students of University Malaysia Sarawak: Association with demographic data. Malaysian Applied Biology, 47(1), 203-208.
*Edussuriya D.H
Department of Forensic Medicine, Faculty of Medicine,
University of Peradeniya, Sri Lanka, 20400
+94711698916
Email: deepthi.edussuriya@med.pdn.ac.lk
Announcements
- Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Volume 9 Number 1 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors. - Volume 8 Number 3 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2021
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2021.
Refer here for the list of recipients. - Most Accessed Article 2021
The Most Accessed Article of 2021 goes to Professional identity formation-oriented mentoring technique as a method to improve self-regulated learning: A mixed-method study.
Congratulations, Assoc/Prof Matsuyama and co-authors. - Best Reviewer Awards 2020
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2020.
Refer here for the list of recipients. - Most Accessed Article 2020
The Most Accessed Article of 2020 goes to Inter-related issues that impact motivation in biomedical sciences graduate education. Congratulations, Dr Chen Zhi Xiong and co-authors. - Scopus
TAPS has been accepted for inclusion in Scopus! - Best Reviewer Awards 2019
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2019.
Refer here for the list of recipients. - Most Accessed Article 2019
The Most Accessed Article of 2019 goes to A two-edged sword: Narrative inquiry into Japanese doctors’ intrinsic motivation. Congratulations,
Professor Hiroshi Nishigori and co-authors!









