The odyssey of medical education in Indonesia
Published online: 2 January, TAPS 2019, 4(1), 4-8
DOI: https://doi.org/10.29060/TAPS.2019-4-1/GP1077
Rita Mustika1,2, Hiroshi Nishigori3, Sjamsuhidajat Ronokusumo1 & Albert Scherpbier4
1Medical Education Department, Faculty of Medicine, Universitas Indonesia, Indonesia; 2The Indonesian Medical Education and Research Institute (IMERI), Faculty of Medicine, Universitas Indonesia, Indonesia; 3Center of Medical Education, Graduate School of Medicine, Kyoto University, Japan; 4Faculty of Health, Medicine, and Life Sciences, Maastricht University, Netherland
Abstract
Medical education in Indonesia has undergone a long journey. It began with the establishment of medical training for native youth in a military hospital in Jakarta during the Dutch colonial period in 1849. Since then, the number of medical schools has increased according to socio-political needs. Currently, there are 83 medical schools, public and private, which generate approximately 8000 graduates per year. The explosion in the number of medical schools challenged quality of medical education. Indeed, several curriculum changes and improvements applied to elevate the quality. Undergraduate program was initially implementing Dutch curriculum, but was then changed into American curriculum. The improvement continued by implementing the first and the second national curriculum. Since 2005 a national level competency-based curriculum (CBC) was carried out for undergraduate programs, while for postgraduate clinical training the CBC began later on. Moreover, Medical Internship Program and the National Competency-based Examination were introduced following the CBC. Nevertheless, some problems with advancement of medical schools were identified, including lack of staff and facilities, existing learning cultures and limitation of experts. Accordingly, many efforts have been made, including enactment of law on medical education and national accreditation. In the future, support from international organizations in terms of financial, consultation, faculty development and accreditation should be optimized. In addition, collaboration with medical education community elsewhere would be beneficial to overcome the challenges and promote the quality of medical education.
Keywords: Medical Schools, Curriculum Changes, Medical Education, Indonesia
Practice Highlights
- Medical education in Indonesia has travelled a long journey since the first medical training program was established in 1849. Currently, there are 83 medical schools and 8,000 annual graduates.
- The implementation of the CBC and the dramatic growth of medical schools have raised concerns about the quality of medical education nationwide.
- Enactment of laws on medical education, accreditation of medical programs, faculty development, and the national competency-based examination have been instituted to improve the quality of medical education.
- Partnerships and collaborations with other medical education communities in and outside the country should be encouraged to continuously improve educational conditions.
I. INTRODUCTION
Indonesia is the largest archipelago, located between Asian and Australian continent, and Indian and Pacific oceans. There are 17.504 islands forming 1.904.569 km2 land area with 257.600.000 inhabitants, making it the fourth most populated country. Most of the population lives in Java. Diverse ethnicities exist, mostly Javanese (40.1%), followed by Sundanese, Malay, Batak, Madurese, Betawi, Minangkabau, Buginese, Bantenese, Banjarese, Balinese, Acehnese, Dayak, Sasak, Chinese and others. Furthermore, 700 languages are spoken and various religions exist, Islam is the religion observed by most of the population (80%), followed by Christianity, Buddhism, Hinduism, and others (Central Bureau Statistics of Indonesia, 2016). Indonesia had been a Dutch colony for 3.5 centuries and declared its independence on August 17th, 1945 after being occupied by Japan for 3.5 years. Long history of colonialism influenced education and health systems in Indonesia.
During the last decade, Indonesia has emerged as a relatively stable country, economically and politically. Moreover, life expectancy reached 71 years (Central Bureau Statistics of Indonesia, 2016). The health system is provided and funded by private and public sectors. In 2014, the government launched a National Health Insurance Program and a plan for universal health coverage in 2019 (Marzuki, 2016). The education system is organized into 3 levels: basic and secondary education in 12 years, followed by higher education. Compulsory age for education is 7-15 years. Higher-education is managed by the Ministry of Research, Technology, and Higher Education. While the basic secondary education is managed by the Ministry of Education and Culture (Marzuki, 2016).
II. MEDICAL EDUCATION DURING THE COLONIAL PERIOD
Medical education in Indonesia began in the Dutch colonial period around 17th century. Since the first medical training initiated in 1849, was established as School of Java Doctor in 1851 to train native youngster to treat smallpox. Dr. W. Bosch, chief of the military-health services was appointed as Head of the school. Students were selected based on ability to write and speak Malay, and the graduate worked as smallpox-caretaker. In 1902, the school transformed into ‘School tot Opleiding van Inlandsche Artsen (School of Medicine for Indigenous Doctors)’ or STOVIA and the Dutch became an academic language. STOVIA only accepted natives and granted title ‘Inlandsch Arts’, meaning doctor from original area. The Nederland Indische Artsen (NIAS) was a second school established in 1913 in Surabaya and accepted students’ from various background. To ensure the ability to speak Dutch, students required to learn Dutch in the first 3 years before they learn medicine for 7 years (Hesselink, 2011).
The medical school as a higher education institute was established in August 16th, 1927 named Geneeskundige Hoogeschool (Higher School of Medicine) to replace STOVIA. The study period was 6 years and the school granted a certificate similar to that of the medical school in the Netherlands ‘Artsen’.
In August 17th, 1945, Indonesia declared its independence. Due to political instability, Geneeskundige Hoogeschool was moved to central Java and NIAS was closed. A year later, Geneeskundige Hoogeschool returned to Jakarta, while in Yogyakarta, a new medical school was established. In the same year, the Government stated that academic activities should be delivered in Bahasa Indonesia (Hesselink, 2011).
III. CURRICULUM CHANGES
By 1950, 3 medical schools existed in Indonesia: Faculty of Medicine Universitas Indonesia (UI) in Jakarta, University of Gadjah Mada (UGM) in Yogyakarta, and faculteit der geneeskunde branch of UI in Surabaya (Hesselink, 2011). During this period, many Dutch physicians who also were lecturers returned to the Netherlands because of inflation, difficulty to teach in Bahasa Indonesia, and hostility toward them. Moreover, the existing schools generated few physicians yearly. The Dutch curriculum was identified as one of the reasons for few graduates. The curriculum emphasized on research-individual study, and the students decided individually when to sit for the examination, resulting only 5-10 students graduated annually. To solve the problem, government opened 3 new schools.
Furthermore, international support was sought to transform the curriculum into American curriculum; the support came from University of California and World Health Organization (WHO). The American curriculum fostered problem solving-critical thinking, study methods were a balance between lectures, laboratory, community, and clerkship. Assessment was in cohort groups. Around 1956, the American curriculum was implemented. Notwithstanding the curriculum succeeding to increase the number of graduates 2-3 times, the shortage of physicians in certain areas persisted, because the graduates still prefer to work in urban areas. Furthermore, the curriculum evaluation revealed that most schools lacked faculty and facilities to continuously implement it. Consequently, in 1970 medical schools returned to the Dutch curriculum (Hesselink, 2011). Other effort was the policy of requiring graduates to serve as rural physicians for 3-5 years before accepting permanent post. With support from WHO, the curriculum was changed into community-oriented curriculum to prepare the graduates to the rural (Indonesian Consortium of Health Sciences, 2013).
In 1984, finally Indonesia developed its own national curriculum, named KIPDI I. It was a community-oriented curriculum and was implemented nationwide. This was followed by KIPDI II, a content- and discipline-based curriculum in 1995. In 2005, influenced by a changing paradigm in medical education globally, from a structure- and process-based to a competency-based curriculum, Indonesia introduced a competency-based curriculum (CBC). At the same time, the Indonesia Medical Council was established with tasks to manage the registration of medical doctors and dentists, authorize medical education standards, and maintain quality of medical practice (Indonesian Consortium of Health Sciences, 2013).
IV. THE GROWTH OF MEDICAL SCHOOLS IN INDONESIA
Medical schools were mushrooming since 1960. Five public and 1 private medical schools in 1960, became 9 public and 10 private medical schools in 1970. The number continuously rose, and in 2005, there were 24 public and 27 private schools. Moreover, in 2010, there was a policy that every island should establish at least one medical school, resulting in 6 public and 14 private new medical schools (Indonesian Consortium of Health Sciences, 2013). Currently, 71 medical schools have already been accredited by the National Accreditation Body for Higher Education (BAN-PT).
In 2016, there were 12 newly established, but not yet accredited, medical schools. In total, presently there are 83 medical schools in Indonesia. Figure 1 shows the growth of medical schools in Indonesia (Indonesian Medical Council, 2017).
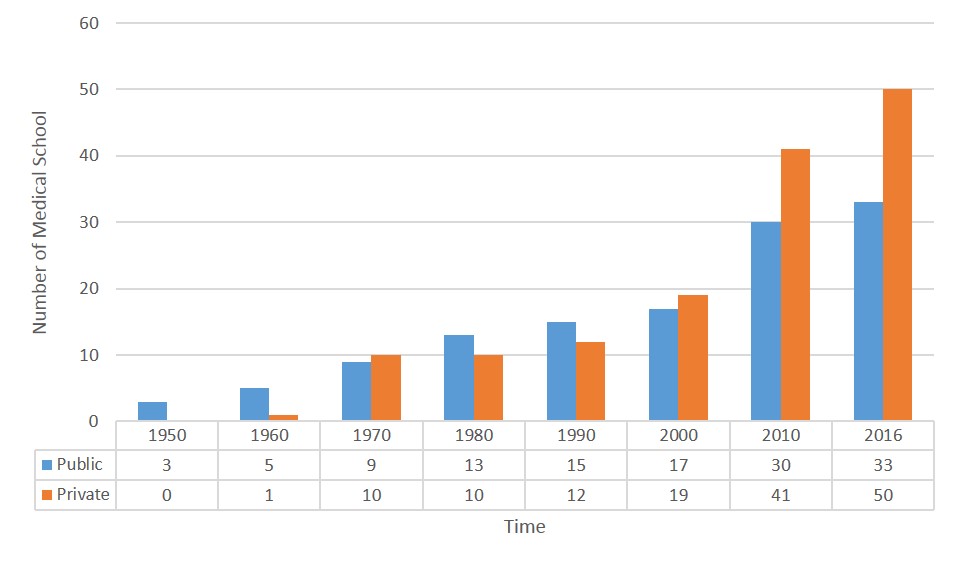
Figure 1. The growth of medical school over time
V. CURRENT SITUATION
A. Undergraduate Medical Education
Medical schools in Indonesia are part of a university, public or private. Besides organizing a regular program, some schools collaborate with schools abroad and offer an International Class Program. The selection process of public medical schools is based on the high school performance or a written test (national and independent written test). Some medical schools add Multiple Mini Interview (MMI) or psychometric test for selection. The private schools organize their own selection. Only high school graduates from science track could apply for selection. Study period of the undergraduate program is at least 3,5 years of pre-clinical studies, followed by a 2-year clinical phase. Strategy for implementing the CBC mandated the medical school to implement at least 50% vertical and horizontal integration in the curriculum. Most medical schools implemented their curriculum based on organ systems in modules. Specific skills such as procedural skills, research, and professional development are integrated within curriculum. Early clinical exposure is achieved by using clinical scenarios for triggering discussion. Mostly community-oriented education is implemented from the beginning of the program (Indonesian Medical Council, 2017).
B. Medical Internship Program
After passing the national examination, since 2010, graduates are required to attend a 1-year medical internship program before they could work independently (Indonesian Medical Council, 2017). The Indonesian Medical Internship program is managed by a committee established in 2009, comprising all stake holders, under the Ministry of Health of the Republic of Indonesia. The graduates were appointed to a healthcare institute close to their medical schools’ location. During internship, an intern works in a primary health care centre and a local hospital, under the supervision of a trained senior physician. Most of the internship is located in the rural areas, but since 2015, Jakarta – the capital – also welcomed interns (Indonesian Medical Council, 2017). The law on medical education mandated a 2-year, primary care physician program for a post-intern to become a primary care physician. Currently, this program is still in preparation.
C. Postgraduate clinical training programme and Continuing Medical Education/ Continuing Professional Development (CME/CPD)
Postgraduate clinical training program started after the independence. Students were recruited based on their undergraduate performance. In 1979, the government established a Consortium of Health Sciences (CHS) to structure the program and produce a general guidelines. Since 2013, the programs are managed by medical schools in coordination with specialist association. Currently, there are 36 specialist associations within 17 medical schools. Quality is assured with an accreditation process by neutral organizations at the national level. In general, the requirement to join the programs is completing internship, but some specialties required additional 1-2 years of clinical experience. The selection included a written test, an English proficiency test, an interview (multiple mini interview [MMI] or regular interview), and a psychometric test. Most programs are implementing a CBC-modular approach (Indonesian Consortium of Health Sciences, 2013).
Lifelong learning and the re-certification process required physicians to join CME/CPD programs. The providers of CME/CPD are The Indonesian Medical Association, the Specialist Association, the medical schools, and the Ministry of Health. Activities vary from academic conferences, seminars, workshops, to e-learning, journal or magazine. Most specialist organizations organize an annual academic conference at the regional, national, and international level. Quality is monitored by the Indonesian Medical Doctor Association (Indonesian Medical Council, 2017).
VI. MAJOR CHALLENGES AND FUTURE PERSPECTIVE
The Implementation of CBC requires many adjustments. A WHO consultant guided the initiation, and some international institutions were supporting financially to develop the system. Despite the support, diverse locations and infrastructure make medical schools vary in implementing CBC. Moreover, students and teachers are struggling to adapt to the new teaching-learning culture. This is aggravated by the lack of medical teachers in the schools.
To support the CBC implementation, the Government paired new schools with the more established ones. The support was in terms of curriculum, faculty development, and resources. Alternative active learning methods were introduced to suit the limited resources. However, the implementation at the national level needs continuous monitoring.
The increasing number of schools not only increases the number of graduates, but also raises concerns about quality. The admission process could be less competitive and problematic, and the availability of teaching hospitals could also be a problem. The Government has set a quota for admission based on the level of accreditation to address this. The other effort is the Government imposing standards and national accreditation guidelines, benchmarked to the Global Standards of Medical Education from World Federation of Medical Education (WFME) (Indonesian Medical Council, 2012). All programs have to undergo a national accreditation processes every 5 years. Medical schools are expected to identify their weaknesses and seek continuous improvement through the accreditation process. Meanwhile, only 20 out of 71 (28%) accredited undergraduate programs were granted ‘A’, the highest level of accreditation grade (Indonesian Medical Council, 2017).
Currently, more medical schools participate in medical education associations and research collaborations. For example, The South East Asia Regional Association for Medical Education (SEARAME) and The Association for Medical Education in Europe (AMEE). Some medical schools organized national medical education meetings annually and invite international speakers. UI organized Jakarta Meeting on Medical Education (JAKMED) conference annually since 2008.
Medical education in Indonesia has come through a long impressive journey. Progressing tremendously over time. The importance of high quality of medical education has been acknowledged by the enactment of the new Law on Medical Education and the support from all stakeholders. Hence, the medical education community should focus on improving quality of education. The Government needs to continuously support in terms of developing regulations for medical education, career paths for medical-clinical teachers, and allocate standard facilities. Furthermore, partnership and collaboration within and outside the country has been proven to be worthwhile, facilitating learning from each other and effectively solving problems. Indonesia medical education community needs to enhance participation in promoting high quality medical education globally.
Note on Contributors
Rita Mustika is a senior lecturer at Department of Medical Education, Faculty of Medicine, Universitas Indonesia and Coordinator of Collaboration in Medical Education at The Indonesian Medical Education and Research Institute (IMERI).
Hiroshi Nishigori is an Associate Professor at the Centre for Medical Education, Graduate School of Medicine, Kyoto University, Japan.
Sjamsuhidajat Ronokusumo is a former Chair of Indonesian Consortium of Health Sciences and Professor emeritus at Department of Medical Education, Faculty of Medicine, Universitas Indonesia.
Albert Scherpbier is a Professor of Quality Promotion in Medical Education and Dean of the Faculty of Health, Medicine, and Life Sciences of Maastricht University, Netherlands.
Acknowledgements
The authors wish to express sincere appreciation to Professor Agus Purwadianto for a fruitful discussion during the finalization of this manuscript.
Funding
This manuscript was initiated during fellowship program at the centre for medical education, Kyoto University, funded by the Medical Education and Research Institute (IMERI).
Declaration of Interest
All authors confirm that they do not have conflict of interest in connection with this manuscript including financial, consultant, institutional and other relationships that might lead to bias or conflict of interest.
References
Central Bureau Statistics of Indonesia. (2016). Statistik Indonesian 2016 [Statistical yearbook of Indonesia], 113–133. Indonesia: BPS-Statistics Indonesia.
Hesselink, L. (2011). Healers on the colonial market; Native doctors and midwives in the Dutch East Indies. Leiden – Boston: Brill. Retrieved from http://www.oapen.org/record/400271.
Indonesian Consortium of Health Sciences. (2013). Perkembangan pendidikan kedokteran di Indonesia. Sistem Pendidikan Kedokteran di Indonesia menuju 2045 [Development of medical education in Indonesia. Medical Education System in Indonesia Toward 2045]. Indonesia: Indonesian Consortium of Health Sciences.
Indonesian Medical Council. (2017). Profil Konsil Kedokteran Indonesia [Profile of Indonesia Medical Council]. Retrieved October 21, 2017, from http://www.kki.go.id/index.php/subMenu/983.
Marzuki, P. (2016). Case study 24.5: Establishing a quality assurance system of medical education in Indonesia. In K. Abdurahman, S. Mennin, R. Harden, & C. Kennedy (1st Ed.), Routledge International Handbook of Medical Education (pp. 340–342). London: Routledge.
*Rita Mustika, MD, M. Epid
Medical Education Department,
Faculty of Jl. Salemba Raya no 6
Jakarta Pusat, Indonesia
Telephone/fax: +62218901814
Email Address: ritakobe@gmail.com
Announcements
- Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Volume 9 Number 1 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors. - Volume 8 Number 3 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2021
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2021.
Refer here for the list of recipients. - Most Accessed Article 2021
The Most Accessed Article of 2021 goes to Professional identity formation-oriented mentoring technique as a method to improve self-regulated learning: A mixed-method study.
Congratulations, Assoc/Prof Matsuyama and co-authors. - Best Reviewer Awards 2020
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2020.
Refer here for the list of recipients. - Most Accessed Article 2020
The Most Accessed Article of 2020 goes to Inter-related issues that impact motivation in biomedical sciences graduate education. Congratulations, Dr Chen Zhi Xiong and co-authors. - Scopus
TAPS has been accepted for inclusion in Scopus! - Best Reviewer Awards 2019
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2019.
Refer here for the list of recipients. - Most Accessed Article 2019
The Most Accessed Article of 2019 goes to A two-edged sword: Narrative inquiry into Japanese doctors’ intrinsic motivation. Congratulations,
Professor Hiroshi Nishigori and co-authors!









