Reflections on an interdisciplinary curriculum and pedagogical approaches in a public health course
Published online: 5 May, TAPS 2020, 5(2), 54-56
https://doi.org/10.29060/TAPS.2020-5-2/CS2150
Julian Azfar & Rayner Kay Jin Tan
Saw Swee Hock School of Public Health, National University of Singapore, Singapore
I. INTRODUCTION
The notion of interdisciplinary health(care) education is an emerging, though not novel concept (Allen, Penn, & Nora, 2006). The module Social Determinants of Health was introduced in the Saw Swee Hock School of Public Health in 2018. The module covered important foundational concepts in the study of social determinants of health and explored examples of such determinants over 13 weeks. The module adopted an interdisciplinary approach to public health, drawing from biomedical, psychological and sociocultural perspectives informed by both the natural and social science disciplines. Coursework took the form of student-led seminars, opinion editorial (Op-Ed) and reflective essays, and a fieldwork project involving a chosen group in the community. While the adoption of such an interdisciplinary approach, or the use of the chosen pedagogical approaches are not novel, we present our reflections on the implementation of a novel, interdisciplinary course in public health for undergraduates in Singapore who do not have prior knowledge or expertise in the subject area.
II. AN INTERDISCIPLINARY FRAMEWORK
Past literature on interdisciplinary pedagogies have highlighted the importance of introducing interdisciplinary subjects in the curriculum, drawing on students’ varying backgrounds or disciplines in collaborative learning, and the focus on problems or issues instead of concepts (Friedow, Blankenship, Green, & Stroup, 2012), which have been incorporated in the present module. For example, module content was divided into three sections: “Environments and Communities”, “Globalisation and Work” and “Culture and Being”, providing opportunities for the exploration of public health issues from diverse perspectives. In addition, the focus on student-led seminars and essays, which emphasised the application of concepts to case studies or real-world contexts, helped further students’ understanding of the social determinants of health.
III. ASSESSMENT AND PEDAGOGICAL APPROACHES
The module’s teaching and learning approach was anchored in three main principles – constructivism, critical thinking and questioning, and experiential learning.
A. Constructivism
Constructivism, as a learning theory, posits that individuals engage in meaning-making through interactions between new and their pre-existing knowledge (Piaget, 1971). Each lesson began with a student seminar exploring a guiding question related to the week’s topic, followed by a lecture. Students were given an opportunity to construct their own understandings of the topics based on the assigned readings and compare these interpretations to those of the teacher. In addition, as part of individual written assessment, the Op-Ed and reflective essays further built on the constructivist approach by enabling students to formulate and defend their own judgments in response to other author’s arguments in the Op-Ed essay, as well as synthesising content meaningfully for the reflective essay.
B. Experiential Learning
Experiential learning, which emphasises the role of engagement with real-life experiences and consequences for learning (Kolb, 1984), was also a key feature of the course. To encourage preliminary insights into the necessity for experiential learning in the understanding of social determinants of health, guest speakers such as academics, non-governmental organisation representatives, researchers and even Traditional Chinese Medicine practitioners provided students with first-hand insight into their work and the social contexts of health in Singapore and beyond. The end-of-semester fieldwork project was also an opportunity for students to apply concepts in a relevant way by exploring how social determinants implicated health outcomes for a chosen community in Singapore.
C. Critical Thinking and Questioning
Critical thinking and questioning was an approach that undergirded the conduct of lessons, as well as the different modes of assessment in the module. Bloom’s Taxonomy (1956), for example, was used to scaffold questioning in teacher-led discussions and student seminar presentations. Particularly, in presenting their fieldwork projects, students were also assessed on the types of questions they fielded to presenting groups and the ability to defend their own arguments. Students were tasked with the responsibility of driving the process of class discussions, with the teacher only playing the role of a facilitator.
IV. REFLECTIONS ON COURSE EFFECTIVENESS
Both quantitative and qualitative feedback were obtained from students following the end of the course. Of the 73 students who had taken the course and were invited to provide feedback, a total of 32 students responded (43.8% response rate). Quantitative feedback focused largely on the effectiveness of the course instructors and did not yield rich insights into the effectiveness of the course relative to the qualitative feedback, and thus are omitted here. Qualitatively, students were asked to provide feedback on what they felt were positive aspects of learning in the course. Thematic analysis of the qualitative feedback generated three specific areas where students felt they were positively impacted; firstly, opportunities for creative thinking via assessment methods were favourable; secondly, real-world application of content helped to sharpen knowledge, skills, values; and lastly, flexibility in assessment and choice of topics engaged students more. A summary of these themes and corresponding quotes may be found in Table 1.
|
Themes |
Corresponding quotes |
|
Opportunities for creative thinking via assessment methods were favourable |
“Creativity as a point of marking for presentations, I feel that it stretched our brains and allowed me to think out of the box.” |
|
Real-world application of content helped to sharpen knowledge, skills, values |
“Raised my social awareness of many issues… applicable to our daily lives.”
“Something about health we can share with family and friends…” |
|
Flexibility in assessment and choice of topics engaged students more |
“Seminar-style… presentations were interesting…”
“The module is interesting because it allowed me to explore various aspects of health.” |
Table 1. Themes and corresponding quotes from qualitative responses as positive feedback on design, pedagogy and assessment of the course
V. CONCLUSION
Social Determinants of Health is establishing itself as a popular course amongst undergraduates from different backgrounds. This stems from the constructivist approach that has informed course design, as well as opportunities for critical thinking and questioning, and authentic experiences in teaching, learning and assessment. It is envisioned that by making more disciplinary connections and scaffolding critical thinking and communication throughout the module, the course will continue to enrich the learning experiences of undergraduates from an even more diverse range of specialisations.
Notes on Contributors
Julian Azfar is currently an instructor at the Saw Swee Hock School of Public Health. He teaches courses related to the health humanities and is interested in using interdisciplinary curricula to promote critical thinking, perspective-taking and an appreciation of diversity in his courses.
Rayner Kay Jin Tan is a PhD student at the Saw Swee Hock School of Public Health. He has assisted in the planning and teaching of Social Determinants of Health and has been a key facilitator of learning activities throughout the entire duration of the course.
Acknowledgements
The authors would like to thank all students, guest lecturers, and coordinators who have contributed to the design and management of the course. The authors would also like to thank the staff at Saw Swee Hock School of Public Health for their support.
Funding
There is no funder for this paper.
Declaration of Interest
The authors confirm that the manuscript is original work of authors which has not been previously published or under review with another journal. The authors confirm that all research meets legal and ethical guidelines and that all possible conflict of interest for this paper has been explicitly stated even if there is none. The authors are not using third-party material that requires formal permission.
References
Allen, D. D., Penn, M. A., & Nora, L. M. (2006). Interdisciplinary healthcare education: Fact or fiction? American Journal of Pharmaceutical Education, 70(2), 39. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1636929/
Bloom, B. S. (1956). Bloom’s taxonomy of educational objectives. New York, NY: Longman.
Friedow, A. J., Blankenship, E. E., Green, J. L., & Stroup, W. W. (2012). Learning interdisciplinary pedagogies. Pedagogy: Critical Approaches to Teaching Literature, Language, Composition, and Culture, 12(3), 405-424. https://doi.org/10.1215/15314200-1625235
Kolb, D. A. (1984). Experiential learning: Experience as the source of learning and development. Englewood Cliffs, NJ: Prentice-Hall.
Piaget, J. (1971). Psychology and epistemology: Towards a theory of knowledge. New York, NY: Grossman.
*Julian Azfar
Saw Swee Hock School of Public Health,
National University of Singapore,
12 Science Drive 2, #10-01,
Singapore 117549
Email: ephjam@nus.edu.sg
Published online: 5 May, TAPS 2020, 5(2), 1-4
https://doi.org/10.29060/TAPS.2020-5-2/GP1084
Colm Bergin1 & Mary Horgan2,3
1School of Medicine Trinity College Dublin, Ireland; 2Royal College of Physicians of Ireland, Ireland; 3School of Medicine, University College Cork, Ireland
Abstract
Medical education and training has evolved over the centuries. Ireland has a long history of leading on aspects of training that remain relevant today, focussing on the apprenticeship model coupled with a robust modern medical education framework. The practice of medicine is changing rapidly driven by expanding knowledge, advances in technology and use of artificial intelligence, demographic shifts and the expectations of patients and society. Medical training and education need to adapt to ensure that our current knowledge and future medical workforce is prepared for modern-day patient-centric practice. Ireland has emerged as a world leader in medical device technology, pharmaceutical research and development and social media technology support which offer the opportunity for the future of medical training. Knowledge, emotional intelligence, critical thinking, compassion, resilience and leadership are key attributes to which we as a profession aspire. There is an opportunity to leverage Ireland’s global position in technology and finance to train our modern-day medical workforce whilst retaining the attributes of the compassionate practice of the art of medicine. This paper explores the past, present and future of medical education and training in Ireland.
Practice Highlights
- Ireland has a history of leading in medical education.
- Training focusses on the blended apprenticeship model.
- Ireland is now a world leader in medical device technology, pharmaceutical research and social media technology.
- Agility, diversity and flexibility are embedded in the modern day medical training model.
- Compassion and communication remain pivotal to the practice of medicine.
I. INTRODUCTION
Ireland is a small island on the westerly fringe of Europe separated from Great Britain by the Irish Sea and with a population size similar to Singapore. Although Ireland is a small nation, its global impact is large due to the high value we, as a nation, put in educating our population. Ireland now ranks fourth in the world in the UN’s Human Development Index, a widely accepted measure of living conditions or quality of life across the globe. Ireland is ranked second to Singapore in reading performance in Organisation for Economic Co-operation and Development (OECD, 2019) rankings. The enrolment of 17-year-olds in Ireland’s secondary education system is 99.3%, with well over the OECD average continuing on to tertiary level education. Ireland is a hub for many major pharmaceutical, medical devices and technology companies which has allowed growth in research. Partnerships between industry and Irish universities facilitate innovation and research in the medical and life sciences sectors. There are six medical schools in the Republic of Ireland, one of which dates from the 17th century and four from the 19th century. Ireland is justly proud of the history and quality of its medical education. This article outlines the past, present and future of undergraduate and postgraduate education in Ireland.
II. THE PAST
Ireland has a long history of being at the forefront of medical education. Many of the Presidents of the Royal College of Physicians of Ireland (RCPI), which was founded in 1654, have played eminent roles in innovation in medical education since the 17th century (Coakley, 1992). Medical education started in Ireland with the appointment of John Stearne as the first professor of medicine at Trinity College in the 1650s. The School of Anatomy in Trinity College did not open until 1711; however, following its opening, the medical school flourished.
Worldwide, doctors and medical students associate the name of Robert Graves with the disease of the thyroid gland however few are aware of the key role he played in the development of bedside teaching. During the early 19th century, Graves introduced two elements of radical change in medical education: the distribution of the care of patients to senior medical students and the changing of teaching from the lecture room to the bedside of the patient. These fundamental changes in medical education developed the skill of observation and ensured that errors in clinical judgement were corrected on the spot (Coakley, 1992). Grave’s method of teaching was adopted in the English-speaking world and continues to this day. Graves constantly exhorted students to spend time on the wards gaining practical experience. Graves appreciated the importance of what is now called continuing professional development by stating that “if a teacher is to maintain the credibility of his students he must keep up with modern advances” (Coakley, 1992, p. 91).
While Graves and his colleague Dr Stokes (the condition Cheyne Stokes respiration bears his name) “were not the first to make use of beside teaching, they did so consistently and so successfully that it was adopted by clinical teachers elsewhere” (p. 94) according to Professor Daniel Reisman writing in the Medical History of the College of Physicians of Philadelphia in 1921 (Coakley, 1992).
In the late 19th century, the first generation of women doctors found the Irish medical hierarchy to be unusually open-minded with regard to the question of women’s admission in contrast to the policy in Great Britain. The Royal College of Physicians of Ireland (previously known as King and Queen’s College of Physicians in Ireland) was the first institution in the British Isles to admit women who had taken their studies abroad to their licentiate examinations in 1877 thereby allowing the first registration of female doctors in Great Britain and Ireland. Sophia Jex Blake, a leading campaigner for women’s admission to the medical profession from the 1860s, remarked that this decision was “the turning point” in the societal shift to gender equality in medicine as a profession.
III. THE PRESENT
A. Undergraduate Medical Education
Medical education in Ireland is provided by six medical schools. In 2006, the Irish government commissioned a report “Medical Education in Ireland: A New Direction”, the Fottrell report (Working Group on Undergraduate Medical Education and Training, 2006), which addressed core issues such as funding, selection criteria for medical school entry and intake numbers, curriculum reform, clinical training and oversight of undergraduate education. The implementation of the report resulted in, 1) expanded and new access routes to medical school with the addition of Graduate Entry Medical programmes in four of the schools, 2) curricular reform with outcomes linked to objectives, content, delivery methodologies, and assessment thereby expanding the methods by which education is delivered in line with international standards, 3) increased funding for faculty and infrastructure, 4) expansion of teaching to primary care facilities and, 5) accreditation of all clinical sites in partnership with Ireland’s national health service, the Health Service Executive (HSE).
Admission to medical school for Irish students is highly competitive, with ten applicants for each place. For school leavers, places are awarded on the basis of a combination of marks achieved in their high school exit examination and the recently introduced Health Professions’ Aptitude Test Ireland. Graduate entry students must achieve at a minimum upper second class honours primary degree and are then admitted on the basis of performance in the Graduate Medical School Admissions Test. Places at Irish medical schools are highly sought after by international students because of the international reputation for high-quality medical education in Ireland, and the safe, welcoming nature of the country. Students apply through international agents and are offered places based on academic performance, interviews and personal statements.
The Medical Council of Ireland regulates undergraduate medical education in accordance with the World Federation for Medical Education Standards. Irish medical schools have long been recognised for their strengths in providing an excellent grounding in foundational sciences, coupled with high-quality clinical teaching, experiential training and an emphasis on professionalism. Recent decades have seen innovation in the areas of inter-professional learning and team-based practice, research and innovation skills, the humanities in medical education, simulation and other forms of technology-enhanced learning. The universities have established academic units specifically dedicated to medical education and offer masters level qualifications in medical education.
Undergraduate medical education in Ireland shares many challenges with other jurisdictions including the continued provision of high-quality clinical learning environments for placements, supporting students’ health and wellbeing, and ensuring that graduates are well prepared for modern-day practice. Irish medical schools have retained the formal observed examination of bedside practice and communication as a significant component of the final year medical examinations.
International partnerships to support medical student exchange programmes are underpinned by memoranda of understanding. These facilitate high-quality research and clinical electives to enhance the student experience and prepare them for future practice in differing healthcare settings.
B. Postgraduate Medical Education
The governance of postgraduate education and training is under the remit of the Royal Colleges which are funded by the HSE to provide training on clinical sites. There are 13 postgraduate training bodies across all domains of practice. The RCPI is the largest training body with 1500 trainees in the specialities of medicine: paediatrics, obstetrics and pathology. Following a year’s internship, trainees enter two years of general professional training (residency) followed by a five-year fellowship of speciality training during which many trainees undertake formal research training to the level of MD/PhD. Partnership between the universities and the postgraduate training bodies has led to the establishment of structured training programmes to train academic clinicians such as the Irish Clinical Academic Training Programme.
The tradition of Irish doctors doing part of their training overseas is a well-established practice. Since the 1950s, the well-educated Irish diaspora have emigrated to develop professionally and return to Ireland to contribute their new knowledge and skills to society. Specifically, the Irish healthcare system has benefitted greatly from these medical graduates returning to Ireland bringing not only the expertise of their particular medical speciality but also the benefits gained from the experiences of working in different health systems.
In recent years, the Irish government published two reports on postgraduate medical education and training: “Preparing Ireland’s Doctors to Meet the Health Needs of the 21st Century”, Buttimer report (Postgraduate Medical Education and Training Group, 2006) and “Strategic Review of Medical Training and Career Structures”, McCraith report (Department of Health, 2014). These reports address the global challenges of doctor recruitment and retention, emerging healthcare needs of the population and the need for medical training and practice to incorporate use of modern-day technologies and fiscal responsibility and stewardship.
IV. THE FUTURE
There are three key elements to consider in the future planning of medical education and training: the modern-day workforce, the patient and the workplace environment. The increased financial challenge from rising healthcare costs is a central consideration for the future of medical education and training. Medical training needs to provide diversity in who we train and what we train doctors for, flexibility in training and work practice, and agility in how we respond to new challenges. We need models of collaboration with the sharing of learning material across borders, avoiding “reinventing the wheel” in a resource-scarce world.
The modern-day workforce is the most educated of all generations. They embrace technology and look for opportunities to innovate. They want a work-life balance that ensures job satisfaction and avoids burnout. The “one size fits all” model of a doctor needs to be “retired” to allow smart young medical professionals to adapt to the needs of the modern-day work patient and work environment. The future will require doctors to leave their comfort zones and work with other professionals outside healthcare. To achieve this, medical training will need to embrace innovation and entrepreneurship, providing doctors with experiential learning in the disciplines of business, science, engineering and law. Ireland is well-positioned to leverage on experiential learning and internships with global pharmaceutical, medical technology and medical device companies, as most of the world’s major companies are based in the country. Programmes, such as Bioinnovate Ireland, establish teams of doctors, other healthcare professionals, engineers and business school graduates who partner to identify innovative solutions to healthcare delivery. Health Innovation Hub Ireland brings innovation in and out of the health service and is a partnership between the medical schools and teaching hospitals and is funded by the Irish government through Enterprise Ireland. Initiatives such as this offer a new funding structure through which these companies sponsor applicants. The output from such partnerships will ensure that doctors become skilled innovators who can provide leadership in tackling global health issues such as disparity and inequality in healthcare access and healthcare provision, embedded in a sustainable financial model.
The new generation of doctors wants the option to practice differently. Modern-day society and individuals have increasing expectations of the healthcare system and their doctors. Doctors need to be effective in managing these expectations through knowledge exchange and communication. The modern-day practice is impacted by external influences, some predictable such as demographic shifts and workforce and resource scarcity; others unpredictable, such as new technological and therapeutic breakthroughs and shifts in global economic power. What is certain is a finite healthcare budget, so cost-consciousness must be built into our training programmes. What is uncertain is how we can deal with the unpredicted nature of quality healthcare provision.
Notes on Contributors
Professor Colm Bergin is a consultant physician in Infectious Diseases at St James’ Hospital and a clinical professor of medicine at Trinity College Dublin, Ireland. He is Director of Training Site accreditation RCPI and Censor in RCPI. He is the former director of Wellcome HRB Clinical Research Facility, Trinity College Dublin
Professor Mary Horgan is the president of the Royal College of Physicians of Ireland and former Dean of the School of Medicine, University College Cork. She is a consultant physician in Infectious Diseases at Cork and has served on numerous government-appointed boards and Governor of University Board.
Acknowledgements
Professor Tim O’Brien National University of Ireland Galway (NUIG), Dr Carmel Malone NUIG, Professor Michael Keane University College Dublin (UCD), Professor Paula O’Leary University College Cork (UCC), Dr Deirdre Bennett UCC and Dr Roisin Craven Royal College of Physicians of Ireland (RCPI).
Funding
There is no funding involved for this paper.
Declaration of Interest
The authors declare no conflict of interest.
References
Coakley, D. (1992). Irish masters of medicine. Dublin, Ireland: Town House.
Department of Health. (2014). Strategic review of medical training and career structure: Report on medical career structures and pathways following completion of specialist training. Retrieved from https://www.lenus.ie/handle/10147/317460
Organisation for Economic Co-operation and Development. (2019). Population [Indicator]. https://doi.org/10.1787/d434f82b-en
Postgraduate Medical Education and Training Group. (2006). Preparing Ireland’s doctors to meet the health needs of the 21st century. Retrieved from https://www.lenus.ie/handle/10147/42920
Working Group on Undergraduate Medical Education and Training. (2006). Medical education in Ireland: A new direction. Retrieved from https://www.lenus.ie/handle/10147/43350
*Mary Horgan
Royal College of Physicians of Ireland,
19 South Frederick Street, Dublin 2, Ireland
Tel: +35 32149 01596
Email: m.horgan@ucc.ie
Published online: 5 May, TAPS 2020, 5(2), 51-53
https://doi.org/10.29060/TAPS.2020-5-2/PV2171
Heng-Wai Yuen1,2,3 & Abhilash Balakrishnan2,3,4
1Department of Otolaryngology-Head & Neck Surgery, Changi General Hospital, Singapore; 2Duke-NUS Medical School, Singapore; 3National University of Singapore, Yong Loo Lin School of Medicine, Singapore; 4Department of Otolaryngology, Singapore General Hospital, Singapore
I. INTRODUCTION
Big data (BD) involves aggregating and melding large and heterogeneous datasets, allowing searches and cross-referencing, and deriving insights and meaning from them. It has tremendous potential for application in medical education (ME) where the massive amounts of data that are generated and collected about learners, their learning, and the organisation of their learning can be analysed and interpreted to provide meaning and insights into various aspects of ME. This article briefly introduces BD, potential areas of application, and highlights the pitfalls and challenges surrounding the use of BD in ME (BDME) from the authors’ perspectives.
II. BIG DATA IN MEDICAL EDUCATION (BDME)
The concept of BD has its origins in commercial industries, and also academic and technical disciplines (e.g., astronomy and genomics) where enormous amounts of complex data and information are routinely collected, managed and analysed (Ellaway, Pusic, Galbraith, & Cameron, 2014; Schneeweiss, 2014). This information possesses characteristics denoted by the four Vs: high Volume, Variety, Velocity, and Veracity (validity); conventional database software tools are unable to fully capture, store, process, or analyse them (Ellaway et al., 2014). BD is relatively new in clinical medicine and applying BDME has been slow and limited (Cook, Andriole, Durning, Roberts, & Triola, 2010; Ellaway et al., 2014) Nonetheless, in the last few years, there are increased efforts to apply BD to ME (Chahine et al., 2018; Ellaway et al., 2014). To this end, ME is well suited for BD application as a massive volume of complex data is generated and collected constantly from different programs and educational institutions, and from multiple sources, both structured and unstructured: e.g., electronic medical records, assessment results and test scores, evaluation and feedback information, as well as curriculum and program evaluation (Chahine, et al., 2018; Cook et al., 2010). By harnessing the power of BDME, information and data can be aggregated, integrated, and analysed, then interpreted and acted on if necessary (Ellaway et al., 2014; Schneeweiss, 2014).
III. POTENTIAL APPLICATIONS OF BDME
The potential of BDME includes both practical (e.g., program and curriculum assessment and evaluation) and research applications. Depending on the purpose and/or research question, the data mining may be on a broad, systems-level or a personalised small-scale basis. BDME application organises and crystallises the data to enable a better understanding of and insight into what happened, and what is currently happening. This may occur through various different ways of analyses including prospective longitudinal analysis, trend discovery, pattern recognition and predictive analytics. Hence, predictions or extrapolations might be made in regards to what may yet happen in curriculum, programs and educational practices (Chahine et al., 2018; Cook et al., 2010; Ellaway et al., 2014).
For instance, BDME can facilitate decision-making in undergraduate ME, e.g., entry selection of medical students, or readiness of a medical student to graduate. In postgraduate ME, BDME can provide insights into data on learners’ experience and exposure, feedback information, as well as assessment data within and across programs (Chahine et al., 2018; Ellaway et al., 2014). This allows personalised feedback and individualised learning plans (Chahine et al., 2018), and facilitates the implementation of entrustable professional activities (EPA). Learning gaps and teaching lapses can also be identified to support improvement or changes to certain practices or contents. Applying BDME on these educational and other data (such as demographics, admission criteria or educational practices) in a longitudinal and cross-sectional manner allows benchmarking and accountability across different cohorts, programs, and institutions. This is vital for continuous quality assurance and improvement of ME practices (Chahine et al., 2018; Cook et al., 2010; Ellaway et al., 2014), or for evaluation of upstream policies (Chahine et al., 2018; Schneeweiss, 2014). These same processes can also be performed across countries to inform ME from international or cross-cultural perspectives.
Another potential application of BDME is to investigate the (hitherto assumed) link between ME and patient care. Drawing on combined data from educational and clinical information repositories (e.g., correlating patient outcomes from hospital and clinic health information systems with different models of educations within and across institutions), one would be able to evaluate if, and to what extent, educational practices translate into improved health care outcomes for patient and society (Chahine et al., 2018). One example is the Jefferson Longitudinal Study of Medical Education (Callahan, Hojat, Veloski, Erdmann, & Gonnella, 2010) whereby data on 8000 students who were tracked over 40 years showed that MCAT examination performance is a valid predictor of medical school and residency performance. This and other studies confirmed the feasibility and utility of applying BD to inform current medical educational practices, and to bridge the gap between pedagogical theory and practice. Further, by enabling a longitudinal view of physicians’ progression and development through their education, and the career choices made, BDME can provide information and evidence to facilitate recommendations for important strategic policies and decisions, e.g., manpower planning or speciality development. These are subjects of interest for policy-makers, regulatory authorities, medical educators and researchers.
IV. POTENTIAL OBSTACLES AND PITFALLS
Whilst there are many potential fruitful applications of BDME, some challenges and issues must be critically addressed before the widespread adoption of BD into mainstream ME practice.
Data fragmentation, so common in healthcare systems, is a major obstacle to the widespread use of BDME (Ellaway et al., 2014; Schneeweiss, 2014). For a start, electronic health or medical records (EMR) are frequently incompatible and heterogeneous across hospital systems that store the data (Chahine et al., 2018; Ellaway et al., 2014). Practice standards and vocabulary are also not standardised. Also, healthcare systems are not required (or willing) to exchange and share data with each other. In addition, organisational policies regarding security and confidentiality limit data accessibility (Chahine et al., 2018; Ellaway et al., 2014). Further, there are ethical and medicolegal considerations. For instance, most of the patient data captured on EMR was not originally intended for education purposes, and does not include informed consent in this respect. Even if the data can be anonymised with identifiers removed, questions remain on what data is collected, how the data is stored and protected, how it is used and shared – by whom, and with whom. These issues extend to ME data too; confidentiality issues and access restrictions to data collected on learners, programs and institutions can limit the quality, analysis and value of BDME.
Hence, government and health authorities, EMR companies, hospitals and training institutions must cooperate to improve medical data and information systems, and strengthen data exchange and integration across organisations (Chahine et al., 2018; Cook et al., 2010; Ellaway et al., 2014). Appropriate legislations or policies may be necessary. Investments in infrastructure, technologies and expertise to manage and protect data from different sources are also needed. The infrastructure and technological expertise (for collection, storage, processing and analysis) could be centralised in a ‘data warehouse’ – different institutions become data providers to this ‘central’ BD collective (Cook et al., 2010; Ellaway et al., 2014). It is likely that external partners (e.g., data science, informatics) will be involved to facilitate and optimise the use of BD. Under these circumstances, the governance, ownership of, and access to data are important issues to consider.
In using BDME to correlate training and clinical care outcomes, the challenge is being able to accurately link a learner’s (or a cohort of learners’) education and training with patient-level or system-level clinical outcomes (Chahine et al., 2018; Cook et al., 2010). Given that multiple healthcare providers (students, residents, practicing physicians) may be involved in the care of a particular patient, innovative data analytical algorithms or techniques will be necessary in order to identify or ‘tag’ different aspects of clinical care or patient encounters, and accurately attribute these to specific providers over prolonged periods of time, and across institutional, clinical and educational boundaries (Chahine et al., 2018; Cook et al., 2010). If successful, this will provide unprecedented potential for performance assessment and evaluation.
The application of BDME also has inherent limitations and fallibility (Chahine et al., 2018; Ellaway et al., 2014). The interpretations and conclusions (and the subsequent decisions and actions) based on BDME must be made with extreme caution. The standards and rigours of academic and scientific research must be applied and met – in the collection methods, precision, representativeness of data. There is intrinsic bias in BD due to the fact that information that cannot (or simply are not) be captured may be undervalued or ignored. Predicting trends and judging current and future potential and success of individuals or programs must similarly be tempered with caution (Chahine et al., 2018; Cook et al., 2010). Major decisions (especially summative) must be based on time-honoured, empirically proven principles: multiple data points, from multiple sources (triangulation), at different time points (reiterative), and after considering the dynamic nature of learning and education in reality.
There are real risks to the individuals and systems if BDME is used out of context, or for unintended purposes. For instance, should BDME be used to alter a learner’s (or a group of learners’) career path or choice? Should we judge learners based on ‘normal’ patterns of learner behaviour derived from BDME? Also, from the faculty’s perspective, it is tempting to use only those educational interventions that were ‘shown to work’ by BDME, at the expense of all others.
This article is not intended to propose solutions to the many issues surrounding the use of BDME. The permeation of BD into ME appears inexorable. It is time for the ME community to take the lead to critically appraise and shape the conversation surrounding BDME, so as to set the agenda and direction for the best use of BDME.
Notes on Contributors
Heng-Wai Yuen is an adjunct Associate Professor with the Duke-NUS Medical School and the Singapore University of Technology and Design (SUTD). He is the Director of Otology and Hearing Implants in the Department of Otolaryngology-Head & Neck Surgery, and the Deputy Director of Undergraduate Medical Education at Changi General Hospital.
Abhilash Balakrishnan is an adjunct Associate Professor with the Duke-NUS Medical School and Clinical Associate Professor with the Yong Loo Lin School of Medicine at the National University of Singapore. He is also the Deputy Head of Department (Education) in the Department of Otolaryngology at Singapore General Hospital.
Funding
The authors declare no funding is involved for this paper.
Declaration of Interest
The authors declare no conflict of interest.
References
Callahan, C. A., Hojat, M., Veloski, J., Erdmann, J. B., & Gonnella, J. S. (2010). The predictive validity of three versions of the MCAT in relation to performance in medical school, residency, and licensing examinations: A longitudinal study of 36 classes of Jefferson Medical College. Academic Medicine, 85(6), 980-987. https://doi.org/10.1097/ACM.0b013e3181cece3d
Chahine, S., Kulasegaram, K., Wright, S., Monteiro, S., Grierson, L. E., Barber, C., … Touchie, C. (2018). A call to investigate the relationship between education and health outcomes using big data. Academic Medicine, 93(6), 829-832. https://doi.org/10.1097/ACM.0000000000002217
Cook, D. A., Andriole, D. A., Durning, S. J., Roberts, N. K., & Triola, M. M. (2010). Longitudinal research databases in medical education: Facilitating the study of educational outcomes over time and across institutions. Academic Medicine, 85(8), 1340-1346. https://doi.org/10.1097/ACM.0b013e3181e5c050
Ellaway, R. H., Pusic, M. V., Galbraith, R. M., & Cameron, T. (2014). Developing the role of big data and analytics in health professional education. Medical Teacher, 36(3), 216-222. https://doi.org/10.3109/0142159X.2014.874553
Schneeweiss, S. (2014). Learning from big health care data. The New England Journal of Medicine, 370(23), 2161-2163. https://doi.org/10.1056/NEJMp1401111
*Heng-Wai Yuen
Changi General Hospital,
2 Simei Street 3, Singapore 539889
Tel: +65 69366259
Email: yuen.heng.wai@singhealth.com.sg
Published online: 5 May, TAPS 2020, 5(2), 48-50
https://doi.org/10.29060/TAPS.2020-5-2/PV2176
Neel Sharma1, Mads S. Bergholt2, Rosalia Moreddu3 & Ali K. Yetisen3
1Queen Elizabeth Hospital Birmingham, United Kingdom; 2Centre for Craniofacial and Regenerative Biology, Faculty of Dentistry, Oral & Craniofacial Sciences, King’s College London, United Kingdom; 3Department of Chemical Engineering, Imperial College London, United Kingdom
I. INTRODUCTION
Medicine historically relied on astute history and examination skills. As technology was lacking, ward rounds focused on debate and discussion of diagnoses and possible differential diagnoses based on the history and physical examination. The technology movement into healthcare was never truly predicted. With its occurrence, came the ability to scan a patient from top to toe via computed tomography and magnetic resonance imaging. Technology now serves as our main diagnostic tool (Patel, 2013).
‘When did the patient have their scan? Shall we repeat it? Maybe we are missing a subtle cancer?’ These are now common questions.
For those that enter medicine, we do so on the basis of the intellectual challenge, the desire to piece together a patient’s symptoms and examination findings and formulate a diagnosis. However, we have now become technicians. Patients are imaged and labelled depending on what the scan tells us. Has our critical thinking now gone (Hall, 2019)?
We urgently need to reinject the thinking into healthcare. Otherwise, retention and recruitment into the medical field will diminish. How can we achieve this? Technologies certainly will not die and patients want them. Hence, we envisage a change in the way doctors are trained. A system where future doctors not only gain clinical knowledge but engineering expertise. By developing a training system whereby engineering colleagues can provide medics an understanding of device and diagnostic development, we will not only be able to accurately diagnose and manage patients but also be able to keep the thinking alive. As clinicians can recognise the limitations in how patients are managed, they can solve these limitations once armed with engineering know-how.
II. METHODS
As the authors of this piece, we have launched the first global clinician engineering platform for medical undergraduates, the clinician engineer hub (www.clinicianengineer.com). The hub is led by one founding clinician NS and two founding engineers MSB and AKY. All members have global experience in their respective fields including internal medicine, gastroenterology, biomedical imaging and biosensors. Next came the decision to recruit an international advisory board, comprising senior experts and mid-level career individuals. Recognising the fact that medical students undertake sabbaticals abroad, it was essential to ensure an international angle. The focus of the first programme was on biomedical optics for early cancer diagnosis and wearable sensors for real-time health monitoring. The focus of the engineering content was based on consensus among the founders and advisory board with the decision to review the theme of the programme on a biannual basis. The programme took place over a two-week period. The first week involved clinical observation to understand the clinical problem and what potential limitations exist in terms of diagnosis and treatment. This involved exposure to patients in an outpatient setting and in the ward. The second week focused on theoretical aspects of engineering and device development. Additionally, it involved lectures and hands-on practical activities. Each learner gained appropriate credit for full participation in the programme with the opportunity to provide feedback on how to enhance the learning experience.
III. DISCUSSION
As the programme builds, our aim is to next integrate engineering training during medical school which can be done in a variety of ways. It could, for example, commence as an elective. Alternatively, of more value, during each attached clinical rotation, be it gastroenterology, cardiology, or respiratory medicine, there could be dedicated teaching time allied to limitations in current diagnostic practice and management strategies with time spent appreciating current engineering strategies and solutions, seamlessly integrated into the curricula (Tables 1 and 2). This way, both disciplines can be learnt simultaneously without prolongation of training time.
The clinician engineer training scheme can also be integrated into allied health care curricula. Globally, we are seeing healthcare being delivered by nurse specialists, physician assistants, and specialist prescribers. Nurse specialists, for example, exist in the field of heart failure management, diabetes, and asthma. Physician assistants play a significant role in the history and examination of patients as well as diagnosis forming. As these individuals enter their respective university programmes, their exposure to patient problems can also be of benefit to developing new diagnostic and treatment methods, alongside fellow clinicians, through an integrated engineering syllabus.
|
Cardiology |
Gastroenterology |
|
AM: Ward round |
AM: Ward round |
|
PM: Clinic |
PM: Endoscopy observation |
Table 1. Current teaching model during medical school
|
Cardiology |
Gastroenterology |
|
AM: Ward round/ Clinic (alternating) |
AM: Ward round/ Endoscopy (alternating) |
|
PM: Teaching on diagnostic and treatment limitations in cardiology with exposure to novel engineering-based solutions (e.g., wearable sensor construction for arrhythmia detection) |
PM: Teaching on diagnostic limitations in gastroenterology (e.g., limitations with current endoscopic equipment for cancer detection and possible solutions such as spectroscopy) |
Table 2. The proposed timetable for clinician engineering teaching at medical school
IV. CONCLUSION
Innovation in medical education is urgently needed. For decades, we have spent time and resources appreciating the most appropriate teaching strategy or way to assess our learners. We have now reached saturation in this regard. There is no one optimum way to teach a learner and no single optimum assessment method. What we now need is a stronger focus on healthcare deficiencies at a time where healthcare provision remains heavily invested in technology. Critics may highlight concerns allied to faculty resources, training of faculty as well as accreditation. However, it is our duty as educators to ensure our patients benefit from future doctors who have been trained in accordance with how healthcare is evolving. With expert clinicians and engineers already highly trained and guiding such programmes, full accreditation can be gained. The future is now not just clinical care but clinician engineering.
Notes on Contributors
NS is the founder of the clinician engineer hub and a clinician academic in gastroenterology.
MSB is a co-founder of the clinician engineer hub and lecturer in biophotonics.
AKY is a co-founder of the clinician engineer hub and senior lecturer in chemical engineering.
RM is a PhD candidate in biomedical engineering and instructor for the clinician engineer hub.
NS, MSB, AKY, and RM contributed to the article equally and agreed on the final version for submission.
Funding
The authors declare no funding is involved for this paper.
Declaration of Interest
The authors declare no conflict of interest.
References
Hall, H. (2019, January 15). Critical thinking in medicine. Science-Based Medicine. Retrieved from https://sciencebasedmedicine.org/critical-thinking-in-medicine
Patel, K. (2013). Is clinical examination dead? BMJ, 346, f3442. https://doi.org/10.1136/bmj.f3442
*Neel Sharma
Department of Gastroenterology,
Queen Elizabeth Hospital Birmingham,
Mindelsohn Way, B15 2TH
Tel: 0121 371 2000
Email: n.sharma.1@bham.ac.uk
Published online: 5 May, TAPS 2020, 5(2), 45-47
https://doi.org/10.29060/TAPS.2020-5-2/PV1085
Chi-Wan Lai
Koo Foundation Sun Yat-Sen Cancer Center, Taipei, Taiwan
I. INTRODUCTION
Most medical education programmes in Taiwan accept students upon high school graduation. Medical education used to consist of seven years with the last year being an internship. Since 2013, medical students have graduated at the end of six years, and the internship has been moved to a postgraduate year. In both formats, students have been offered medical humanities courses in the “pre-med” phase, i.e. the first two years of medical school. From the third year onward, however, students rarely have exposure to subjects related to humanism, other than courses on medical ethics and some problem-based learning case discussions. Moreover, medical students have had very little exposure to humanities in high school. Such limited exposure to humanities during medical school can have detrimental effects on cultivating humanistic physicians in Taiwan.
It is known that the majority of medical schools in the U.S. are post-baccalaureate system, i.e. most of the medical students have already had exposure to humanities courses during undergraduate years. Yet research shows that medical students in the U.S. have problems with empathy decline as they advance through medical school (Neumann et al., 2011). The Arnold P. Gold Foundation has been advocating for infusing the human connection into healthcare, and Plant, Barone, Serwint, & Butani (2015) articulated very well the need to take humanism back to the bedside. Lacking these efforts, the empathy decline among medical students in Taiwan could conceivably be even more serious than in the U.S.
This paper advocates for the importance of instilling humanism at the bedside during clinical rotations to serve as “booster shots” to enhance the medical humanities learned by students in the pre-med phase.
II. MY PERSONAL EXPERIENCES IN LEARNING AND TEACHING AT THE BEDSIDE
Following my graduation from medical school at National Taiwan University School of Medicine in 1969, I completed a four-year residency in the Neurology & Psychiatry Department at Taiwan Medical University Hospital (1970-1974) and did an attending year before I went to the University of Minnesota to start another residency program in Neurology (1975-1978). In Minnesota, I was deeply impressed by the bedside teaching of my respected mentor, Dr. A. B. Baker, the chairman of the Neurology Department. I vividly remember one unforgettable incident – before he did a “straight leg raising test” (Swartz, 2014) on a female patient suffering from sciatica, he first asked for a towel to cover the area between the patient’s legs before raising her leg to test the possibility of sciatic nerve entrapment. He clearly demonstrated sensitivity to the patient’s potential feeling of embarrassment caused by performing such a test while surrounded by students and residents. Through several of these “enlightening moments” at the bedside, he demonstrated his famous quote: “Students learn from observing how you do, rather than from what you say.”
Since then, I have continued my interest in bedside teaching while teaching at the University of Kansas Medical Center (1979-1998) and upon my return to Taiwan in 1998.
It is my personal conviction that bedside teaching should include not only medical knowledge and skills but also bedside manner, sympathetic listening and empathetic communication. Such teaching can serve as “booster shots” during clinical years to enhance the humanism that medical students learn in earlier years. For more than a decade, I have been conducting regular bedside teaching in three teaching hospitals for 5th or 6th year medical students at National Yang Ming Medical University, National Taiwan University, and National Cheng-Kung University during their clerkship rotating through neurology.
I would like to present the following two cases to illustrate how to enhance students’ sensitivity to the suffering of others (patients and their families), while also teaching neurological examination techniques, differential diagnoses, and management.
III. CASE 1: A PATIENT WITH MYASTHENIA GRAVIS WHO SUFFERS FROM DIPLOPIA
The diagnosis was delayed by his presenting chief complaints as “dizziness,” for which he visited several ENT doctors, until finally he was referred to neurologists. Students were puzzled by how the patient could “confuse” diplopia (“double vision”) with dizziness. I then demonstrated to students how to self-induce diplopia by stretching out their left arm, with index finger pointed to the sky, and then continue to stare at this finger while trying to apply pressure to their right eyeball with their right hand. This would artificially create different positions of the eyeballs (dysconjugation), resulting in problems with the fusion of two images projected from the retinae to the brain. This caused “double vision” and a dizzy feeling, which was exactly what happened to this patient. Students then appreciated what the patient was suffering and understood why the patient could perceive “double vision” as “dizziness.”
IV. CASE 2: A PATIENT AT THE END-STAGE OF AMYOTROPHIC LATERAL SCLEROSIS, A DEVASTATING MOTOR NEURON DISEASE THAT HAS NO EFFECTIVE TREATMENT
After the student presented the history of the patient, I reminded students to find out how we could help such a seemingly “medically helpless” patient. After observing severe bulbar symptoms and demonstrating the coexistence of upper and lower motor neuron signs at bedside, I thought it might be a good case to lead the patient into a discussion of serious issues related to end-of-life.
So I posed a question – “What do you worry about the most?” – trying to lead the patient into a discussion of whether he would consider accepting emergent intubation followed by long term ventilation when he developed difficulty with breathing. Unexpectedly, the patient responded, “What I worry about the most is my daughters’ education.” He then went on to share with us his story of how his lack of formal education due to poverty led him to the life-long misery of humiliation at work. Consequently, he has tried to save as much money as possible for his two daughters’ college education. Unfortunately, his financial status had been seriously compromised by his loss of job and increasing medical expenses since he became ill, at a time when his two daughters would soon graduate from high school.
After we left the patient and started discussing the patient’s neurological findings, one student reminded us that we had not discussed how to help this patient. She went on to share with us her thoughts: she would like to see the patient’s daughters, discuss with them whether they themselves were interested in going to college, and if so, she would urge them to speak to their father about their desire to work in the daytime and to attend college through evening school.
We were all impressed by this student’s thoughtful proposal, and I went on to praise her, saying that she had beautifully illustrated the truth of the following statement: “Although there is nothing more that can be done for the body, this does not mean that there is nothing more that can be done for the sick person” (Cassell, 2004).
V. GENERAL DISCUSSION OF HOW I CONDUCT BEDSIDE TEACHING
At the end of my bedside teaching, I usually ask students to share what they have learned. Students tend to recall cognitive learning, i.e. medical knowledge of diagnosis and treatment as well as clinical skills in neurological exam. Then under prompting, they begin to share their observations of behavioral/affective aspects and express their empathy towards the suffering of patients and their families. Some of them voice their appreciation for bedside manner and communication skills demonstrated by the medical team. At the end, I have consistently tried to raise their sensitivity and draw attention to the patient’s suffering. Lately, I like to share with students the joy of reading Dr. Charon’s succinct article, “To See the Suffering,” in which she writes, “To see the suffering might be what the humanities in medicine are for, and that those who become capable of seeing the suffering around them in medical practice both experience the cost of countenancing the full burden of illness and death and, simultaneously, comprehend with clarity the worth of this thing, this life.” (Charon, 2017)
VI. MY PERSONAL PLEA FOR THE INTEGRATION OF CLINICAL MEDICINE AND HUMANITIES IN MEDICAL EDUCATION PROGRAM
Attention to humanistic issues at the bedside demonstrates to students the relevance and application of humanities in individual cases and leads to a deeper appreciation of what they have learned about medical humanities during their pre-med years. Consequently, such bedside teaching can serve as “booster shots” to rekindle students’ interest in the humanistic aspects of patient care. However, it is difficult to expect lasting effects on the attitudes and behaviors of medical trainees unless such teaching can be frequently and widely practiced throughout clinical rotations.
Therefore, I would like to recommend that more attending physicians in teaching hospitals should be encouraged to teach humanism at the bedside. Medical schools should set a high priority for the clinical faculty to help students enhance their sensitivity “to see the suffering” and develop empathy towards patients. If possible, such efforts should be incorporated into faculty development programs for clinical teachers from all clinical departments in teaching hospitals.
Note on Contributor
Chi-Wan Lai, M.D. is the chair professor of medical education, attending physician in the Division of Neurology, Koo Foundation Sun Yat-Sen Cancer Center, Taipei, Taiwan.
Funding
The author declares no funding is involved for this paper.
Declaration of Interest
The author declares no conflicts of interest.
References
Cassell, E. J. (2004). The nature of suffering and the goals of medicine (2nd ed., p. 118). United Kingdom: Oxford University Press.
Charon, R. (2017). To see the suffering. Academic Medicine, 92(12), 1668-1670. https://doi.org/10.1097/ACM.0000000000001989
Neumann, M., Edelhäuser, F., Tauschel, D., Fischer, M. R., Wirtz, M., Woopen, C., … Scheffer C. (2011). Empathy decline and its reasons: A systematic review of studies with medical students and residents. Academic Medicine, 86(8), 996-1009. https://doi.org/10.1097/ACM.0b013e318221e615
Plant, J., Barone, M. A., Serwint, J. R., & Butani, L. (2015). Taking humanism back to the bedside. Pediatrics, 136(5), 828-830. https://doi.org/10.1542/peds.2015-3042
Swartz, M. H. (2014). Textbook of physical diagnosis: History and Examination (7th ed., p. 564). Philadelphia, PA: Elsevier.
*Lai Chi-Wan
125 Lih-Der Road,
Pei-Tou District, Taipei, Taiwan
Telephone: +886 2 2897-0011
Email address: chiwanlai@gmail.com
Published online: 5 May, TAPS 2020, 5(2), 57-58
https://doi.org/10.29060/TAPS.2020-5-2/LE2221
Muhammad Raihan Jumat
Office of Education, Duke-NUS Medical School
I read with great interest Samarasekera and Gwee’s article in TAPS (January, 2020) entitled: “Grit in healthcare education practice”. The authors cited Duckworth’s seminal studies on grit and its strong correlation with success. The authors suggested that grit be used to select for medical students and for healthcare systems to adopt organisational grit. I applaud the authors’ call for implementing organisational grit in healthcare. This is a step forward in working out the multiple issues plaguing healthcare. Interestingly, the call to implement organisational grit might not make it necessary to select for grit upon medical school admission.
Duckworth had posited that the mere assembly of gritty individuals might not necessarily create a gritty organisation (Duckworth, 2016). Students who test as gritty upon admission might be gritty in a different context than that of a medical school. Medical school has its own specific set of challenges which are not shared in many other pre-medical school experience. Hence, students who type as gritty on a medical school entry exam might not remain gritty in medical school.
Grit needs to be developed as a team within an organisation with a shared goal (Duckworth, 2016; Lee & Duckworth, 2018). This development starts with assembling a group of individuals with similar interests. These individuals are then encouraged to work together with chances to carry out deliberate practice and constant reminders of their shared purpose. This group should be even encouraged to fail and learn from those failures. This group will then develop grit as a unit (Duckworth, 2016).
Creating an environment which is demanding yet nurturing is key in promoting grit (Lee & Duckworth, 2018). Team-based or problem-based learning provides a conducive setting for such an environment to thrive in medical school. Students are grouped in teams and are faced with demanding challenges which would force them to work together over an extended period of time. These students are allowed to fail and learn from their mistakes. Over time, the team develops grit.
The formation of a culture which promotes and breeds grit within an organisation would be a stronger force to withstand the demanding challenges of healthcare than just a selection of gritty individuals. Structural changes in healthcare to allow for organisational grit to take root should be undertaken. Increased reports of physician burnout necessitate that healthcare workers be given support. Organisational grit would give healthcare workers the support they require.
Note on Contributor
Muhammad Raihan Jumat, PhD, is an Education Fellow in the Office of Educaiton at Duke-NUS Medical School. The author conceived the idea and wrote this letter.
Acknowledgements
The author would like to thank Professors Scott Compton and Sandy Cook for their advice and encouragement in writing this letter.
Funding
No funding was involved in this letter.
Declaration of Interest
The author does not have any competing interests.
References
Duckworth, A. (2016). Grit: The power of passion and perseverance (First Scribner hardcover ed.). New York, NY: Scribner.
Lee, T. H. & Duckworth, A. L. (2018). Organizational grit. Retrieved from Harvard Business Review, https://hbr.org/2018/09/organizationalgrit
*Muhammad Raihan Jumat
Office of Education,
Duke-NUS Medical School,
8 College Road,
Singapore 169857
Tel: +6 56516 4771
E-mail: raihan.jumat@duke-nus.edu.sg
Published online: 5 May, TAPS 2020, 5(2), 41-44
https://doi.org/10.29060/TAPS.2020-5-2/SC2134
Sok Mui May Lim1,2, Zi An Galvyn Goh2 & Bhing Leet Tan1
1Health and Social Sciences Cluster, Singapore Institute of Technology, Singapore; 2Centre for Learning Environment and Assessment Development (CoLEAD), Singapore Institute of Technology, Singapore
Abstract
The use of standardised patients has become integral in the contemporary healthcare and medical education sector, with ongoing discussion on exploring ways to improve existing standardised patient programs. One potentially untapped group in society that may contribute to such programs are persons with disabilities. Persons with disabilities have journeyed through the healthcare system, from injury to post-rehabilitation, and can provide inputs based on their experiences beyond their conditions. This paper draws on our experiences gained from a two-phase experiential learning research project that involved occupational therapy students learning from persons with disabilities. This paper aims to provide eight highly feasible, systematic tips to involve persons with disabilities as standardised patients for assessments and practical lessons. We highlight the importance of considering persons with disabilities when they are in their role of standardised patients as paid co-workers rather than volunteers or patients. This partnership between persons with disabilities and educators should be viewed as a reciprocally beneficial one whereby the university and the disability community learn from one another.
Keywords: Standardised Patients, Objective Structured Clinical Examination (OSCE), Persons with Disabilities, Inclusion, Role-play, Script, Practical Lessons
I. INTRODUCTION
The use of standardised patients (SPs) has become integral to the contemporary healthcare and medical education sector. While an SP is commonly defined as a person trained to portray a scenario, an SP can also be an actual patient using his or her own history and physical exam findings (Kowitlawakul, Chow, Salam, & Ignacio, 2015). Presently, persons with disability (PWDs) have participated in SP programs, albeit less frequently and on a smaller scale (Long-Bellil et al., 2011; Minihan et al., 2004; Wells, Byron, McMullen, & Birchall, 2002). SPs with disabilities have also been used in Singapore hospitals, but mainly as patients to be examined for their own medical conditions. PWDs have a lot to offer in clinical education beyond sharing about their conditions.
A. Why Incorporate Persons with Disabilities into SP Programs?
There are many benefits in involving PWDs in SP programs. PWDs may be able to impart knowledge that ‘goes beyond the textbook’, due to their experiences of receiving services from various healthcare professionals – from the time the disability occurred to the post-rehabilitation phase of living independently in society. The input given based on their individual experiences would, therefore, be authentic (Wells et al., 2002). Students can get practice working with real PWDs in a safe setting where they can make mistakes and receive feedback before going for their clinical placements and meeting with real patients (Minihan et al., 2004). This can nurture a new generation of healthcare professionals who may be more proficient in treating PWDs, thereby raising the service delivery standard for the entire sector.
B. Perspectives Gained From Previous Experiential Learning Project
This paper is based on our experiences gained from a previous experiential learning research project. PWDs participated in a two-phase experiential learning research project that spanned two years (Lim, Tan, Lim, & Goh, 2018). In phase one, the PWDs acted as community teachers to occupational therapy student groups, interacting with them in the community while performing their daily activities. This paper draws from our experiences in Phase Two of the study, in which a group of PWDs were trained to and worked as SPs in practical classes and Objective Structured Clinical Examinations (OSCEs). Upon the conclusion of the research project, PWDs continue to be part of the degree programme contributing as community teachers and SPs. The paper aims to provide practical helpful tips in bringing PWDs onboard as SPs.
II. DISCUSSION
A. Tip 1 – Interviewing and Selecting PWDs Who Are Suitable for Acting
PWDs were selected based on six criteria determined by faculty members in the health profession who have prior experience working with SPs. First, the PWD has an interest in healthcare education and wants to work with students for the purpose of educating them as future healthcare professionals. Second, the PWD should have come to terms and accepted their disability. It is very difficult for them to talk about their disability or role-play as a patient when they are still struggling emotionally with their own conditions. Third, the PWD does not have cognitive impairment and is able to understand and remember the script for role-playing. Fourth, he/she must be able to communicate clearly and coherently. Fifth, the PWD should be willing to learn the basics of acting or role-playing. Sixth, he/she must understand the objectives of the training or assessment, such as being impartial to all students and being honest in giving feedback when required.
B. Tip 2 – Training Should Be Conducted in Gradual Phases
Training PWDs as SPs can be carried out in a gradual phase as outlined in details in Figure 1. In the first phase, novice PWD SPs are taught the basics of role-play by faculty and experienced SPs. In the second phase, the entire group goes through a common script. Novice PWD SPs observe the faculty and experienced SPs enact the script. Then, the novice PWD SPs practice amongst themselves and receive feedback.
After the training, faculty should speak to the PWDs individually to determine if they are comfortable with role-playing and address any queries that they may have. It is only after they attempt the role of an SP that they can personally assess their comfort level and confidence. This can ensure that the PWDs who participate are comfortable with their roles and feel engaged and respected by the institution.
In the third phase, PWD SPs can progress to non-graded practical lessons with students, which are less stressful for both students and PWD SPs. In subsequent phases, the faculty can then decide to select PWD SPs whom they deem are ready for summative assessments such as the OSCE.
C. Tip 3 – Start Novice PWD SPs with Simple and Suitable Scripts
Initial scripts should be simple and should not require complex acting skills. It takes time to gain confidence in memorising required lines, maintaining their roles as well as acting in scenarios which require more expression of emotions. Scripts that involve more sophisticated acting skills (e.g., maintenance of strong emotions) should be reserved for SPs who are experienced and confident with acting. The PWD SPs should be matched to suitable scripts that do not conflict with their disability. For example, a PWD SP who uses a wheelchair cannot be paired with a script that involves walking. The combination of progressing gradually and usage of suitable scripts allows for PWD SPs to refine their skills and ensure that their acting skills do not compromise the students’ learning experience.
D. Tip 4 – Prepare Students Not to Be Surprised By Real Disability
Prior to the interaction session, students should be pre-empted by the faculty that they would be working with PWDs who may have a range of disabilities. This is to prevent unnecessary surprise. In addition, students should be reminded that the disability may or may not be the focus of the scenario, depending on the instruction given to the student. For example, in an OSCE scenario, students may be tasked to explain a medical error or demonstrate a procedural skill instead of addressing the disability of the SP. This pre-empting can be complemented with teaching communication skills geared towards interacting with PWDs.
E. Tip 5 – Checking Accessibility – Within and Outside of the Venue
Ensuring accessibility prior to the session is important. This includes the route from the nearest public transport node (e.g., train station) to the venue. Things to take note of are the availability of ramps and lifts for wheelchair users and the presence of accessible parking lots. In addition, the venue where the lesson or assessment is going to take place needs to be inspected to ensure that the entrances and exits are wide enough for wheelchairs access.
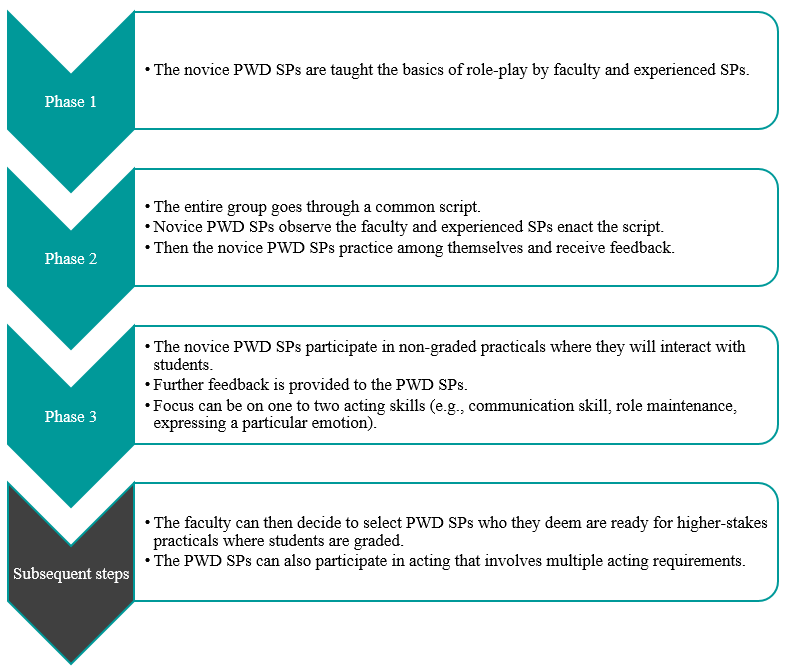
Figure 1. Diagram to outline general recommended steps for training PWD SPs
F. Tip 6 – Pay PWDs at Market Rates and Accord Them Identical Contractual Rights
PWD SPs should be remunerated at market rates that are equal to SPs without disability. They also sign the same SP contract and fulfil the same legal obligations. In performing the role of the SP, they are treated as co-workers of the university, not volunteers or patients. This reflects the principles of equality and diversity, as well as the seriousness of their roles as active members of the healthcare and medical education system. If there are certain risks involved in their interaction with students, such risks should be made clear to the PWD SPs, so they can make an informed decision on accepting the job.
G. Tip 7 – Provide Opportunity for PWDs to Give Feedback
PWDs can be a valuable resource in providing feedback to faculty, scenario developers and other SPs. Similarly, they may be able to give insightful feedback to students. It is important to train the PWD SPs on the methods of providing feedback to students. Given their lived experience, they can provide insight into how real patients would respond and react while suggesting ways for trainee healthcare professionals to respond in a more patient-centred manner.
H. Tip 8 – Reflect and Improve
Carrying out an evaluation with the respective stakeholders, whether they are PWD SPs, faculty, or students, is key to the success of an inclusive SP program. This can also ensure quality assurance of the program. The following are several broad questions which can be considered in the evaluation. Firstly, whether the stakeholder faced any challenges during the session. Secondly, whether the scenarios or scripts worked well for PWD SPs to interact with students. Thirdly, whether there are any other ways that the learning experience can be improved. This can provide rich data for the SP program developers to reflect and improve upon the pedagogy. We have received positive feedback from both students and PWDs in this project.
III. CONCLUSION
It is important to empower PWDs and create a dynamic relationship between them and healthcare professionals/
educators. For an inclusive SP program to be effective, educators must change their own mindset about PWDs. We have to switch the lens from viewing them as patients to co-workers. This partnership should be viewed as a reciprocally beneficial one whereby the university and the disability community learn from one another. Through the process of engagement, both educators and students learn from PWD SPs about knowledge that goes beyond the textbook, and the factors that enhance or diminish the quality of healthcare/medical service delivery from individuals who have experienced going through the healthcare/medical system. With time and with more training institutions engaging PWDs as SPs, this can be a potentially viable employment option for PWDs.
Notes on Contributors
Associate Professor May Lim is the Director of the Centre for Learning Environment and Assessment Development (CoLEAD) at the Singapore Institute of Technology, and a faculty in the Health and Social Sciences Cluster teaching occupational therapy.
At the time when this work was done, Mr Goh Zi An Galvyn was a research assistant in the Centre for Learning Environment and Assessment Development (CoLEAD) at the Singapore Institute of Technology.
Associate Professor Tan Bhing Leet is the Deputy Cluster Director (Applied Learning) of the Health and Social Sciences Cluster, and Programme Director of the Bachelor of Science in Occupational Therapy degree programme at the Singapore Institute of Technology.
Ethical Approval
Ethics approval was granted by the Singapore Institute of Technology Institutional Review Board for this project (IRB number: 20150002).
Acknowledgements
The authors thank all faculty, students, PWD and non-PWD standardised patients who were involved in the Singapore Institute of Technology Bachelor of Science in Occupational Therapy degree programme. In addition, we would like to extend our deepest gratitude to Associate Professor Tham Kum Ying, Education Director of Tan Tock Seng Hospital Pre-Professional Education Office and senior lecturers Miss Heidi Tan and Mr Lim Hua Beng from the Singapore Institute of Technology.
Funding
Funding was provided from the Singapore Ministry of Education (MOE Tertiary Education Research Fund grant: R-MOE-A203-A002).
Declaration of Interest
The authors declare no conflict of interest concerning any aspect of this research.
References
Kowitlawakul, Y., Chow, Y., Salam, Z., & Ignacio, J. (2015). Exploring the use of standardized patients for simulation-based learning in preparing advanced practice nurses. Nurse Education Today, 35(7), 894-899. https://doi.org/10.1016/j.nedt.2015.03.004
Lim, S. M., Tan, B. L., Lim, H. B., & Goh, Z. A. G. (2018). Engaging persons with disabilities as community teachers for experiential learning in occupational therapy education. Hong Kong Journal of Occupational Therapy, 31(1), 36-45. https://doi.org/10.1177/1569186118783877
Long-Bellil, L. M., Robey, K. L., Graham, C. L., Minihan, P. M., Smeltzer, S. C., Kahn, P., & Alliance for Disability in Health Care Education. (2011). Teaching medical students about disability: The use of standardized patients. Academic Medicine, 86(9), 1163-1170. https://doi.org/10.1097/ACM.0b013e318226b5dc
Minihan, P. M., Bradshaw, Y. S., Long, L. M., Altman, W., Perduta-Fulginiti, S., Ector, J., … Sneirson, R. (2004). Teaching about disability: Involving patients with disabilities as medical educators. Disability Studies Quarterly, 24(4). https://doi.org/10.18061/dsq.v24i4.883
Wells, T. P. E., Byron, M. A., McMullen, S. H. P., & Birchall, M. A. (2002). Disability teaching for medical students: Disabled people contribute to curriculum development. Medical Education, 36(8), 788-790. https://onlinelibrary.wiley.com/doi/abs/10.1046/j.1365-2923.2002.01264_1.x
*Lim Sok Mui
Singapore Institute of Technology,
SIT@Dover, 10 Dover Drive,
Singapore 138683
Email: may.lim@singaporetech.edu.sg
Published online: 5 May, TAPS 2020, 5(2), 32-40
https://doi.org/10.29060/TAPS.2020-5-2/OA2194
Suriyakumar Mahendra Arnold1, Sepali Wickrematilake2, Dinusha Fernando3, Roshan Sampath1, Palitha Karunapema4 & Pasyodun Koralage Buddhika Mahesh5
1Quarantine Unit, Ministry of Health Sri Lanka; 2Regional Director of Health Services Office, Matale, Sri Lanka; 3Regional Director of Health Services Office, Puttalam, Sri Lanka; 4Health Promotion Bureau, Ministry of Health, Sri Lanka; 5Ministry of Health, Sri Lanka
Abstract
Background: The duties of Public Health Inspectors (PHI) includes those related to food legislation. Effective methods are being explored in providing refresher training for them amidst the constraints of resources.
Objective: To assess the knowledge, attitudes and skills of the PHI on food legislation and to evaluate the effectiveness of a Distance Education (DE) programme in improving these.
Methodology: The study included quasi-experimental educational intervention with a pre- and post- assessments. 105and 109 PHI were recruited for the intervention and control groups. Pre and post interventional assessments on the knowledge, attitudes, self-assessed competencies and performance were done with a self-administered questionnaire and observational checklist. Intervention group was exposed to an educational intervention through a distance education programme. Post-assessments were done following four months of the intervention.
Results: The pre interventional knowledge and performance was poor. PHI had unfavorable views. Post intervention mean knowledge and performance scores revealed that a statistically significant improvement (P<0.001) has occurred in the intervention group. Change in the opinions on usefulness of in-service training on food safety to develop knowledge and skills, was statistically significant (P<0.01) in the intervention group.
Conclusion: The DE method used in the present study was feasible to implement and was effective in significantly improving the knowledge and performance of the PHI.
Keywords: Distance Education, Continuing Education, Public Health Inspector, Food Legislation
Practice Highlights
- Continues Education is important for development of knowledge and skills of healthcare staff.
- Distance Education can be successfully used for Continues Education for staff geographically scattered.
I. INTRODUCTION
Learning is an active, continuous, sequential process. Learning takes place more rapidly when the learner has the opportunity to practice and experience what is being learned in a variety of situations. It is facilitated when it takes place in or near the real situation in which the learner expects to work (Schunk, 2012). There is an increasing recognition of the need for health workers to continue their education throughout their career (Price & Reichert, 2017). The changes that take place in health needs and health care policies necessitate continued learning.
Continuing education (CE) should be an integral part of an employment. Adequate provision should therefore be made for it in terms of manpower, study level and financial reimbursement. Whenever possible, CE must be provided at the place of work and must be relevant to the immediate needs of the health care workers and the community he/she serves (Billett et al, 2015; Cedefop, 2015; Kenny, Ralph & Brown, 2006; Sherman & Chappell, 2018).
Professional and technical education with traditional methods of training are often inflexible, time- and place- constrained and too expensive to meet the demand for training (Asian Development Bank, 2014; Scott, 2010). Efforts like technological advancements and distance education techniques have created an immense impact in molding the education methods (Chay, 2019). Distance education (DE) seems to offer a way of providing flexible, effective job-related training.
To be successful, DE programme must be systematically designed, interactively motivational and suited to the needs of the audience (Balaban-Sali, 2008). Distance education has the potential of delivering more educational opportunities to more people than ever before, at lower average cost and most importantly, at a higher quality than most people can get in other ways (Marcinkiewicz, Cybart & Chrominska-Szosland, 2002).
The problem of updating the knowledge and skills of health personnel already on the job still remains as a challenge (Murray & Christison, 2018). It is almost impossible to have them re-trained at the institutions they occupy with face-to-face contact with the physical presence of trainers. Hence it is important to develop novel programmes in updating and refreshing of the health personnel amidst the feasibility constraints.
Food borne diseases account for a major toll on health. According to the World Health Organization (WHO), up to one-third of the populations of developed countries are affected by foodborne illnesses and the problem is likely to be far widespread in developing countries (World Health Organisation, 2002). The administration and implementation of food laws requires a qualified, trained, and efficient food inspection service (Food and Agriculture Organization of UN & WHO, 2003; Sri Lanka Accreditation Board for Conformity Assessment, 2013). Hence, proper training of food inspectors (PHI) is a prerequisite for an efficient food control system.
The need of providing training to PHI to improve their performance has been identified in the National Health Development Plan (NHDP) of Sri Lanka (Ministry of Health Sri Lanka, 2016). Public Health Inspector is one of the main authorised officers to implement public health laws in Sri Lanka. Of their many duties, PHI play a major role in maintaining food safety in the community. In addition, the food legislation is one area where major responsibility in implementation lies with the health sector. Therefore, educational interventions to improve the implementation could be carried out successfully as a part and parcel of the NHDP of Sri Lanka.
This study was done to assess the knowledge, attitudes and skills of the PHI on food legislation and to evaluate the effectiveness of a DE programme in improving these.
II. METHODS
A. Study Design
The study consisted of 3 components; Pre-interventional assessment, a quasi-experimentation and a post-interventional assessment. In the pre- and post-tests assessment of knowledge, attitudes, self-assessment of competencies (SAC) and observation of performance of PHI on implementation of legislation on food safety was carried out.
B. Study Setting
The study was conducted in Gampaha and Kurunegala districts. Range PHI (PHI serving in an allocated PHI range in a MOH area) serving in these districts were selected as the study population. PHI performing duties of specialized campaigns were excluded as they do not carry out activities on food safety. In allocating PHI to the intervention and control groups, all PHI in a single district were allocated to either the intervention or the control group. Random allocation within a district was not possible in this educational intervention as cross-contamination would have occurred if PHI serving in the same area or adjacent areas were included in both the intervention and control groups. Assessment of knowledge, self-assessment of competencies and attitudes were carried out in all the PHI in both groups. However, the performance was assessed in a sub-sample of 25% of PHI in each group due to feasibility-related practical constraints.
C. Study Instruments
Self-administered questionnaires were used for the assessment of knowledge, attitudes and SAC. Performances were assessed by direct observation in the filed and the office settings using check lists. The questionnaires and checklist were developed using Delphi Technique with the participation of Public Health Specialists, Medical Officers of Health, Food & Drugs Inspectors and Public Health Tutors. Knowledge questionnaire had 15 short answer question with a maximum score of 50 marks. Attitude questionnaire had 15 5-point Likert Scale statements and SAC questionnaire had 15 statements with a 4-point rating scale ranging from very competent to cannot perform. Three checklists were for assessment of food handling establishments, food sampling and record keeping in the PHI office. Checklists were administered by the principal investigator. Following the pre-interventional assessment the intervention group was exposed to a distance education programme using distance education modules. The control group was not exposed to this educational programme.
D. Training Needs Assessment
A Training Needs Assessment followed by selection of study topics, development of the curriculum and development of course materials were carried out in preparation of the three distance education modules. Through the training needs-assessment the specific training needs in the poorly performed areas of the pre-test were identified. Topics that were to be incorporated in the distance education modules were selected using the Nominal Group Technique. The topics selected for the three modules were; “1.Legislation on food safety”, “2.Food sampling, Inspection and rating of food establishments and maintenance of records in food safety” and “3.Legal procedures in food safety”.
E. Distance Education Programme
The DE programme was conducted using the printed media. Three DE modules were distributed at monthly interval for three months. Each module contained a tutorial and the participants were requested to answer after studying the entire module. The questions were based on subject matter covered by all the lessons in the module.
Post intervention assessment was conducted after a lapse of four months of administering the final module. The tools used for this assessment i.e. questionnaires and checklists, were identical to those used in the pre intervention assessment.
III. RESULTS
There were 105 PHI in the intervention group and 109 in the control group.
|
Component |
Intervention Group | Control Group | ||||
| Pre | Post |
Signifi cance |
Pre | Post |
Significance |
|
| Mean | Mean | Mean | Mean | |||
|
Enactments on food safety
|
29.4 | 61.3 | P < 0.001 |
30.6
|
32.1 | NS |
|
Food labelling
|
52.4 | 68.1 | P < 0.001 | 54.2 | 56.4 | NS |
|
Food sampling
|
24.0 | 63.4 | P < 0.001 | 24.9 | 26.8 | NS |
|
Meat and fish inspection
|
54.4 | 67.6 | P < 0.001 | 53.6 | 55.6 | NS |
| Legal procedures | 40.3 | 67.8 | P < 0.001 | 41.4 | 43.5 | NS |
Table 1. Comparison of PHI in the intervention and control groups by mean scores of theknowledge assessment before and after the intervention
| Intervention Group | Control Group | ||
| Component | Difference between post and pre mean scores | Difference between post and pre mean scores | Significance |
| Enactments on food safety | +31.9 | +1.5 | P< 0.001 |
| Food labelling | +15.7 | +2.2 | P< 0.001 |
| Food sampling | +39.4 | +1.9 | P< 0.001 |
| Meat and fish inspection | +13.2 | +2.0 | P< 0.001 |
| Legal procedures | +27.5 | +2.1 | P< 0.001 |
Table 2. Comparison of the changes in the mean scores of the knowledge assessment between the intervention and control groups
A. Knowledge
In comparison of the pre and post intervention knowledge scores, PHI in the intervention group has shown statistically significant (P<0.001) improvements in all components. Control group failed to achieve a significant improvement (Table 1).
In the intervention group highest change was seen in the knowledge on ‘food sampling’ (+39.4 marks) and was closely followed by ‘enactments in food safety’ (+31.9 marks). The difference of scores between the two groups achieved a statistical significance at P < 0.001 (Table 2).
B. Attitudes
Except for the change in the attitudes on usefulness of in-service training to develop knowledge and skills where there was a 25.4% increase in the number of PHI of the intervention group who agreed with this statement and showed a statistically significant difference (P<0.01), there was no other significant changes of the attitudes of PHI in both groups (refer Appendix A, Supplementary Table 1).
C. Self assessed competencies
At both pre and post tests a high proportion of the PHI in both groups rated themselves either ‘very competent’ or ‘competent’ in performing activities. Only a minority indicated that they cannot perform the listed activities. The only deviation of this pattern was seen in the intervention group in two activities, “correctly identifying the legislation in which different violations of food safety be prosecuted” and “performing court procedures in court cases in food safety” where an increase of 16.6% and 25.4% respectively was seen from the pre intervention value, which were statistically significant (refer Appendix B, Supplementary Table 2).
D. Performance
In comparison of the mean performance scores obtained in the pre and post intervention assessments the intervention group showed a significant increase (P < 0.001) at the post-intervention assessment in all 3 activities: inspection and categorization of food establishments, food sampling and documentation and maintenance of records. In the control group there was a marginal increase in the mean scores at the post intervention assessment and was not statistically significant (Table 3).
| Intervention Group | Control Group | |||||
| Component |
Pre n=30 |
Post n=30 |
Signifi cance |
Pre n=30 |
Post n=30 |
Significance |
| Mean | Mean | Mean | Mean | |||
| Inspection and categorization of food establishments | 40.1 | 69.3 | P < 0.001 | 42.2 | 44.1 | NS |
| Food sampling | 50.7 | 70.9 | P < 0.001 | 53.5 | 55.1 | NS |
| Planning, documentation and maintenance of records | 29.8 | 47.3 | P < 0.001 | 31.2 | 32.9 | NS |
Table 3. Comparison of mean performance scores before and after intervention
The difference of the pre and post mean performance scores of the intervention and control group showed that the changes in the mean performance scores were marginal in the control group in comparison to the changes of the intervention group (Table 4). The difference of scores between the two groups achieved a statistical significance (P< 0.001).
| Intervention Group | Control Group | ||
| Component | Difference between post and pre means | Difference between post and pre means | Significance |
| Inspection and categorization of food establishments | +29.2 | +1.9 | P< 0.001 |
| Food sampling | +20.2 | +1.6 | P< 0.001 |
| Planning, documentation and maintenance of records | +17.5 | +1.7 | P< 0.001 |
Table 4. Comparison of the changes in mean performance scores between the intervention and control groups
IV. DISCUSSION
This is the first documented local study testing a DE method for improving the knowledge, attitude and skills of PHI on food legislation. CE is a process, including the experiences after initial training that helps the personnel to attain competencies relevant to their work (Gaspard & Yang, 2016). Of the methods available, distance education method has been used successfully in many countries to provide CE for health care workers. With the advances in the healthcare system, it is essential that Sri Lanka evaluate the effectiveness of different strategies in updating the primary healthcare workers. Hence this study is an eye-opener for the policy-planners in relation to the in-service training of the health staff.
Pre-intervention assessment results showed that the overall knowledge was poor in both groups. Similarly there was no significant difference in attitudes, self-assessed competencies and performance between the two groups, thus the intervention and control groups were comparable before the intervention. Therefore, these results also discount the selection bias in the present study.
The findings of the pre-intervention assessment pointed to the need of CE as the total knowledge scores obtained was unsatisfactory. Only 17.1% of the study group and 23.9% of the control group have undergone any training on food safety during the past three years. Thus a majority of the PHI have had no opportunity for CE to improve and update their knowledge. The findings also revealed that the knowledge and performance in enactments in food safety, food sampling and legal procedures were poor. These findings were taken into consideration in selecting study topics for the distance education modules. Gap analysis is important in planning CE (Moore, Green, & Gallis, 2009) and identifying of needs has an impact on performance outcome in CE (Cervero & Gaines, 2015).
In training a large number of health care workers at different geographical locations, it is important to maintain uniformity of such training. In addition, the quality of educational materials provided will have an effect on the outcome of the intervention. The present study considered these factors and the services of experts were obtained in developing DE modules which were technically sound and of high quality. Uniformity was maintained by administering the modules in a similar manner at all centres where the training programme was conducted.
Since a time lag between the intervention and the post intervention assessment is needed to ascertain the sustainability of the effectiveness of the intervention, the post-intervention assessment was carried out four months after administering the final module.
In general there was no change in the attitudes towards implementation of food legislation in both intervention and control groups except for the views expressed on usefulness of in-service training. One of the reasons for no change in views in both groups may be due to the fact that there was no significant change in their working environment, resources and support services. However, these factors were outside the control of the present intervention.
CE activities can lead to improved competencies and performance (Moore et al., 2009). This study revealed that DE strategy used here was effective in improving the knowledge and performance significantly in the intervention group.
The intervention used in the present study was carried out with minimal interference to the routine duties of the trainees. Unlike institutional-based training programmes or workshops, trainees did not have to be away from the work place resulting in incurring a minimal cost. In the present educational intervention, printing cost incurred for the three distance education modules was minimal. Thus as a developing country with health care workers scattered throughout the island, due consideration should be given to shift from traditional institutional-based training at the central level to providing continuing education at the local setting using feasible, cost-effective methods such as DE where appropriate.
The study was limited to two districts in two provinces. This study was conducted in two districts as a quasi-experimental study. Since then the probability of a selection bias cannot be totally excluded. Overall picture could have been obtained if this study was conducted as an island-wide study. These were taken into account in the interpretation of findings. Sustainability of the improved performance as a result of the DE programme would have been better monitored if post interventional assessments were carried out at one-year and two-year period.
V. CONCLUSION
The present intervention was effective in improving the knowledge and performance of the PHI in implementing legislation on food safety indicating the effectiveness of providing continues education to PHI using distance education method. As this method proved to be feasible, of low cost and has the ability to provide training without mobilizing the staff, it can be incorporated into the existing training system for health care workers.
Notes on Contributors
Mahendra Arnold, Sepali Wickramatilake, Dinusha Fernando, Roshan Sampath and Palitha Karunapema are Public Health Specialists attached to the Ministry of Health. Pasyodun Koralage Buddhika Mahesh is a Senior Registrar in Community Medicine of the Ministry of Health.
Ethical Approval
Ethical approval was obtained from Ethics Committee, Faculty of Medicine, University of Colombo.
Acknowledgements
The authors would like to acknowledge the Public Health Inspectors who participated in this study.
Funding
This study did not receive any external funding.
Declaration of Interest
The authors do not have any conflict of interest to declare.
References
Asian Development Bank (2014). Innovative Strategies in Technical and Vocational Education and Training for Accelerated Human Resource Development in South Asia. Mandaluyong City, Philippines: Asian Development Bank.
Billett, S., Choy, S., Dymock, D., Smith, R., Henderson, A., Tyler, M., & Kelly, A.(2015). Towards more effective continuing education and training for Australian workers, NCVER, Adelaide.
Balaban-Sali, J. (2008). Designing motivational learning systems in distance education. Turkish Online Journal of Distance Education-TOJDE, 9(3), 149-159.
Cervero, R. M., & Gaines, J. K. (2015). The impact of CME on physician performance and patient health outcomes: An updated synthesis of systematic reviews. Journal of Continuing Education in the Health Professions, 35(2), 131–138.
Chay, O. M. (2019). Transformation of medical education over the years – A personal view. The Asia Pacific Scolar, 4(1), 59-61
Food and Agriculture Organization of the United Nations [UN], & World Health Organization [WHO] (2003). Assuring Food Safety and Quality: Guidelines for Strengthening National Food Control Systems,_FAO Food and Nutrition Paper 76. A Joint FAO/WHO publication. http://www.fao.org/3/a-y8705e.pdf
Gaspard, J., & Yang, C. (2016). Training needs assessment of health care professionals in a developing country: The example of Saint Lucia. BMC Medical Education, 16, 1-6. https://bmcmededuc.biomedcentral.com/articles/10.1186/s12909-016-0638-9
Kenny, M., Ralph, S., & Brown, M. (2006) Lifelong learning, professional development and community work. Research in Post-Compulsory Education, 5(1), 51-62.
Marcinkiewicz, A., Cybart, A., & Chrominska-Szosland, D. (2002). Distance learning in postgraduate training of professionals: Example of occupational medicine specialization. Wiad Lek, 55(1), 330-334.
Ministry of Health Sri Lanka. (2016). National health strategic master plan 2016 -2025. Colombo, Sri Lanka: Ministry of Health
Moore, D. E., Green, J. S., & Gallis, H. A. (2009). Achieving Desired Results and Improved Outcomes: Integrating Planning and Assessment Throughout Learning Activities. Journal of Continuing Education in The Health Professions, 29(1), 1–15.
Murray, D. E., & Christison, M. (2018). Online Language Teacher Education: A Review of the Literature. Aqueduto, Norwich.
Price, S., & Reichert, C. (2017). The importance of continuing professional development to career satisfaction and patient care: Meeting the needs of novice to mid- to late-career nurses throughout their career span, Administrative Sciences, 7(2), 17. https://www.mdpi.com/2076-3387/7/2/17.
Schunk, D. H. (2012). Learning Theories, An Educational Perspective (6th Ed.). Boston, MA: Pearson Education, Inc.
Scott, S. G. (2010) Factors Impacting the Selection of Training-Delivery Systems and Training Methodology of Virginia Training Professionals (doctoral dissertation). Blacksburg, VA: Faculty of the Virginia Polytechnic Institute and State University.
Sherman, L. T., & Chappell, K. B. (2018). Global perspective on continuing professional development. The Asia Pacific Scolar, 3(2), 1-5.
Sri Lanka Accreditation Board for Conformity Assessment. (2013). Specific Criteria for Food Inspection, (Doc No. IB-GL(P)-03). Retrieved from http://www.slab.lk/Support/Publications/Inspection%20Bodies/IB-Specific-Criteria-for-Food-Inspection.pdf
World Health Organization. (2002). WHO Global Strategy for Food Safety: Safer food for better health. Retrieved from https://apps.who.int/iris/handle/10665/42559
*Mahendra Arnold
52/18, Pulinathalarama Road,
Magammana, Ragama, Sri Lanka
Tel: +94714199953
Email: mahendra_arnold@yahoo.com
Published online: 5 May, TAPS 2020, 5(2), 22-31
https://doi.org/10.29060/TAPS.2020-5-2/OA2173
Andrea Thompson1, Tanisha Jowsey1, Helen Butler1, Augusta Connor2, Emma Griffiths2, Hadley Brown2 & Marcus Henning1
1University of Auckland, New Zealand; 2Mercy Hospice, Auckland, New Zealand
Abstract
Objective: The aim of this study was to identify the impact of a series of palliative care educational packages on pharmacists’ practice for improved service delivery. We asked, what are the educator and learner experiences of a short course comprised of workshops and a series of palliative care learning packages, and how have learners changed their practice as a result of the course?
Method: Semi-structured interviews were conducted and transcribed verbatim. Interpretive thematic analysis was undertaken.
Results: Eight people participated in this study; five pharmacists who had completed learning packages in palliative care and three educators who facilitated teaching sessions for the learning packages. The teaching and assessment approaches were applied and transferable to the clinical setting. The teaching strategies stimulated engagement, enabling participants to share their ideas and personal experiences. Participants’ understanding of palliative care was improved and they developed confidence to engage in deeper conversations with patients and/or their families and carers. Although the completion of assessment for the learning packages enabled credit for continuing professional development, their impact on the long-term practice of pharmacists was not established.
Conclusions: The findings of this study suggest that interactive teaching methods assisted the interviewed pharmacists to further develop their understanding of palliative care, and communication skills for palliative care patients and/or their families/carers. Pharmacists were better equipped and felt more comfortable about having these potentially difficult conversations. We recommend educators to place more emphasis on reflective activities within learning packages to encourage learners to develop more meaning from their experiences.
Keywords: Palliative Care Education, Pharmacist, Hospice, Interactive Learning, Communication, Learning Packages
Practice Highlights
- The course studied informs pharmacists’ practice for improved service delivery.
- The course led to more meaningful palliative care conversations.
- Interactive teaching methods supports learner engagement.
- Educators sharing personal experiences supports learning.
I. INTRODUCTION
There have been recommendations in the literature for over 30 years that pharmacists should receive more education around end-of-life issues and care (Dickinson, 2013). While inadequate training and knowledge in palliative care leads to poor palliative care provision (Furstenberg et al., 1998; Vernon, Brien, & Dooley, & Spruyt, 1999), effective palliative education can positively transform care provision (Institute of Medicine, 2015).
Research shows that effective palliative care education for pharmacists can deepen their understanding of their role in symptom and therapy management and psychosocial care during end-of-life stages, including reducing death anxiety among patients (Atayee, Best, & Daniels, 2008; Dickinson, 2013; Needham, Wong & Campion, 2002). Learning about palliative care encourages collaboration and continuity in service provision, and appropriate, timely and individualised care (Dickinson, 2013). Additionally, with extra training, community pharmacists can become more actively involved in their palliative patients’ care, including providing patient education, prescribing advice to physicians and facilitating continuity between healthcare settings (O’Connor, Pugh, Jiwa, Hughes, & Fisher, 2011). Australian community pharmacists report that completing a flexible online palliative care education programme positively impacts their practice (Hussainy, Marriott, Beattie, Nation, & Dooley, 2010). Hussainy et al. (2010) recommend future educational courses to include face-to-face weekly workshops in order to increase participation. In New Zealand, undergraduate pharmacy students receive palliative care training and upon graduation they manage various palliative care needs. To booster pharmacist palliative care knowledge and communication skills, and in response to the call from Hussainy et al. (2010), in 2016, educators at a metropolitan hospice in New Zealand ran a short course for pharmacists. The authors, including the educator participants in this study, were not involved in the course design. Here we explore participant experiences of the course including application of new knowledge/skills to practice.
The seminal pedagogical approaches of Schön (1983), Kolb (1984) and Knowles (1984) are relevant. Learning occurs when professionals reflect on their tacit knowledge and make sense of their experiences; therefore reflective practice is a central pedagogical approach (Schön, 1983). With this in mind, opportunities for reflective practice ought to be integrated into the design of educational initiatives. Kolb’s (1984) experiential learning model suggests learners have a concrete experience and then reflect on it, enabling them to formulate abstract concepts and generalisations. Learners can then try out their new understanding through the process of active experimentation. The need to be self-directed, the role of the learner’s experiences, motivation, and readiness to learn are examples of assumptions embedded in Knowles’ adult learning theory (Knowles, Holton, & Swanson, 2015).
In this paper, we explore the course in terms of teaching delivery and learning. We undertook a small interpretive thematic study to explore the participants’ experiences of the course. It is important for educators to be involved in researching and reflecting on their own teaching (Henning, Hu, Webster, Brown & Murphy, 2015; Steinert, Cruess, Cruess, & Snell, 2005) and we therefore included the teaching staff as participants alongside learner participants in this study.
A. Research Questions
We asked, what are the educator and learner experiences of a short course comprised of workshops and a series of palliative care learning packages, and how have learners changed their practice as a result of the course?
II. METHODS
A. Participants and Description of Educational Intervention
Learner participants were pharmacists who were enrolled in the course. The course learning packages were part of Hospice New Zealand’s Fundamentals of Palliative Care education programme (Appendix A). Figure 1 outlines the mode of delivery and educational frameworks for the learning packages. A two-hour workshop was offered for each learning package and the participants were given access to online resources such as a workbook, pre-reading and reflection activities. Learners were required to complete the pre-reading and reflection activities prior to each workshop. Learners engaged in classroom-based teaching activities, which largely included group discussions. The total number of learning packages that each learner participant completed is shown in Appendix A.
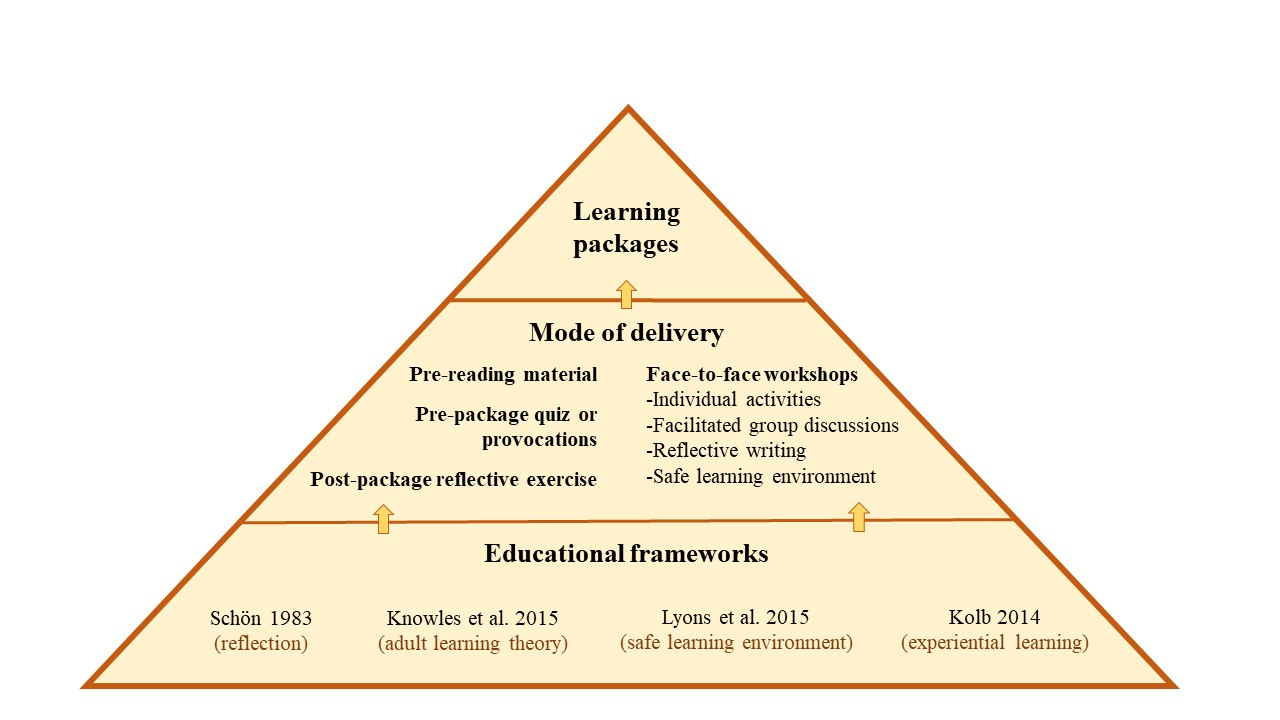
Figure 1. Mode of delivery and educational frameworks
Educator participants were three experienced facilitators (with pharmacy and nursing backgrounds) who were employed by the hospice. Each had an interest in education and had undertaken formal training sessions in palliative care delivery prior to facilitating the course.
B. Data Collection
Course educators and learners were invited via email to partake in a one-off face-to-face or phone interview to discuss their experiences of the course. One member of the research team (author 4) conducted all interviews following a semi-structured interview guide (Appendix B). Interviews were audio-recorded and transcribed verbatim. Data were collected between December 2016 and March 2017.
C. Data Analysis
Following Morse and Field (1995) and Saldaña(2016), we used general purpose interpretive thematic analysis. Transcripts were de-identified then uploaded into a qualitative data management system, QSR NVivo 11 software. Three members of the research team (authors 1, 2 and 7) read the transcripts and iteratively created a coding scheme. This involved looking for recurrent words, phrases and concepts within the data, which were termed codes. An initial coding scheme was developed iteratively containing primary codes, subsidiary codes and their definitions. There was a defined protocol for when to code the concepts. Two members of the research team (authors 1 and 2) independently coded each transcript and this coding was then checked by author 7 to ensure consistency and rigour. Two of our authors (3 and 5) were educator participants in this study. They were interviewed by a member of the research team, using the same questions posed to the third educator participant. To minimise bias, these authors were not involved in any aspect of the data analysis.
As the analysis progressed, some of the codes and sub-codes and their definitions were modified to ensure they conveyed the meaning participants had expressed during interviews. Assumptions about the relationships within and between concepts were proposed and explored. The codes were iteratively formed into themes and subthemes (Table 1). These themes were manually cross-checked for consistency. The QSR NVivo 11 software query functions were used to confirm relationships between themes and subthemes. These themes were discussed and refined between the three members of the analysis team.
|
Theme |
Subthemes |
|
A. Application to Practice |
1) Developing an understanding of palliative care 2) Developing empathy, listening and communication skills |
|
B. Learner Engagement |
1) Methods of teaching 2) Engagement – interactive style of teaching works 3) Drawing on personal experience 4) Feeling safe to share and learn |
|
C. Assessment and Evaluation |
1) The role of assessment and evaluation |
Table 1. Themes and subthemes of participant experiences
III. RESULTS
Eight females participated in this study, including five learners (course participants) and three educators. Their reflections on the course that they had attended as either an educator or learner rotated around three core themes: (1) application to practice, (2) learner engagement, and (3) assessment and evaluation (Table 1).
A. Application to Practice
Learner participants reported that the packages had increased their sense of preparedness for having real-life discussions with patients and family members/carers about death and dying/palliative care options, and ethical issues. Learners reported that this sense of preparedness had encouraged them to engage more deeply in conversations concerning palliative care.
1) Developing an understanding of palliative care: Educator and learner participants said the course enhanced their skills and understanding of communication with patients, their families/carers and other health professionals. Learners particularly valued information concerning the following subjects: the impact of a cancer diagnosis on significant others; medication; pharmacology; symptom and pain management; caring for palliative patients; ethical dilemmas; and dementia. A greater understanding of palliative care meant that learners reported they found they were able to make decisions about pharmaceuticals (without needing to check with another health professional), which they saw as likely to save time while maintaining quality of care. Further, learners’ understanding was influenced by the educators’ passion for teaching in the area of palliative care.
You might be thinking why on earth are they using Dexamethasone to increase this patient’s appetite – that doesn’t sound right. I need to ring the doctor. Whereas now they understand this is normal, this is the dose range, so they’re better equipped to supply the medication because they understand why. They’re not having to constantly ring the GP [general practitioner].
(Educator 1)
They [educators] know their topic inside out and they do their best to pass on … every ounce of knowledge that they have, which is great to see in colleagues. I just found it incredibly, inspiring to have that sort of passion for a topic.
(Learner 2)
2) Developing empathy, listening and communication skills: The learning modules enabled learner participants to develop awareness, empathy, and communication skills–particularly listening skills. They gave specific examples of empathic behaviour when dealing with patients and their families, for example, recognising and attempting to understand the multiple losses and life changes one might experience with a cancer diagnosis. Further, the content and delivery of the learning packages gave learners opportunities to be more prepared to engage in difficult conversations around death and dying.
It’s just being able to have more empathy for the people because you appreciate what they’re going through and what’s happening … just being a bit more available I suppose and realise in the end you spend time listening to what they have to say and trying to do the best for them.
(Learner 1)
And I guess when I’m talking to people, [recognising] that they’re going through a lot of losses and because of their cancer for example, they may have lost their job, I mean, if they can’t work anymore, their role in the family, they may have physical changes and loss around that.
(Learner 3)
The importance of ‘giving special time’ for conversation was an additional skill participants learned through completion of the modules. They recognised the importance of moving beyond the patient’s prescription and taking time to listen and engage in conversation with the patients and/or their families/carers.
Well actually at the time we had a customer–a man whose wife was dying of cancer, and I think instead of taking the prescription and things like that, you went out and took a special time and talked to them and spent a bit of time without actually asking too many specific questions.
(Learner 5)
In addition to communicating with patients and their families/carers, learner participants reported that the delivery of the learning modules helped equip and gave learners confidence to communicate more effectively with other health professionals.
“I deal a lot with rest homes and private hospitals so being able to assist the RNs [registered nurses] and to be able to relate to them.”
(Learner 2)
“And so, I sort of feel a lot more comfortable about that and comfortable talking to the doctors, you know, when something’s happening. So, I’ve learnt that.”
(Learner 4)
B. Learner Engagement
1) Methods of teaching: All participants discussed methods of teaching as having direct impact on their learning. Educator participants discussed teaching methods in more depth and greater frequency than pharmacist learner participants. They identified that when interactive strategies were utilised (videos, small group activities, case scenarios, demonstrations, and brainstorms), the learners absorbed/embedded more information and valued the teaching material more than when the information was presented didactically.
If I have to use a PowerPoint [slide presentation] I will learn it so that it’s behind me and I’m speaking to the audience and using eye contact, engaging from them their interest and whether they’re understanding. And I like to encourage questions to be asked as I’m talking because that then helps to add another layer of explanation. I also like case scenarios and preparing a case scenario or an ethical situation for groups to break off and discuss in their small groups and then to feedback so that each group can learn from everybody else.
(Educator 1)
The exception to this pattern was Educator 3’s observation that didactic teaching was an effective teaching strategy to begin the learning session, as it is a teaching format familiar to learners. Once the class was underway a more engaging method was needed.
“[Learners] were quite happy to be led initially, [using] didactic teaching. But I don’t think the sessions would have been as effective if we had continued that route.”
(Educator 3)
The relevance of content was also important to both the educator and learner participants. They valued material that was relevant and applicable to the pharmacists’ ‘specific care populations and practices of care.’
I was satisfied that I was able to provide consultant specialist advice and make it real for the pharmacists…. I put in a number of extra slides that were specific to pharmacists and some of the pharmacology of the drugs etcetera.
(Educator 1)
“It was kind of practical stuff [content] that you could easily translate when dealing with people when they came into the pharmacy.”
(Learner 1)
2) Engagement–Interactive style of teaching works: The teaching methods that learner participants had most to say about were interactive ones. This included facilitated whole-group conversation that was supported by small group activities.
There were a lot of different points of view and a lot of different people who were at different levels of experience in different areas and I think having the whole group there that were all pharmacists was really helpful. We all learned from each other.
(Learner 3)
In contrast, when educators discussed interactive teaching, they talked about it in terms of group dynamics and managing the discussions so that all learners had opportunity to voice their opinions.
There’s nothing worse than having somebody that just has to answer every question, has to share everything because they just need to be heard. So, you have to manage that and … manage the person that just sits there and doesn’t say anything.
(Educator 2)
3) Drawing on personal experience: Three educators and two learners reported that some educators drew on their personal experience–such as from the hospice pharmacist setting–to illustrate the relevance of material. When learners discussed their relevant personal experiences, it was equally valued.
“We all learned from each other.”
(Learner 3)
“We even had one pharmacist kind of stand up and say ‘This happened to me and I want you guys to learn from this’, so there was a lot of them talking about their experiences and sharing stuff.”
(Educator 3)
A learner reflected that the course material had value for her in her personal life.
I’d also gone through it [living and caring for a palliative care patient] with a flatmate early on and I felt that I hadn’t actually coped with it particularly well. So, it [the course] was a little bit for my own good as well.
(Learner 5)
Likewise, an educator made the observation that the course material was applicable to learners in their personal as well as their professional lives.
There was a strong feeling from pharmacists that they were also doing this to learn for their own personal lives because everybody will be touched by palliative care at some point in their lives, whether it be family or friends and it’s helped them to be better equipped with that.
(Educator 1)
The telling of personal experience can be linked with our first theme of Developing empathy, listening and communication skills. It is both telling and listening that comprises effective communication, which is core to pharmacist practices of care.
4) Feeling safe to share and learn: Feeling safe is important to supporting people’s learning. This was explicitly discussed by participants, and implicitly presented in other participants’ accounts.
She [Educator 2] talked to us, she encouraged you to give your opinion or your thoughts as well and you were never made to feel like what you said wasn’t right or was not significant. I thought she was great. It was very much an open forum, so you could relate, add bits in or ask questions and you felt comfortable doing that.
(Learner 4)
Educators were strategic in providing effective learning safe learning environments:
One of the skills of palliative care education is talking about topics that can be really quite difficult for some people if they’ve had a recent loss or they’ve had a situation in their personal life and it’ll trigger, so ground rules are really important to try and keep–to make sure people feel safe. So, you ensure when you start a session that people know that they can share stuff of a personal nature, but that information stays in the room and that it’s not to go outside. And you want people to be respectful.
(Educator 2)
C. Assessment and Evaluation
1) The role of assessment and evaluation: Educator participants highlighted the importance of assessment to enhance learning. Two assessment methods; reflective activities undertaken during the learning packages and quizzes completed at the end of the packages were formatively assessed methods. Educator participants pointed out there is a mechanism for assessment to be recognised by the Pharmaceutical Society of New Zealand. In this case, successful completion of assessment therefore becomes a summative assessment.
“[The] Pharmaceutical Society approves questions and if participants gain more than 80% then … the Society awards them learning points that contribute to their compulsory continuing education.”
(Educator 1)
Along with the assessment methods described, the Hospice NZ programme gives learners the opportunity to complete an evaluation which includes questions about learning value for each learning package. The inclusion of assessment and evaluation methods fosters learners to think about how process (teaching delivery) and content have contributed to their learning.
Although educators promoted the merits of assessment comprising part of the learning modules, they acknowledged that assessment gauges learning only in the short term. It is not possible to determine the long-term impact on practice from the assessment and evaluation methods currently utilised. Further, participants identified some confusion around the reflective activities.
“We struggle with assessing their learning long-term – what have they taken away a year later? What are they using in their practice? That’s what we haven’t been able to establish.”
(Educator 1)
“Participants appeared confused about the requirements for the pre and post session reflective activities which they were required to complete in the learning packages.”
(Learner 1)
IV. DISCUSSION
Effective palliative education for pharmacists enables participants to understand their role in end of life care, reduces death anxiety, prepares them to relate to people who are dying and facilitates psychological and emotional competence (Dickinson, 2013). It offers people knowledge and confidence to engage in the types of conversations that enrich peoples’ lives by making them feel heard and cared for. Dau Voire said, “be brave enough to start a conversation that matters” (Bravery Sayings & Bravery Quotes, n.d.). Is it bravery for pharmacists to engage patients in conversations about life and death? It absolutely is because the conversation may necessitate reflecting on your own life, mortality, and wishes.
We have shown that pharmacists valued this palliative care course because it developed key skills–and increased their bravery–to engage in deeper, more meaningful palliative care conversations in their professional and personal lives. We discuss the findings in turn.
A. Learning Engagement
Teaching delivery, which is primarily focused on interactive teaching methods such as small group activities, case scenarios, demonstrations, discussions and brainstorms markedly supported learner engagement. They valued opportunities to learn through discussing learner and educator experiences. These findings are consistent with Knowles’ adult learning theory, which suggests that the learners’ experiences ought to be tapped into (Knowles, et al., 2015). Teachers can help learners by using experiential techniques to acknowledge and utilise learners’ experiences through group discussions, activities to foster reflection, simulation exercises, and problem-solving activities (Knowles et al., 2015; Kolb, 1984; Schön 1983). In our view, one of the strengths of the learning packages is that they align with key educational frameworks (Figure 1).
Learners and educators in this study promoted a safe learning environment to optimise participation and learning (Lyons et al., 2015). This is echoed by existing education literature (Brown, 1988; Douglas, 1976). A safe climate, atmosphere or environment enables participants to feel comfortable about discussing personal experiences, including those which are difficult or challenging.
B. Assessment and Evaluation
When reflection is not encouraged in the clinical setting learning opportunities may be lost (Branch & Paranjape, 2002; Schön, 1983). In this course, learning was promoted through reflection and this was valued by learners, although they reported confusion about requirements for reflection activities. The opportunity for completion of modules to contribute to pharmacists’ continuing professional development (CPD) requirements was a key driver for participants completing the summative assessment. It is unlikely that meeting CPD requirements is the sole requirement for engaging in CPD. Further motivators for CPD may be to enhance professional knowledge and competence (Ryan, 2003).
C. Application to Practice
Several elements of the course were reportedly taken forward by participants to change their practices of care which had the flow-on effect of reducing their need to contact another health professional (for example, the patient’s general practitioner) to assist in decision-making processes. This improved the patient’s continuity of care. The value of palliative education is supported by the evaluation of an online programme in palliative care for pharmacists which demonstrated that the programme positively influenced the knowledge, confidence and practice of community pharmacists (Hussainy et al., 2010).
Delivery of the learning packages enabled pharmacists to develop a greater understanding of the impact of life-limiting illnesses and fostered both their development of empathy and ability to communicate with patients and their families and/or carers. The need for developing communication skills was strongly emphasised in a study which examined the community pharmacist’s role in palliative care (O’Connor et al., 2011). Emotional issues were seen as a major source of stress for general practitioners in an earlier study that identified the importance of the need for training and education to support general practitioners in managing emotional responses for palliative care patients and their families (O’Connor, Fisher, & Guilfoyle, 2006).
D. Limitations
Only females consented to participate in this study. We cannot speak to male pharmacist experiences of the course. The number of course participants was small and we had difficulty recruiting people to our study, partly because the interviews were held several months after the conclusion of the course. Our sample size was therefore small and our findings may not be generalisable. To increase study participation, future research of palliative care pharmacy courses could seek to recruit participants on workshop days or within a week of the course conclusion. Two of the authors on this paper were participants in the study. They were not involved in any aspect of the data analysis but they did contribute to the introduction and discussion sections of this article. The study did not establish the longer-term impact of the educational initiative on pharmacists’ practice. This is an opportunity for future research.
V. CONCLUSION
It is clear that effective palliative care education such as the learning packages discussed here is valued by pharmacists and relevant to their practice. Pharmacists in this study found the learning packages enhanced their understanding of palliative care, sharpened their communication skills and bolstered their confidence to engage in deeper conversations with patients and their families/carers and other health professionals. The interactive teaching methods promoted participant engagement and gave them opportunities to share their ideas and personal experiences and to listen to the experiences of others. Improving communication was a key feature for participants in this study. We therefore recommend that community pharmacists continue to be offered effective palliative care education, and that promotion of communication skills remain central to course method and content. An increased focus on critical reflection activities within such courses needs to be encouraged so that pharmacists can make meaning of their experiences and learning opportunities are not lost.
Notes on Contributors
Andrea Thompson is a Professional Teaching Fellow at the Centre for Medical and Health Sciences Education, University of Auckland.
Tanisha Jowsey is a medical anthropologist and a Senior Lecturer at the Centre for Medical and Health Sciences Education, University of Auckland.
Helen Butler was formerly employed at a Hospice in New Zealand and is now a Professional Teaching Fellow in the School of Nursing at the University of Auckland.
Augusta Connor, was formerly a research assistant at a Hospice in New Zealand and now works in health economics in the United Kingdom.
Emma Griffiths works at a Hospice in New Zealand as a specialist palliative care pharmacist.
Hadley Brown was formerly employed at a Hospice in New Zealand and is now self-employed. He has been involved in management within in the New Zealand hospice sector.
Marcus Henning is an Associate Professor at the Centre for Medical and Health Sciences Education, University of Auckland.
Ethical Approval
This study was approved by the University of Auckland Human Participants Ethics Committee (Reference Number: 016800).
Acknowledgements
We would like to acknowledge the participants who shared their experiences of teaching and learning.
Funding
A research assistant who conducted and transcribed the interviews was funded by Mercy Hospice, Auckland, New Zealand.
Declaration of Interest
Two authors were participants in the study. Although they were involved in the design of the study and contributed to writing the paper they were not involved in analysis of the data.
References
Atayee, R., Best, B., & Daniels, C. (2008). Development of an ambulatory palliative care pharmacist practice. Journal of Palliative Medicine, 11(8), 1077-1082. https://doi.org/10.1089/jpm.2008.0023
Branch, T., & Paranjape, T. (2002). Feedback and reflection: Teaching methods for clinical settings. Academic Medicine, 77(12), 1185-1188. https://doi.org/10.1097/00001888-200212000-00005
Bravery Sayings & Bravery Quotes (n.d.). Bravery sayings and quotes. Retrieved from http://www.wiseoldsayings.com/bravery-quotes/
Brown, G. (1988). Effective teaching in higher education. London: Methuen.
Dickinson, G. (2013). End-of-life and palliative care education in US pharmacy schools. American Journal of Hospice and Palliative Medicine, 30(6), 532-535. https://doi.org/10.1177/1049909112457011
Douglas, T. (1976). Groupwork practice. London: Tavistock Publications.
Furstenberg, C., Ahles, T., Whedon, M., Pierce, K., Dolan, M., Roberts, L., & Silberfarb, P. (1998). Knowledge and attitudes of health-care providers toward cancer pain management: A comparison of physicians, nurses, and pharmacists in the state of New Hampshire. Journal of Pain and Symptom Management, 15(6), 335-349. https://doi.org/10.1016/S0885-3924(98)00023-2
Henning, M., Hu, J., Webster, C., Brown, H., & Murphy, J. (2015). An evaluation of Hospice New Zealand’s interprofessional fundamentals of palliative care program at a single site. Palliative & Supportive Care, 13(3), 725-732.
Hussainy, S., Marriott, J., Beattie, J., Nation, R., & Dooley, M. (2010). A palliative cancer care flexible education program for Australian community pharmacists. American Journal of Pharmaceutical Education, 74(2), 1-9. https://doi.org/10.5688/aj740224
Institute of Medicine (2015). Committee on Approaching Death: Addressing, Key End-of-Life Issues. Dying in America: Improving quality and honoring individual preferences near the end of life. Washington, D.C.: National Academies Press.
Knowles, M. (1984). The adult learner: A neglected species (3rd Ed.). Houston: Gulf Pub. Co.
Knowles, M., Holton, E., & Swanson, R. (2015). The adult learner. (8th Ed.). New York: Routledge.
Kolb, D. (1984). Experiential learning: Experience as the source of learning and development. Englewood Cliffs, N.J.: Prentice-Hall c1984.
Lyons, R., Lazzara, E. H., Benishek, L. E., Zajac, S., Gregory, M., Sonesh, S. C., & Salas, E. (2015). Enhancing the effectiveness of team debriefings in medical simulation: More best practices. The Joint Commission Journal on Quality and Patient Safety, 41(3), 115. https://doi.org/10.1016/S1553-7250(15)41016-5
Morse, J. & Field, J. (1995). Qualitative research methods for health professionals (2nd Ed.). Thousand Oaks: Sage Publications.
Needham, D. S., Wong, I. C. K., & Campion, P. D. (2002). Evaluation of the effectiveness of UK community pharmacists’ interventions in community palliative care. Palliative Medicine, 16(3), 219-225. https://doi.org/10.1191/0269216302pm533oa
O’Connor, M., Fisher, C., & Guilfoyle, A. (2006). Interdisciplinary teams in palliative care: A critical reflection. International Journal of Palliative Nursing, 12(3), 132-137. https://doi.org/10.12968/ijpn.2006.12.3.20698
O’Connor, M., Pugh, J., Jiwa, M., Hughes, J., & Fisher, C. (2011). The palliative care interdisciplinary team: Where is the community pharmacist? Journal of Palliative Medicine, 14(1), 7-11. https://doi.org/10.1089/jpm.2010.0369
Ryan, J. (2003). Continuous professional development along the continuum of lifelong learning. Nurse Education Today, 23(7), 498-508. https://doi.org/10.1016/S0260-6917(03)00074-1
Saldaña, J. (2016). The coding manual for qualitative researchers (3rd Ed.). London: Sage.
Schön, D. (1983). The reflective practitioner. New York, NY: Basic Books.
Steinert, Y., Cruess, S., Cruess, R., & Snell, L. (2005). Faculty development for teaching and evaluating professionalism: From programme design to curriculum change. Medical Education, 39(2), 127-136.
Vernon, J., Brien, J., Dooley, M., & Spruyt, O. (1999). Multidisciplinary treatment paths and medication management of palliative care patients. Proceedings of the Australian Society of Clinical and Experimental Pharmacologists and Toxicologists, 7, 74.
*Andrea Thompson
University of Auckland,
Building 599, Level 12,
Auckland City Hospital
Private Bag 92019,
Auckland 1142
Tel: +6499231906
Email: andrea.thompson@auckland.ac.nz
Published online: 7 January, TAPS 2020, 5(1), 79-81
DOI: https://doi.org/10.29060/TAPS.2020-5-1/CS2092
Rajeev Ramachandran1, 2, Clarice Chong3 & Lee Gan Goh3
1Khoo Teck Puat – National University Children’s Medical Institute, National University Health System, Singapore; 2Department of Paediatrics, Yong Loo Lin School of Medicine, National University of Singapore; 3Department of Family Medicine, National University Health System, Singapore & Yong Loo Lin School of Medicine, National University of Singapore
I. INTRODUCTION
Family Medicine (FM) is an applied and integrative discipline. In 2011, the Ministry of Health introduced FM Residency Program in Singapore to train aspiring Family Physicians (FP). There are three sponsoring institutions, namely, Sing-Health Polyclinics, National Healthcare Group Polyclinics, and National University Health System (NUHS).
The Singapore FM Residency programs have rotations involving 13 disciplines, one of which is Paediatrics. As part of training in Paediatrics, the NUHS program has set up an outpatient Paediatric Longitudinal Clinic (PLC) staffed by FM Residents. This PLC is a service cum training clinic. It is supervised jointly by a Paediatrician core-faculty and a FM core-faculty. The FM Residency program aims at training a FP to provide primary, personal, and preventive care; and comprehensive, continuing and coordinated care to the patient and their family (Goh & Ong, 2014).
We report a case study of using a patient with a genetic syndrome to illustrate the Family Medicine approach in the training of the FP in a FM Residency Program. This Approach consists of the 3 Ps (personal, primary, and preventive care) to define care needs; and 3Cs (comprehensive, continuing and coordinated care) in managing the patient and family.
II. OBJECTIVE AND METHODS
The objective of this paper is to illustrate the potential of using FM approach in managing a patient with a rare multi-system genetic disorder. This teaching event took place at the PLC. The patient was clerked by the FM resident on duty. The one-year-old patient who looked dysmorphic to us (having microcephaly, broad thumbs and great toes, poor growth, and mental slowness), presented with constipation. The resident discovered that he was regularly seeing a neonatologist, neurologist, dietitian and gastroenterologist for the multiple problems he was having.
Using the FM approach, we defined the patient’s primary, personal, and preventive care needs and formulated a comprehensive, continuing, and coordinated care approach in managing the patient and family. Through this approach we hoped to reduce fragmentation of care, duplication of services, and forestall complications through preventive care.
III. LEARNING POTENTIAL FOR THE FM RESIDENT
All three subspecialists managing this patient have worked independently of one another. The neonatologist with the help of a dietitian was following up the patient for failure to thrive. The height and weight centiles were < 3% and this did not improve with nutritional intervention. The neurologist was following up for microcephaly and gastroenterologist was treating the patient for constipation. In this particular instance, it was the constipation that brought the patient to Children’s Emergency and she was followed up by us in the PLC a week later.
During the case discussion with the FM Resident, the General Paediatrician recognized that microcephaly, broad thumbs and great toes are prominent features of Rubinstein-Taybi syndrome which is a genetic syndrome. The FM faculty encouraged the resident to read about this condition and find out if the presentation of the patient matches with what is described in text books as well as explore the strategies to reduce fragmentation of care and work with various members of the health care team to increase the integration of care (Newbronner, Borthwick, Finn, Scales, & Pearson, 2017; Starfield, Shi, & Macinko, 2005). In the follow-up discussion, the patient’s care needs of the 3Ps (primary care, personal care, and preventive care needs) were defined. With a better understanding of the genetic syndrome, the FM Resident was able to formulate the 3Cs of management care needs (comprehensive, continuing, and co-ordinated care) of the patient and family. Table 1 shows the scope of the 3Ps and 3Cs in this case study (Gandhi, 2016).
|
| Source: Gandhi, 2016 |
Table 1. Components of the family medicine approach in the clinical case of a patient with genetic syndrome
IV. DISCUSSION
The FM approach in the integration of care in Paediatrics is illustrated in this case study of a genetic syndrome. The potential of using such a clinical case is rich. What is also important is the paradigm shift from the focus of studying biomedical features of syndromic rarities to integrate care of the patient.
The Rubinstein-Taybi syndrome (Gandhi, 2016) encountered in this patient is one example of a genetic syndrome that can be used to teach the scope and breadth of the FM approach. There are other genetic syndromes that can be used, e.g., the patient with Trisomy 21; Duchenne progressive muscular atrophy, or Spinal muscular atrophy (SMA).
Some of the day-to-day medical problems found in such genetic syndromes can be dealt with by the Family Physician alone, e.g., constipation. Other problems may need shared care of two or more clinical disciplines, as for example, the care for mental retardation, skeletal abnormalities, organ abnormalities, and slow physical growth. These are common features encountered in genetic syndromes.
The 3Ps: Defining the primary, personal, and preventive care needs of the patient.
Primary care is first level care. Constipation is an outpatient problem that the FP can help.
Personal care is important in connection with monitoring growth and development and providing acute care for common problems. The FP needs to help the patient and family define the tasks and provide recommendations where these are needed.
Preventive care has its role too. The preventive treatment of constipation, orthopaedic problems, mental stimulation, can be jointly coordinated by the FP and the Paediatric subspecialists (neonatologist, neurologist, and gastroenterologist in this case study).
The 3Cs: Managing the comprehensive care, continuing care, and coordinated care needs of the patient and family.
Comprehensive care spans the physical domain of the patient’s clinical features, social domain of the patient (parents, helpers) which will include the caregivers who need to know the medical condition that the child is having, as well as symptoms and treatment that will be needed e.g. constipation, schooling, and other life-course preparation for the child. The treatment of this condition is based on symptoms.
Continuing care is needed. In view of the multisystem involvement, anticipatory care may be needed e.g., dental care, intellectual and social development needs of the child.
Co-ordination of care is also needed. The child is under the care of the neonatologist, neurologist, and gastroenterologist. The FP could certainly co-ordinate the care between the specialists and in this way reduce duplication of care.
V. MOVING FORWARD
The Family Medicine Approach in teaching the management of the patient with a genetic syndrome shifts the focus from learning just biomedical rarities to teaching a system of defining the care needs that can be remembered as 3Ps; and the management of these needs as the 3Cs.
Through the co-ordination of care, reduction in fragmentation and duplication of care can be achieved and the inter-professional collaborative practice helps to deliver high quality, safe patient-centred services to achieve best possible long term health outcomes. Through prevention, some of the complications of multi-system diseases can be reduced.
Notes on Contributors
Rajeev Ramachandran, MD, FAAP, is an American Board certified General Paediatrician and Senior Consultant in the Department of Paediatrics, National University Hospital, Singapore and a Core Faculty for the Family Medicine Residency Program, National University Health Systems, and Singapore. He conceived this construct and intervention, wrote the manuscript, and agreed to its publication in its final form.
Clarice Chong, MBBS, MMED (Family Medicine), was a Family Medicine resident at the Family Medicine Residency Program, National University Health Systems, Singapore. She has since passed her MMed. (Family Medicine) specialty examination. She conceived this construct and intervention and agreed to its publication in its final form.
Goh Lee Gan, MMED (Internal Medicine), FCFP(Singapore), FRCGP, FRACGP, is a Senior Consultant and Professorial Fellow in the Department of Family Medicine, National University Hospital, Singapore and Associate Program Director for the Family Medicine Residency Program, National University Health Systems, Singapore. He conceived this construct and intervention, wrote the manuscript, and agreed to its publication in its final form.
Acknowledgements
We thank Dr Dimple Rajgor for her assistance in formatting, reviewing, and in submitting the manuscript for publication.
Funding
No funding is involved in this paper.
Declaration of Interest
There is no conflict of interest, including financial, consultant, institutional or otherwise for any of the authors involved in this manuscript.
References
Gandhi, A. (2016). Rubinstein-Taybi Syndrome. Retrieved from https://patient.info/doctor/rubinstein-taybi-syndrome-pro
Goh, L. G., & Ong, C. P. (2014). Education and training in family medicine: Progress and a proposed national vision for 2030. Singapore Medical Journal, 55(3), 117-23. https://doi.org/10.11622/smedj.2014031
Newbronner, E., Borthwick, R., Finn, G., Scales, M., & Pearson, D. (2017). Creating better doctors: Exploring the value of learning medicine in primary care. Education for Primary Care, 28(4), 201-209. https://doi.org/10.1080/14739879.2016.1277789
Starfield, B., Shi, L., & Macinko, J. (2005). Contribution of primary care to health systems and health. The Milbank Quarterly, 83(3), 457-502. https://doi.org/10.1111/j.1468-0009.2005.00409.x
*Rajeev Ramachandran
NUHS Tower Block Level 12,
1E Kent Ridge Road,
Singapore 119228
Tel: + 65 6772 3615
Fax: +65 67797486
Email: rajeev_ramachandran@nuhs.edu.sg
Announcements
- Best Reviewer Awards 2024
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2024.
Refer here for the list of recipients. - Most Accessed Article 2024
The Most Accessed Article of 2024 goes to Persons with Disabilities (PWD) as patient educators: Effects on medical student attitudes.
Congratulations, Dr Vivien Lee and co-authors! - Best Article Award 2024
The Best Article Award of 2024 goes to Achieving Competency for Year 1 Doctors in Singapore: Comparing Night Float or Traditional Call.
Congratulations, Dr Tan Mae Yue and co-authors! - Fourth Thematic Issue: Call for Submissions
The Asia Pacific Scholar is now calling for submissions for its Fourth Thematic Publication on “Developing a Holistic Healthcare Practitioner for a Sustainable Future”!
The Guest Editors for this Thematic Issue are A/Prof Marcus Henning and Adj A/Prof Mabel Yap. For more information on paper submissions, check out here! - Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Volume 9 Number 1 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors. - Volume 8 Number 3 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2021
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2021.
Refer here for the list of recipients. - Most Accessed Article 2021
The Most Accessed Article of 2021 goes to Professional identity formation-oriented mentoring technique as a method to improve self-regulated learning: A mixed-method study.
Congratulations, Assoc/Prof Matsuyama and co-authors. - Best Reviewer Awards 2020
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2020.
Refer here for the list of recipients. - Most Accessed Article 2020
The Most Accessed Article of 2020 goes to Inter-related issues that impact motivation in biomedical sciences graduate education. Congratulations, Dr Chen Zhi Xiong and co-authors.









