Dental education continuity during the COVID-19 pandemic – Experience at National Dental Centre Singapore
Submitted: 27 January 2021
Accepted: 1 April 2021
Published online: 5 October, TAPS 2021, 6(4), 131-134
https://doi.org/10.29060/TAPS.2021-6-4/SC2478
Lean Heong Foo & Marianne Meng Ann Ong
Department of Restorative Dentistry, National Dental Centre Singapore, Singapore
Abstract
Introduction: The novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has caused the COVID-19 pandemic which started in 2020. This resulted in a disruption to educational activities across the globe. Dental education, in particular, was affected because of its vocational nature where learners come into close contact with patients when performing dental procedures.
Methods: This is a narrative review with no research data analysis involved.
Results: Social distancing measures introduced to curb the spread of the infection revolutionised the advancement of online education as the virtual environment is a safer place to conduct teaching compared to face-to-face teaching. In this article, we share our experience at the National Dental Centre Singapore (NDCS) in ensuring the safety of our faculty and learners when conducting didactic and clinical education during the pandemic. Didactic lectures were conducted in the virtual environment via synchronous and non-synchronous teaching. Essential clinical education was conducted in small groups with safe management measures in place. In addition, we provide guidelines to highlight the importance of meticulous planning, thorough preparation, and seamless delivery in conducting effective synchronous teaching.
Conclusion: Safe management measures put in place to ensure the well-being of our faculty and learners can ensure dental education continuity during the pandemic.
Keywords: Dental Education, Education Continuity, COVID-19
I. INTRODUCTION
The COVID-19 pandemic is severely affecting dental professionals since the Department of Labor Occupational and Health Administration United States of America (USA) published guidelines associating aerosol-generating procedures (AGP) in dentistry with SARS-CoV-2 virus spread. Many dental schools in the USA and Asia Pacific have desisted clinical practice and simulation sessions, causing severe disruption in dental training (Chang et al., 2021). Innovative guidelines were developed to conduct dental education during the pandemic (Hong et al., 2021). Singapore has undergone five phases during the pandemic: Pre-pandemic, Circuit Breaker (CB), Phase 1, Phase 2, and Phase 3 (current). We share our experience in continuing dental education for oral healthcare team learners (residents, dental technicians trainees, dental assistant trainees) in NDCS during the pandemic.
II. CLINICAL ADJUSTMENTS
After the Ministry of Health Singapore (MOH) raised the Diseases Outbreak Response System Condition (DORSCON) level from yellow to orange on 7th February 2020 (Pre-pandemic), NDCS senior management immediately adopted team segregation by establishing three self-contained teams comprising clinicians, dental surgery assistants, lab technicians, patient service associate executives, and health attendants (Tay et al., 2020). Learners at NDCS were also assigned to teams. All staff and learners were briefed on safe management measures to observe during clinical sessions. They were required to wear a surgical mask at all times except during meals, perform hand hygiene with an alcohol-based hand sanitiser, and report their temperature twice daily online. Triage and risk assessment of patients were carried out (Hong et al., 2021; Tay et al., 2020) and dental procedures were limited to emergency procedures to relieve pain, ongoing dental treatment, and dental clearance before medical procedures during CB. Use of personal protective equipment (PPE) comprising an eye shield, N95 mask or respirator, surgical gown, and gloves were indicated for all AGP while the use of an eye shield, surgical mask, and surgical gown was indicated for non-AGP following a risk-based assessment (Tay et al., 2020). Patients with suspected COVID-19 or who had close contact with a confirmed case were treated in a negative pressure room with proper PPE. All patients were required to rinse with cetylpyridinium chloride mouth rinse before their procedure. A 15-minute window in between patients was implemented to disinfect the operatory until Phase 3.
III. EDUCATION PROGRAMME ADJUSTMENTS
We conduct three structured education programmes in NDCS–National Institute of Technical Education (NITEC) Dental Assisting (DA), NITEC Dental Technology (DT), and National University of Singapore Master of Dental Surgery Residency Training Programme (RTP) for six dental specialties. In addition, Singapore Institute of Technology (SIT) Diagnostic Radiography (DR) students have observation attachments at NDCS. During CB, Phase 1, and Phase 2, we postponed the new intake of learners for DA due to logistic issues with our collaborators. The posting of DR learners to our centre was also halted. All existing DA and DT learners were allocated to the same clinical team and completed their programme during the pandemic. Residents in the RTP were divided into two groups; one group was based in NDCS and the other in National University Centre for Oral Health Singapore during the 7-week CB. From Phase 1 onwards, the two groups of residents started weekly alternating rotations for their clinical sessions between the two institutions.
NDCS education activities are classified into didactics and clinical sessions. We conducted didactics using synchronous and non-synchronous formats while clinical sessions gradually resumed from Phase 1 to 3 following prevailing MOH and institutional policies. Synchronous teaching and seminars were carried out using Zoom and WebEx online platforms. Voice annotated presentations and e-learning modules were launched in the SingHealth e-learning platform, Wizlearn, for non-synchronous teaching. Clinical sessions were conducted with a small clinical supervisor-learner ratio (1:5), triage of patients, use of complete PPE with an N95 mask, hand hygiene, and high suction evacuator for AGP (Tay et al., 2020). Face-to-face sessions for essential hands-on clinical skills building were organised in Phase 2 and 3 with safe management measures in place such as small instructor-learner ratio, safe distances between learners and instructors, segregation of learners and instructors in groups, donning of surgical masks, meticulous hand hygiene, and proper disinfection after equipment use (Tay et al., 2020).
IV. GUIDELINES FOR ONLINE SYNCHRONOUS TEACHING
Mayer’s theory of multimedia learning (Mayer, 2002) describes the learning process in online education by highlighting the dual channels (auditory and visual) and three stages of memory (sensory, working, and long-term) for processing information. The learner’s eyes and ears capture diagrams and text in the multimedia presentation with sensory memory input. These are converted into a pictorial and verbal mode respectively in the working memory and integrated with prior knowledge from the long-term memory. Educators should prevent cognitive overload in content planning, as learners have limited capacity to hold the pictorial and verbal mode in working memory. A three-phase guide highlighting salient information for conducting effective online synchronous teaching is provided.
A. Meticulous Planning
To understand learners, faculty can adopt a 5W and 1 H concept [(who (the learners), where (location of teaching), why (learning objectives), what (lesson content), when (duration), and how (online platform in this context)] when planning a teaching module. Besides, faculty can construct the learning objectives and teaching activities using Bloom’s taxonomy based on learning outcomes. Bloom’s taxonomy covers six cognitive domains in the following order: knowledge, comprehension, application, analysis, synthesis, and evaluation, where a higher-order is more complicated for the learners to master and demonstrate.
B. Thorough Preparation
Apart from teaching material, a faculty guide is recommended. It should contain the schedule and details of the teaching session, teaching activities, and probing questions and answers for reference; to ensure all the teaching tasks are completed within the planned schedule. Handouts are used to reduce cognitive overload and as a backup when the connection is down. Generally, a good camera, laptop or smartphone, internet connection, a simple background with light, and a quiet room are sufficient for online teaching.
C. Seamless Delivery
Good online synchronous teaching platforms include Zoom, WebEx, Microsoft Teams, Google Meet, Mikogo, and Slack with breakout rooms and annotation board features that are included in the premium subscription of these platforms. A dry run is recommended to familiarise oneself with the functions on the various platforms. Setting the learning climate during the session by preparing learners to respond at appropriate times is crucial. The faculty should look at the camera frequently to keep eye contact with learners. Backup plans that include standby internet access and soft copy handouts are useful when connection is down. Increased feedback and communication between faculty and learners is crucial in online teaching and can be achieved by:
i) Using a learning management system such as GoSoapBox to allow learners to input text individually, particularly useful for clinical case discussion.
ii) Using Slido or Poll Everywhere to conduct needs analysis or summative or formative assessment between teaching.
iii) Utilising the question and answer segment to assess learners’ responses and check progress.
iv) Using the chatbox to allow learners to post questions and comments.
Teleconferencing has limited non-verbal cues coupled with milliseconds delay in observation by other participants that can subconsciously force our brain to restore the synchrony present in face-to-face contact. This overworking can lead to tiredness and discomfort from virtual teleconferencing tools, termed as ‘Zoom fatigue’. Recommendations to reduce Zoom fatigue include taking a rest in between brief lessons and turning off the camera when muted to reduce stimulus and mental fatigue. Netiquette, a blend of ‘internet etiquette’, refers to a code of good behaviour for both educators and learners (Table 1) that should be practised in an online environment (Lateef, 2020) to promote courteous communication between learners and educators for a pleasant learning experience. Evaluation of online education can be conducted during the session by performing formative and summative assessment; assessing quality and completion rate of learners’ assignment; analysing learners feedback from the post-session questionnaire as well as learners’ grade during module assessment and performance in the clinic.
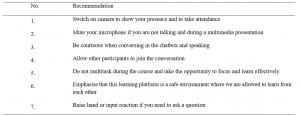
Table 1. Netiquette for online education
Note: Adapted from “Computer-based simulation and online teaching netiquette in the time of COVID 19,” by F. Lateef, 2020, EC Emergency Medicine and Critical Care, 4(8), 84-91.
V. MOVING FORWARD
It may take years to return to pre-COVID-19 normalcy, where physical interaction and large gatherings were social norms. Moving forward, we can consider a hybrid or blended learning module alongside limited face-to-face sessions confined to essential skill-based training. However, the effectiveness of online learning compared to traditional modes of clinical teaching has not been elucidated. Dentistry is a practical vocation that requires developing surgical and psychomotor skills to perform specific tasks. Online learning addresses the delivery of didactics but translating theory into practice which involves hands-on skills, teamwork and communication are challenging in the virtual setting. Virtual and augmented reality programmes such as Spatial, coupled with simulation video demonstration, may be suitable for skill-based training in dental education in the virtual environment. Psychological support for faculty and learners and forming a digital technology community of practice among educators can help to improve resilience and coping mechanisms during this challenging period. With safe management measures in place to ensure the well-being of our faculty and learners, we can adapt and continue education activities while looking for innovative ways to deliver clinical teaching effectively in dentistry amidst this pandemic.
Notes on Contributors
Dr Lean Heong Foo is a Consultant Periodontist in the Department of Restorative Dentistry and Head to the Dental Surgery Assistant Certification Programme. FLH reviewed the literature, contributed to the conception, data acquisition, drafted and critically revised the manuscript.
Dr Marianne Meng Ann Ong is a Senior Consultant Periodontist & Director of Education in National Dental Centre Singapore. MO contributed to the conception, data acquisition and critically revised the manuscript. All authors gave their final approval and agree to be accountable for all aspects of the work.
Ethical Approval
This is a narrative review related to dental education continuity during the COVID-19 pandemic and no ethical approval is required.
Data availability
This paper is a narrative review with no data analysis.
Acknowledgement
The authors would like to thank Ms Safiyya Mohamed Ali for providing editorial support.
Funding
There is no funding involved in the preparation of the manuscript.
Declaration of Interest
The authors declare no conflict of interest.
References
Chang, T., Hong, G., Paganelli, C., Phantumvanit, P., Chang, W., Shieh, Y., & Hsu, M. (2021). Innovation of dental education during COVID-19 pandemic. Journal of Dental Sciences, 16(1), 15-20. https://doi.org/10.1016/j.jds.2020.07.011
Hong, G., Chang, T., Terry, A., Chuenjitwongsa, S., Park, Y., Tsoi, J. K., Kusdhany, M. F. L. S., Egusa, H., Yamada, S., Kwon, J., Seow, L., Garcia, M. C. A. G., Wong, M. L., Ayuchai, P., & Hsu, M. (2021). Guidelines for innovation in dental education during the coronavirus disease 2019 pandemic. Journal of Oral Science, 63(1), 107-110. https://doi.org/10.2334/josnusd.20-0399
Lateef, F. (2020). Computer-based simulation and online teaching netiquette in the time of COVID 19. EC Emergency Medicine and Critical Care, 4(8), 84-91.
Mayer, R. E. (2002). Multimedia learning. Psychology of Learning and Motivation, 41, 85-139.
Tay, J. R. H., Ng, E., Ong, M. M. A., Sim, C., Tan, K., & Seneviratne, C. J. (2020). A risk-based approach to the COVID-19 pandemic: The experience in National Dental Centre Singapore. Frontiers in Medicine, 7. https://doi.org/10.3389/fmed.2020.562728
*Foo Lean Heong
National Dental Centre Singapore
5, Second Hospital Avenue,
168938 Singapore
Email: foo.lean.heong@singhealth.com.sg
Announcements
- Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Volume 9 Number 1 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors. - Volume 8 Number 3 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2021
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2021.
Refer here for the list of recipients. - Most Accessed Article 2021
The Most Accessed Article of 2021 goes to Professional identity formation-oriented mentoring technique as a method to improve self-regulated learning: A mixed-method study.
Congratulations, Assoc/Prof Matsuyama and co-authors. - Best Reviewer Awards 2020
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2020.
Refer here for the list of recipients. - Most Accessed Article 2020
The Most Accessed Article of 2020 goes to Inter-related issues that impact motivation in biomedical sciences graduate education. Congratulations, Dr Chen Zhi Xiong and co-authors. - Scopus
TAPS has been accepted for inclusion in Scopus! - Best Reviewer Awards 2019
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2019.
Refer here for the list of recipients. - Most Accessed Article 2019
The Most Accessed Article of 2019 goes to A two-edged sword: Narrative inquiry into Japanese doctors’ intrinsic motivation. Congratulations,
Professor Hiroshi Nishigori and co-authors!









