Residents’ expectations and perceptions of clinical teaching activities in National Dental Centre Singapore
Published online: 7 May, TAPS 2019, 4(2), 52-57
DOI: https://doi.org/10.29060/TAPS.2019-4-2/SC2035
Marianne Meng Ann Ong1 & Sandy Cook2
1Department of Restorative Dentistry, National Dental Centre, Singapore; 2Academic Medicine Education Institute, Duke-NUS Medical School, Singapore
Abstract
Aim: To describe residents’ expectations of faculty using the One-Minute Preceptor (OMP) in microskills and their ratings of faculty performing them during clinical sessions.
Methods: Prior to the start of residency, residents were invited to participate in a survey on residents’ expectations of faculty performing the OMP microskills in clinical teaching activities using a 4-point Likert scale. At the end of Year 1, they rated faculty on their use of the OMP microskills using a 4-point Likert scale using a second survey.
Results: Sixteen Year 1 residents completed the first survey and 15 residents completed the second survey. Prior to residency, correcting mistakes with feedback was the highest rated microskill (3.78) and obtaining a commitment was the lowest rated (3.15). At the end of Year 1, residents rated faculty performing getting a commitment as the highest (3.63) and giving feedback the lowest (3.17).
Conclusion: In this small cohort of residents, expectations were high around the OMP microskills. Residents felt faculty performed them well in their first year of residency. However, residents view of the importance of the five OMP microskills by faculty differed from their perception of how well the faculty demonstrated them. Future studies could explore if residents’ perceptions of importance changed over time or were related to their view on the quality of performance by faculty. Faculty will be further encouraged to employ the five OMP microskills to maximise their teaching moments with residents managing patients in busy outpatient clinics in National Dental Centre Singapore.
Keywords: Learner Perception, Expectation, Evaluation, Clinical Teaching
I. INTRODUCTION
Some challenges faced by learners and faculty in clinical teaching include work demands, time constraints, multiple levels of learners and lack of active participation of learners (Spencer, 2003). The use of the One Minute Preceptor (OMP) in microskills in clinical teaching has been shown to be easy to learn and effective in helping faculty improve their teaching (Furney et al., 2001) in addition to maximising their teaching moments with learners in busy outpatient clinics (Neher, Gordon, Meyer, & Stevens, 1992). The OMP framework consists of five microskills: obtaining a commitment (OAC); probing for supporting evidence (PSE); teaching general rules (TGR); providing positive feedback (PPF); and correcting mistakes with feedback (CMF). Depending on the situation, each microskill can be used either on its own or in any sequence to cater to different learning contexts. Earlier studies done in National Dental Centre Singapore (NDCS) assessed whether OMP in microskills faculty development workshops had an impact on in-flight residents’ perceptions of clinical teaching (Ong, Yow, Tan, & Compton, 2017) and obtained information on past residents’ perceptions on the importance and frequency of the OMP microskills in residency clinics (Ong, Woo, & Cook, 2016). However, we found no studies in the literature that explored incoming dental residents’ expectations of faculty using the OMP microskills during clinical sessions in their residency programmes, nor their perceptions of faculty performing them in their first year of the programme. This descriptive study thus describes Year 1 residents’ expectations and perceptions of clinical teaching activities performed by faculty.
II. METHODS
A. Study Design
This is a descriptive study on residents’ expectations and perceptions of clinical teaching activities performed by faculty. The protocol was sent to SingHealth CIRB (Ref: 2018/2137) and it was deemed exempt from review.
B. Subjects
During the Academic Year (AY) 2015 orientation session in June 2015, prior to the start of residency programmes, all sixteen residents in five dental specialities (Endodontics, Oral and Maxillofacial Surgery, Orthodontics, Periodontics and Prosthodontics) were invited to participate in this survey.
C. Surveys
Two surveys were developed to explore Year 1 residents’ expectations and perceptions of clinical teaching activities in relation to the OMP microskills. The first survey (PRE) (refer Appendix A) had 14-items grouped by the microskills: OAC (3 items), PSE (3 items), TGR (3 items), PPF (3 items) and CMF (2 items). Residents rated the importance they placed on faculty engaging in teaching activities related to them on a 4-point Likert scale (1= not important to 4= very important).
The second survey (POST) (refer Appendix B), administered at the end of their first year (June 2016), had 13-items that were also grouped by the microskills: OAC (4 items), PSE (3 items), TGR (2 items), PPF (2 items) and CMF (2 items). While similar in the microskills classification as the PRE survey, these items were focused on how well faculty performed them on a 4-point Likert scale (1= inadequate to 4= excellent) and included slightly different phrasing. Both survey items were reviewed by 2 residents in Year 2 of their residency programmes for relevance, ease of use, language and clarity of items.
D. Administration of Surveys
At the AY 2015 orientation session, paper copies of the PRE survey were handed out to residents after the overview briefing session of NDCS residency training programmes by the Director of Education. At the end of Year 1, during the annual programme evaluation session, paper copies of the POST survey were handed out to residents to fill in by an Academic Clinical Programme (ACP) office executive.
E. Data Analysis
The PRE and POST survey data were collated by an executive in the ACP office. De-identified data were sent to the staff of Duke-NUS Office of Education to provide basic descriptive statistics. Individual items in each microskill category for both surveys were averaged to get a general sense of the residents’ views by category. No further statistical analysis was done as different rating scales were used and there was slight variation in the phrasing of items in both surveys.
III. RESULTS
Sixteen Year 1 residents (100% response rate) completed the PRE with overall mean ratings of importance ranging from 3.15 (OAC) to 3.78 (CMF) for the five microskills (Figure 1). Fifteen residents (93.75% response rate) completed the POST (1 resident dropped out of a residency programme before the end of Year 1) with overall mean ratings of quality ranging from 3.17 (PPF) to 3.63 (OAC) (Figure 1).
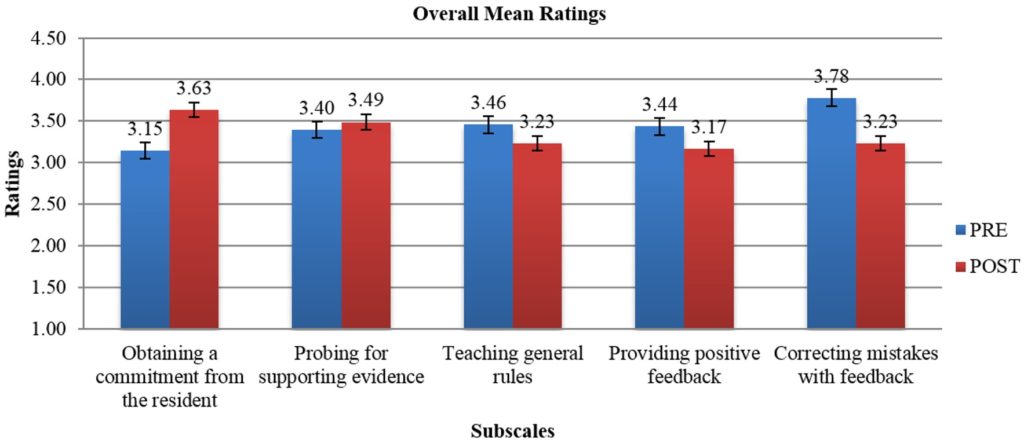
Note: While the broad categories are similar, rating scales and individual items that were averaged by microskills category were different on each survey. The PRE scale was 1=not important to 4=very important. The POST scale was 1=inadequate to 4=excellent).
Figure 1. Overall mean ratings on the importance of OMP activities (PRE) and mean ratings on quality of faculty performing OMP activities (POST)
IV. DISCUSSION
In this study, clinical teaching was defined as performance of teaching activities related to OMP microskills. Residents in this cohort rated faculty CMF (PRE: 3.78) as the element of most importance of the five OMP microskills prior to the start of residency. Yet, it was not one of the OMP microskills rated as done well (POST: 3.23) as the rest. This is an area NDCS faculty can improve upon. The OMP microskill rated as best performed by faculty was OAC (POST: 3.63), was actually the least important to residents (PRE: 3.15). But overall residents perceived faculty performing the five OMP microskills well (>3.0) in clinical teaching.
Earlier data obtained from past learners in the residency programmes from a 2015 general survey done in NDCS had revealed they valued the use of the OMP microskills in clinical teaching. The two microskills with the highest mean ratings on importance were OAC and CMF (Ong et al., 2016). The frequently demonstrated microskills in that survey were OAC and TGR. In contrast, a survey done with in-flight residents in 2014 exploring the short-term follow up after an OMP in microskills workshop for faculty, had revealed TGR as the most adequately performed microskill by faculty (Ong et al., 2017). The differences in perceptions in OMP microskills in clinical teaching by faculty can be attributed to the different cohorts of learners surveyed at different periods of time. It is not unexpected that learners at various stages of their residency would have different expectations and perceptions of the five microskills in clinical sessions.
Limitations of this study include its small sample size, residents responded to survey items based on their own subjective expectation of faculty demonstrating the OMP microskills in clinical teaching and their own subjective assessment of how well faculty performed them during their first year of residency in the clinics. The nature of the study, different rating scales and variation in the phrasing of the survey items limited our ability to determine any change in perceptions on importance and quality in the OMP microskills.
V. CONCLUSION
In this small cohort of residents, expectations were high around certain of the OMP microskills. Residents felt the faculty performed them well. However, residents view of the importance of the five OMP microskills by faculty differed from their perception of how well the faculty demonstrated them. Future studies could explore if residents’ perceptions of importance changed over time or were related to their view on the quality of performance by faculty. Faculty will be further encouraged to employ the five OMP microskills in clinical teaching to maximise their teaching moments with residents managing patients in busy outpatient clinics in NDCS.
Notes on Contributors
Dr Marianne M. A. Ong, Cert Perio (Michigan), MS (Michigan); Adjunct Associate Professor, Duke-NUS Medical School, Singapore; Senior Consultant & Director, Education National Dental Centre Singapore.
Dr Sandy Cook, PhD; Senior Associate Dean, Deputy Head of Office of Education; Deputy Director, Academic Medicine Education Institute; Professor, Duke-NUS Medical School.
Ethical Approval
The protocol was sent to SingHealth CIRB (Ref: 2018/2137) and was deemed not requiring a formal review as it reports on residents’ expectations and perceptions of clinical teaching activities performed by faculty and satisfaction with their first-year experience.
Acknowledgements
The authors would like to give special thanks to Ms Kia-Mun Woo from the MD Programme Department for her help in the data analysis.
Funding
The authors have not received any funding or benefits from industry or elsewhere to conduct this study.
Declaration of Interest
The authors have no conflict of interest.
References
Furney, S. L., Orsini, A. N., Orsetti, K. E., Stern, D. T., Gruppen, L. D., & Irby, D. M. (2001). Teaching the one-minute preceptor: A randomized controlled trial. Journal of General Internal Medicine, 16(9), 620-624.
https://doi.org/10.1046/j.1525-1497.2001.016009620.x
Neher, J. O., Gordon, K. C., Meyer, B., & Stevens, N. (1992). A five-step “microskills” model of clinical teaching. Journal of the American Board of Family Practice, 5(4), 419-424. Retrieved from https://www.jabfm.org/content/5/4/419
Ong, M. M., Woo, K. M., & Cook, S. (2016). A general survey on learners and faculty perspectives on educational activities held in the National Dental Centre, Singapore. Proceedings of Singapore Healthcare. 25(3), 158-168.
https://doi.org/10.1177/2010105816642246
Ong, M. M., Yow, M., Tan, J., & Compton, S. (2017). Perceived effectiveness of one-minute preceptor in microskills by residents in dental residency training at National Dental Centre Singapore. Proceedings of Singapore Healthcare, 26(1), 35-41. https://doi.org/10.1177/2010105816666294
Spencer, J. (2003). Learning and teaching in the clinical environment. British Medical Journal, 326(7389), 591-594. https://doi.org/10.1136/bmj.326.7389.591
*Marianne Ong
Department of Restorative Dentistry
5 Second Hospital Avenue, Singapore 168938
National Dental Centre Singapore
Tel: +65 63248925
E-mail: marianne.ong.m.a@singhealth.com.sg
Announcements
- Best Reviewer Awards 2024
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2024.
Refer here for the list of recipients. - Most Accessed Article 2024
The Most Accessed Article of 2024 goes to Persons with Disabilities (PWD) as patient educators: Effects on medical student attitudes.
Congratulations, Dr Vivien Lee and co-authors! - Best Article Award 2024
The Best Article Award of 2024 goes to Achieving Competency for Year 1 Doctors in Singapore: Comparing Night Float or Traditional Call.
Congratulations, Dr Tan Mae Yue and co-authors! - Fourth Thematic Issue: Call for Submissions
The Asia Pacific Scholar is now calling for submissions for its Fourth Thematic Publication on “Developing a Holistic Healthcare Practitioner for a Sustainable Future”!
The Guest Editors for this Thematic Issue are A/Prof Marcus Henning and Adj A/Prof Mabel Yap. For more information on paper submissions, check out here! - Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Volume 9 Number 1 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors. - Volume 8 Number 3 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2021
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2021.
Refer here for the list of recipients. - Most Accessed Article 2021
The Most Accessed Article of 2021 goes to Professional identity formation-oriented mentoring technique as a method to improve self-regulated learning: A mixed-method study.
Congratulations, Assoc/Prof Matsuyama and co-authors. - Best Reviewer Awards 2020
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2020.
Refer here for the list of recipients. - Most Accessed Article 2020
The Most Accessed Article of 2020 goes to Inter-related issues that impact motivation in biomedical sciences graduate education. Congratulations, Dr Chen Zhi Xiong and co-authors.









