Proposal for What-If Kiken-Yochi Training (risk prediction training) Patient Safety Education Design: Improve risk assessment of medical students
Published online: 7 January, TAPS 2020, 5(1), 61-69
DOI: https://doi.org/10.29060/TAPS.2020-5-1/OA2152
Yoshitaka Maeda1, Yoshikazu Asada2, Yoshihiko Suzuki1 & Hiroshi Kawahira1
1Medical Simulation Centre, Jichi Medical University, Japan; 2Center for Information, Jichi Medical University, Japan
Abstract
Students in the early years of medical school should learn the skills of clinical site risk assessment. However, the effect of this training on clinically inexperienced students is not clear, and it is difficult for them to predict risks from a wide range of perspectives. Therefore, in this study, based on Kiken-Yochi Training (KYT) for risk prediction using what-if analysis, we examined how to expand risk prediction among clinically inexperienced medical students. We divided 120 students in the first year of medical school into small groups of seven to eight students. First, each group predicted risks in the standard KYT (S-KY) method, stating what risks exist in the illustrations. Next, they conducted a What-If KYT (W-KY) analysis, brainstorming situations that differed from the illustrations, and again conducted risk prediction. Three kinds of illustrations depicting medical scenes were used. Last, each student proposed solutions to prevent risks. In this study, we clarify differences in risk assessment tendencies for students between W-KY and S-KY. We found that students could predict a wide variety of risks about illustrations using W-KY, particularly risks about patient and medical personnel. However, for risks regarding management, clinical rules, and stakeholders, prediction in both S-KY and W-KY was difficult due students’ lack of knowledge, but solutions proposed by students covered these elements. Improving the format of discussion in W-KY might allow students to predict risk from a wider range of perspectives.
Keywords: Patient Safety Education, Undergraduate Education, Risk Assessment Skill, Kiken-Yochi Training, KYT, Risk Prediction, Clinically Inexperienced Medical Students
Practice Highlights
- This method helps inexperienced students brainstorm various scenarios needed for risk prediction.
- It was possible for students to practice risk assessment using What-If Kiken-Yochi Training (W-KY).
- Students could predict a wide variety of risks regarding patients and medical personnel using W-KY.
- It was difficult to predict management, clinical rules, and stakeholders’ risks even with W-KY.
I. INTRODUCTION
A. Issues on Patient Safety Education for Medical Students in Japan
In Japan, students enrol at medical schools immediately after graduating from high school. Safety education is often provided only at higher levels (4th or 5th year) in over 60% of medical schools in Japan, when clinical practice begins (Ishikawa, Hirao, & Maezawa, 2008). The following are the reasons: (1) educational practical methods for clinically inexperienced students are not specifically referred to in any guidelines or papers for students in the early years; (2) the educational effect on such students is unclear; (3) higher grade students have sufficient medical knowledge and can immediately apply their patient safety knowledge in clinical practice; and (4) there are few teachers specialising in medical safety, thus making it easier to determine the theme of education for higher grade students. On the contrary, 70% of medical schools only teach the minimum medical safety knowledge through lectures to students who have not yet practiced safety in clinical practice. The main contents of the lectures are analysis tools to prevent the recurrence of incidents, such as Root Cause Analysis and Failure Mode and Effects Analysis, legal responsibility knowledge, ethics, and infection (Mayer, Klamen, Gunderson, & Barach, 2009). However, as there are certain things that can be included immediately in clinical practice, it is difficult to keep students motivated.
The Telluride Interdisciplinary Roundtable (Mayer et al., 2009) and Lucian Leape Institute (2010) indicated that patient safety education should be conducted through a longitudinal curricular approach (including patient safety education in the curriculum of all grades), and it is important to educate lower grade students who have no clinical experience. This would enable students to learn the necessity and importance of patient safety knowledge, and to consider patient safety as implementation science while continuously practicing patient safety skills (Nakajima, 2012). Ishikawa et al. (2008) also emphasised the importance of continuous patient safety education, starting with beginner students so they can acquire good safety habits.
The Telluride Interdisciplinary Roundtable (Mayer et al., 2009) and Lucian Leape Institute (2010) outlined the patient safety competencies that students should acquire. In particular, students lack education on “non-technical skills” (Nakajima, 2012). Some of the necessary non-technical skills students need when they start working after graduation are risk assessment (situational awareness) skills to prevent accidents. This involves advance awareness of safety weaknesses and threats (risks) in the workplace or operations and the ability to avoid these risks (Doi, Kawamoto, & Yamaguchi, 2012; Takahashi, 2010). The World Health Organization’s (WHO’s) Patient Safety Curriculum Guide shows in Topic 6 (Understanding & Managing Clinical Risk) that students have to take correct action when they see an unsafe situation or environment (Walton et al., 2010). For example, when they see wet steps, they should predict the possibility of patients falling. WHO’s guide outlines the four-step process to manage clinical risks: (1) identify the risk, (2) assess the frequency and severity of the risk, (3) reduce or eliminate the risk, and (4) assess the costs saved by reducing the risk versus the costs of not managing the risk. However, this guide does not explain the teaching methods to enable students to identify or predict risks.
B. Educational Method Issues for Risk Assessment in Japan
Kiken-Yochi Training (KYT), a type of risk prediction training, was created by Sumitomo Metal Industries Co., LTD in 1974 (Chen & Mao, 2011), and helps workers understand risks in many kinds of industries, including the medical field (Doi et al., 2012; Hirokane, Shiraki, & Ohdo, 2010). KYT originated in Japan (Ito, Taguchi, & Fujinami, 2014) and has become a common safety management method (Ji, 2014). It increases workers’ awareness of risks and motivation to practice in a team and improves their problem-solving skills (Chen & Jin, 2012). KYT also enables workers to easily conduct on-site risk assessment. In a metal auto parts factory, the accident rate fell by six percent one year after the implementation of KYT (Poosanthanasarn, Sriboorapa, Fungladda, & Lohachit, 2005). In recent years, KYT use has also begun to spread in the medical field in countries other than Japan (Noor, Irniza, Emilia, Anita, & Suriani, 2016). In standard KYT (S-KY), the facilitator presents the learner with illustrations or photographs depicting the work site and guides them through four steps: (1) extracting items and risks considered to be dangerous in the illustration, (2) rating each item’s risk, (3) planning solutions, and (4) selecting urgent solutions (Japan Industrial Safety & Health Association, 2008). In particular, an important skill for medical staff at clinical sites is the ability to predict a myriad of risks from a broad perspective using the illustration in Step 1. More effective KYT has recently been designed, such as KYT using video instead of illustrations and KYT applications for tablets that enable students to easily take risk assessment training alone, such as during breaks, and KYT combining medical simulations of real clinic situations (Kadoyanagi, 2016; Nagamatsu, Miyazaki, & Harada, 2011; Takahashi et al., 2017; Yoneda et al., 2017).
However, in S-KY, the ability of experts to predict risks is higher than that of novices because novices do not have enough knowledge of important areas in the illustrations (Murata, Hayami, & Moriwaka, 2009). Hirokane et al. (2010) pointed out that experts are able to predict risks specifically in order to consider effective solutions to prevent accidents. Therefore, KYT is usually conducted for clinically experienced students, and is rarely implemented for inexperienced students. The reasons are as follows: (1) in S-KY, risk prediction in the illustrations is limited to “specific circumstances”; (2) if medical students practice risk prediction using only these illustrations, they cannot accurately identify risks at clinical sites when they encounter a situation different from the “specific circumstances” in the illustration in the future; and (3) if teachers use illustrations of scenes from non-medical sites to avoid the inability to predict risks in clinically inexperienced students who do not have enough medical knowledge, it is difficult for students to link the risk prediction content with actual clinical sites, to become motivated to learn, and to obtain educational effects from the training.
C. Hypothesis: What-If KYT (W-KY) Applicability
What-If analysis is used as a brainstorming method. It is widely used in the field of service design and brainstorms what kind of things will occur if a particular situation changes (Stickdorn & Schneider, 2012). Based on this method, Mochizuki and Komatsubara (2016) propose a step 0 prior to the existing risk assessment in KYT that is aimed at traffic safety, letting the participants identify various alternate situations: “If the situation of the illustration were different”. Next, the participants perform a risk assessment for each situation developed in Step 0. For example, the facilitator shows participants illustrations depicting sunny daytime “driving scenes on a straight road”. Participants conduct what-if brainstorming and consider various situations, such as “if the weather is different from the illustration”, “if it was night-time”, or “if it is a mountain pass”. They then conduct a risk assessment for each situation. This modification is called the W-KY. The subsequent steps are the same as the S-KY (Steps 1 to 4). By adding Step 0, participants are then better able to predict various risks from the illustrations, and their risk sensitivity increases.
Based on these articles related to S-KY and W-KY, S-KY might be more feasible for clinically experienced students than inexperienced students. Therefore, W-KY might be feasible for clinically inexperienced students, because the What-If analysis (Step 0) might help students’ brainstorming. It also might increase motivation to practice and improve students’ problem-solving capabilities. The central question of this paper is whether the W-KY is effective and feasible for clinically inexperienced students. Existing studies have not adopted the W-KY to medical treatment, and the effect on clinically inexperienced students is unclear.
D. Purpose of This Study
In this study, based on the W-KY, we propose and implement a training method to help clinically inexperienced students predict risks. We also clarify differences in the risk assessment tendencies of students in W-KY versus the S-KY.
II. METHODS
A. Methods in W-KY
We conducted the S-KY and W-KY for 120 medical students half a year after admission in 70-minute compulsory classes. The purpose of these classes was to teach diversity of thinking and thinking of others through discussions in small groups of seven to eight people. The S-KY and W-KY were conducted over two classes (140 minutes). Specifically, the students conducted group work in the following order using three kinds of illustrations (Figure 1) depicting clinical sites. In our class, after individual students brainstormed ideas, they shared ideas with others and learned about the diversity of ideas.
Figure 1. Illustrations used in S-KY and W-KY (Courtesy of Japan Industrial Safety & Health Association [n.d.])
Step 1 (S-KY Step): Individual students predicted what risks exist in the three illustrations, then they used posters to share their prediction results with the group.
Step 2 (W-KY Step): Individual students brainstormed “situations that differed from the illustration” for each of the three illustrations. For example, in Illustration 1, one student thought of “a situation in which only one person was guiding the gurney”.
Step 3 (W-KY Step): Individual students predicted what risks exist in the situations they brainstormed in Step 2, then shared the results in their groups using posters.
Step 4 (S-KY and W-KY Steps): Each student considered solutions to mitigate the risks that they had predicted and submitted a report on them at the end of the class. Specifically, each student selected one risk considered to be the biggest risk in each illustration, and considered three solutions to prevent the risk.
B. Clarification of Differences in Risk Assessment Tendency of Students Between W-KY and S-KY
We compared the prediction results of S-KY in Step 1 and W-KY in Step 3 using the P-mSHELL model (Kawano, 2002). This model shows that factors of medical incidents are patient, management, software, hardware, environment, and liveware (individuals/ teams). P-mSHELL represents the initials of these factors. To evaluate the effectiveness of safety education, it is necessary to ensure that risks related to Human Factors can be predicted from a broad viewpoint. There are several models that explain the cause of Human Factors issues: Lewin’s equation model (human behaviour is determined by factors related to the person and their environment; Lewin, 1936), the 4M model (factors related to Man, Machine, Media, and Management), and Reason’s categories (factors related to patient and provider; task, technology, and tool; and team, environment, and organisation; Reason, 1997). All models consider both human and environmental factors as the background of Human Factors issues. Among these models, P-mSHELL is a highly detailed model that explains human and environmental factors in medicine, thus making it easy to evaluate the effectiveness of safety education. The P-mSHELL model is based on the SHEL model that has been used in analysis of Human Factors issues in aviation. Molloy and O’Boyle (2005) pointed out this model is useful in examining errors in clinical site, and may have some potential in training medical staff about Human Factors. Therefore, the P-mSHELL model is frequently referenced to understand human error in medical care. It is expected that the target students of this research will be able to predict the safety weaknesses (risks) in the clinical site from the point of view of P-mSHELL and to take preventative solutions. For this reason, this study verifies the educational effect by comparing the danger predicted by S-KY and W-KY using this model. We also summarise student brainstorming results in Step 2 “regarding situations that differ from the illustration” and examine its effect on student risk assessment. Then, we classify the solutions described in the report by students from the point of view of P-mSHELL.
C. Ethical Considerations in This Research
Regarding the ethical use of the results of S-KY and W-KY conducted in the class for research, we emphasised and explained to students that cooperation in this study was voluntary and that declining to cooperate would have no influence on their grades. We explained that students’ grades are scored based on the rubric described in the syllabus and that consent to cooperate in the research could be withdrawn at any time. It was explained that the results of this study may be published after processing, but the student’s personal information would not be revealed in the publication. The students entered their consent to use the results of S-KY and W-KY for this research in the e-learning system, Moodle, and 120 out of 123 students agreed to participate. In this research, we analysed data from students who agreed to participate. This study was considered exempt by the Jichi Medical University Review Board (protocol number 18-014).
III. RESULTS
A. Results of Predicted Risk by S-KY and W-KY
Figure 2 (left) shows the total number of risks predicted by students for each illustration. In addition, Figure 2 (right) shows the average number of predicted risks for each student group. We clarified the difference between S-KY and W-KY using the students’ t-test.
First, students were able to predict a variety of risks regardless of whether S-KY or W-KY was used. With the exception of liveware (team) in Illustration 3, the risks for all elements of P-mSHELL were predicted. In addition, the risks varied widely in the ease of prediction by the illustration (Figure 2, left). In Illustration 1, patient, environment, and liveware (individual) risks were predicted in S-KY and W-KY. In Illustration 2 predicted risks were liveware (person), and in Illustration 3, patient. Risks related to management, software, and liveware (team) were very few in both S-KY and W-KY, and for some illustrations, student groups predicted no risks in some categories.
Despite W-KY being implemented after S-KY, patient and environment risks had approximately the same number in S-KY and the W-KY. The number of liveware (individual) and hardware risks predicted in W-KY was less than in S-KY—liveware (individual): t(16) = 3.47, p < .05; Hardware: t(16) = 3.44, p < .05. In W-KY, many were predicted in Illustrations 1 and 2.
For example, in scenario 1, risks such as, “staff transferred patient to the wrong room” and “the patient would be injured if the stretcher breaks” were predicted in S-KY. In W-KY, risks such as, “If the corridor is dark, staff are not able to notice changes in the patient’s condition”, “If the corridor gets wet, the stretcher may slip and fall”, “If the patient is elderly, the patient will fracture a bone due to impact”, “If the patient has dementia, he forgets about treatment when he wakes up and removes the infusion tube himself”, and “If the staff is busy, he forgets to change the drip, emptying the drip and harming the patient” were predicted.
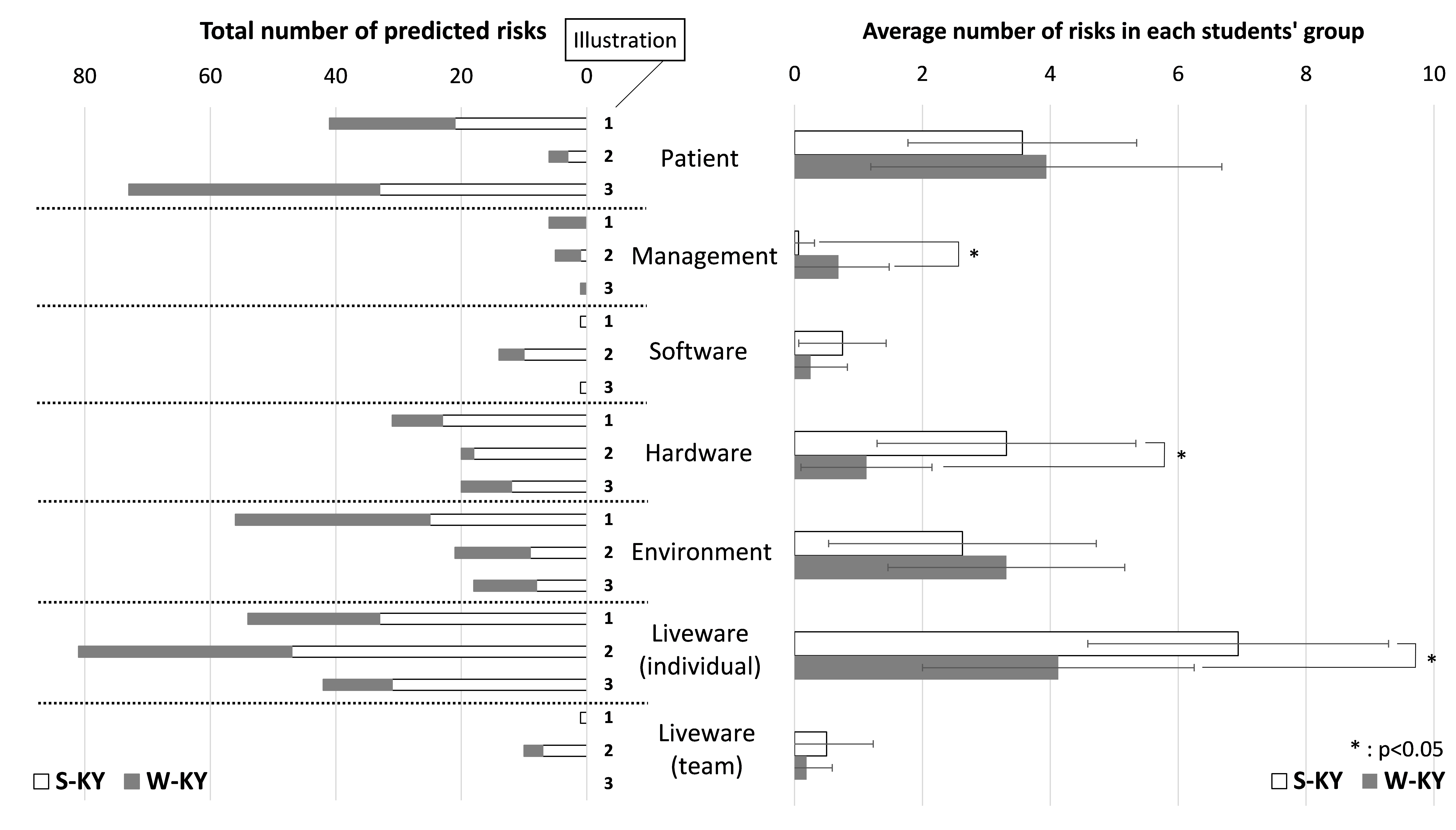 Figure 2. Result of predicted risk by S-KY and W-KY (Based on the classification of P-mSHELL)
Figure 2. Result of predicted risk by S-KY and W-KY (Based on the classification of P-mSHELL)
B. Results of Brainstorming Situations That Differed from the Illustration in Step 2
Table 1 shows how the students brainstormed situations that differed from each illustration in Step 2 as mentioned in the Methods section (refer to A. Methods in W-KY). In Table 1, the situations brainstormed by the students are organised based on each element of P-mSHELL.
First, the situations brainstormed by the students were remarkably diverse regarding patient, liveware (individual), hardware, and environmental factors. Although the number of liveware (individual) and hardware risks predicted in W-KY were less than in S-KY, the liveware (individual) risks predicted in W-KY were diverse.
On the other hand, the situation about management, software and liveware (team) were small in number (Table 1). This is also reflected in the low number of risks predicted for these factors (Figure 2).
| Description in the illustration | Situations brainstormed by students (in W-KY) | |
| Patient | One adult patient | Infants, elderly patients, infections, dementia, allergies, acute diseases, tall, obese patient, angry, sleeping, turning over many times, excited, removing the tube, patient with the same name exists, the patient’s family (child) is present, the operation is refused for religious reasons |
| Management | N/A | Staff shortage |
| Software | Directions | Mistaken, hard to read handwriting |
| Hardware
|
Gurney | Broken, screw loose, unstable |
| Bed | Narrow, nurse call button is broken | |
| Drip stand, tube | Fall, break, clogged tube, multiple drops exist | |
| Environment | Corridor | Crowded, wet in the rain, slippery, narrow, blackout |
| Room | Dark, bumpy, flickering, large number of patients | |
| Workspace | Messy | |
| Liveware (individual) |
One nurse | Fatigue, poor health, infection, lack of sleep, after working late, rushing, novice, lack of technology, lack of knowledge, presbyopia |
| Liveware (team) |
Nurse | Does not exist, bad relationship, noisy |
Table 1. Results of brainstorming in Step 2 about “situation different from illustration”
C. Solutions Proposed by Students to Mitigate the Risks
In Figure 3, the solutions proposed by the students to mitigate the risks were classified by P-mSHELL. In addition, Table 2 shows a concrete example of solutions for each element. In this paper, it has not been possible to analyse what kind of solutions were considered for each risk in S-KY and W-KY because students considered solutions in a post-class report.
In both S-KY and W-KY, students were able to consider a wide variety of solutions for almost all P-mSHELL factors. Although predicted risks related to management, software, and liveware (team) were very few, students were able to propose a lot of solutions related to them. There were many solutions, especially for software and hardware. For example, for software, double-checking, pointing and calling (occupational safety method), and creating a checklist were suggestion; in hardware, changing the shapes and names of the medicine in order to make it difficult to make mistakes was proposed.
| Patient | Patient participation Patient education Counseling, informed consent |
| Management | Work-life balance Rest management Staffing |
| Software | Creation of procedures (patient transport, patient fixation, dispensing, medication, patient assistance, etc.)
Examination of check method (pointing and calling, etc.) Efficiency of preparation work |
| Hardware
|
Improvement of hospital facilities
Improvement and computerisation of medical records and prescriptions Change of medicine shape and name Automation |
| Environment | Sorting Setting-in-order Shining Standardising Sustaining the discipline |
| Liveware (individual) |
Education and training Counseling Studying medical knowledge Attention/concentration Multitasking prevention Qualifications |
| Liveware (team) |
Good communication Thorough double check Establish a contact system |
Table 2. Examples of solutions considered by students
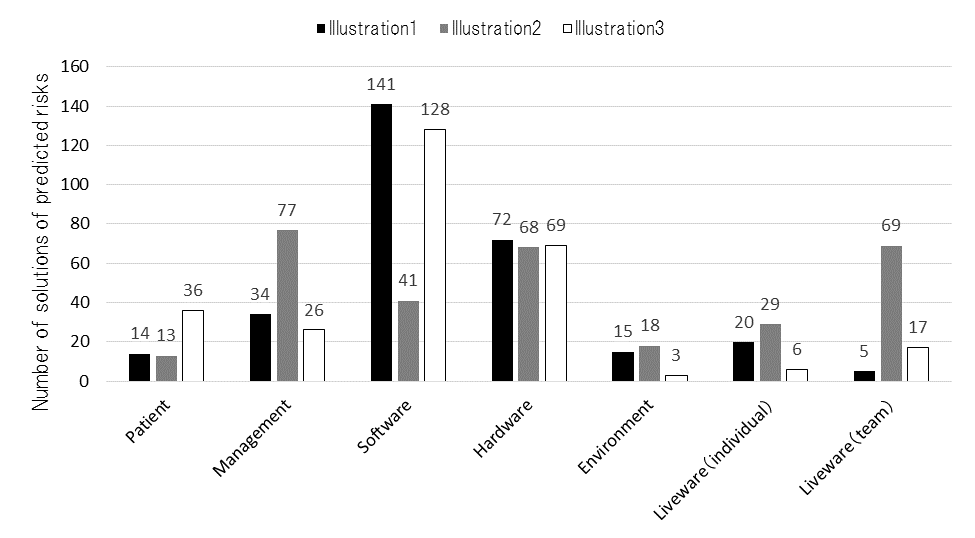 Figure 3. Result of solutions of predicted risks (based on the classification of P-mSHELL)
Figure 3. Result of solutions of predicted risks (based on the classification of P-mSHELL)
IV. DISCUSSION
A. Similarity and Difference Between S-KY and W-KY
Students should be able to predict risks in all elements of P-mSHELL as they can minimally experience the risks of each element in a clinical site. The results show that the elements of risk in P-mSHELL in both S-KY and W-KY are similar. Students could predict many patient and environment risks. These elements were drawn in advance in each illustration as shown in Figure 1. In other words, it was possible for students to brainstorm risks regarding stakeholders and medical devices drawn in illustrations in S-KY and W-KY. One of the possible reasons students could predict several patient and environment risks is that even a clinically inexperienced medical student has experience as a patient or has experienced the same situation (e.g., fatigue, immorality, lack of knowledge, etc.) as liveware (individual). Kazaoka, and Otsuka (2003) indicate that nursing students tend to recognise risks that they can imagine as their own and consider important, such as liveware (individual). On the other hand, management, software, and liveware (team) risks were very few in both S-KY and W-KY. The number of patient, environment, management, software, and liveware (team) risks had approximately the same number in S-KY and W-KY. The number of liveware (individual) and hardware risks in W-KY was less than in S-KY. In other words, it is considered that W-KY may cover the risks that can be predicted with S-KY.
Next, we discuss the strengths of W-KY. The risk description by students in W-KY included the risks and information related to various situations. Particularly in W-KY, students were able to brainstorm a wide variety of situations regarding patient, liveware (individual), hardware, and environmental risks (Table 1). This tendency is the same as the risk prediction tendency of S-KY and W-KY, and the reason for this tendency is considered to be the same. In W-KY, for example, regarding the transporting of stretchers, inexperienced students could consider various dynamic situations that can cause accidents, such as wet corridors, crowded corridors, violent or acutely ill patients, and lack of human resources. These situations that students brainstormed, listed in Table 1, are paraphrased as medical accident risks. In other words, in S-KY, students predict only medical accidents related to illustrations (results of accidents), whereas in W-KY, students were able to predict many high-risk situations that can cause medical accidents, and medical accidents (possible cause and results of accidents).
Through W-KY, students may have learned what a high-risk situation is and that clinical tasks can change into various dynamic situations that differ from illustrations. As a result, they may have learned the necessity of risk prediction in clinical practice and the significance of learning patient safety. These points will be explored in future research. In addition, Hirokane et al. (2010) pointed out that it is very important to predict risks specifically to prevent accidents. Therefore, it is possible that even inexperienced students can do this by using W-KY.
B. Limitations of W-KY
Only few students could predict risks management, software, and liveware (team) in S-KY and W-KY. However, students were able to consider solutions for almost all P-mSHELL factors (Figure 3). Contrary to the results of predicting risks in W-KY and S-KY, students were able to propose many solutions related to the aforementioned elements. This means that students can brainstorm these elements. In particular, regarding the software, students can mention the establishment and thoroughness of rules and manuals when planning solutions, and can think sufficiently from that viewpoint. Therefore, improving the format of discussion in W-KY may allow students to predict risks from a wider range of perspectives.
V. CONCLUSION
In this research, we proposed and implemented a training method to help clinically inexperienced students predict various risks. W-KY (brainstorming situations in illustrations and predicting risks based on them), as implemented in this research, allowed clinically inexperienced students to predict risks. We found that the elements of risk in P-mSHELL in both S-KY and W-KY are similar. Students could predict many patient and environment risks. However, with regard to management, software, and liveware (team) factors, S-KY and W-KY appeared to be difficult.
In addition, W-KY enables the prediction of high-risk situations that can cause medical accidents. This is important for predicting risks—including possible causes of accidents—specifically to prevent accidents.
In summary, W-KY can cover the risks that can be predicted by S-KY, and also allows students to consider various dynamic high-risk situations that can cause accidents. This suggests that W-KY can be used instead of S-KY.
In this study, it was not possible to analyse what kind of solutions to prevent risks were considered for each risk in S-KY and W-KY, as students considered solutions in a post-class report. Because this study was conducted as part of the class, we could not obtain data of student perspectives on learning outcomes or transferring learning to practice. The first-year medical school students in this research have the opportunity to receive medical safety education again when they are in the fourth year. At that time, we have plans to provide opportunities for practicing skills by applying W-KY in clinical practice, which will be explored in a future research. In addition, comparisons between students with clinical experience and inexperienced students and between W-KY/S-KY and other educational programs on accident prevention are also future topics of this research.
Notes on Contributors
Yoshitaka Maeda, PhD, is a research associate at the Medical Simulation Center at Jichi Medical University, Japan. He conducted the research supervision, class implementation, and data analysis.
Yoshikazu Asada, PhD, is an assistant professor at the Center for Information at Jichi Medical University, Japan. He contributed to the data compilation regarding the effect of this education.
Yoshihiko Suzuki, MD, is an assistant professor at the Medical Simulation Center at Jichi Medical University, Japan. He contributed to the design and planning of this class.
Hiroshi Kawahira, MD, is a professor at the Medical Simulation Center at Jichi Medical University, Japan. He gave advice on writing this paper and on data aggregation.
Ethical Approval
This study was approved by the Jichi Medical University Institutional Review Board (Protocol number 18-014).
Funding
There is no funding involved for this paper.
Declaration of Interest
The authors report no conflict of interest. The authors alone are responsible for the content and writing of this article.
References
Chen, Q., & Jin, R. (2012). Safety4Site commitment to enhance jobsite safety management and performance. Journal of Construction Engineering and Management, 138(4), 509-519. http://doi.org/10.1061/(ASCE)CO.1943-7862.0000453
Chen, N., & Mao, Y. (2011). Specific statistics and control method study on unsafe behavior in Chinese coal mines. Procedia Engineering, 26, 2222-2229. https://doi.org/10.1016/j.proeng.2011.11.2428
Doi, T., Kawamoto, K., & Yamaguchi, K. (2012). Difference in the level of patient treatment safety analysed by the years of experience of the radiological technologies. Nihon Hoshasen Gijutsu Gakkai zasshi [Japanese Journal of Radiological Technology], 68(5), 608-616. http://doi.org/10.6009/jjrt.2012_jsrt_68.5.608
Hirokane, M., Shiraki, W., & Ohdo, K. (2010). Hazard prediction activities for safety education. Doboku Gakkai Ronbunshuu F/JSCE Journal of Construction Engineering and Management, 66(1), 55-69. https://doi.org/10.2208/jscejf.66.55
Ishikawa, M., Hirao, T., & Maezawa, M. (2008). Study of patient safety education for undergraduates. Igaku Kyoiku / Medical Education (Japan), 39(2), 115-119. https://doi.org/10.11307/mededjapan1970.39.115
Ito, K., Taguchi, H., & Fujinami, K. (2014). Posing questions during experimental operations for safety training in university chemistry experiments. International Journal of Multimedia and Ubiquitous Engineering, 9(3), 51-62. http://dx.doi.org/10.14257/ijmue.2014.9.3.06
Japan Industrial Safety and Health Association. (2008). Sugu ni jissen shirīzu Anzen wo Sakidori Kiken Yochi [Practice series: Ahead of safety, risk prediction]. Tokyo, Japan: JISHA.
Japan Industrial Safety and Health Association. (n.d.). Iryō kango | kiken yobō kunren (KYT) muryō irasutoshīto-shū [Medical/Nursing | Risk prediction training (KYT) free illustration sheet collection]. Retrieved from https://www.aemk.or.jp/kyt/iryo/page/5
Ji, H. J. (2014). A study on safety culture construction for coal mine. Applied Mechanics and Materials, 644-650, 5949-5952. https://doi.org/10.4028/www.scientific.net/AMM.644-650.5949
Kadoyanagi, T. (2016). Shūdan sanka taiken-gata kōshū-yō kizai (dōga KYT)-tō no un’yō jōkyō ni tsuite (tokushū jukō-sha no tokusei ni ōjita kōtsū anzen kyōiku) (Operation of group training equipment [Video KYT]. [Traffic safety education according to the characteristics of the students]). Gekkan Kōtsū, 47(7), 44-55.
Kawano, R. (2002). Iryō risuku manējimento seminā tekisuto [Medical risk management seminar text]. Tokyo, Japan: Tepco Systems.
Kazaoka, T., & Otsuka, K. (2003). Study of nursing students’ recognition of the risks of medical treatment accidents: Using the scenario of role playing drug misadministrations. Journal of Japan Society of Nursing Research, 26(5), 133-143. https://doi.org/10.15065/jjsnr.20030912009
Lewin, K. (1936). Principles of topological psychology. New York, NY: McGraw-Hill. http://dx.doi.org/10.1037/10019-000
Lucian Leape Institute. (2010). Unmet needs: Teaching physicians to provide safe patient care. Boston, MA: National Patient Safety Foundation.
Mayer, D., Klamen, D. L., Gunderson, A., & Barach, P. (2009). Designing a patient safety undergraduate medical curriculum: The telluride interdisciplinary roundtable experience. Teaching and Learning in Medicine, 21(1), 52-58. https://doi.org/10.1080/10401330802574090
Mochizuki, R., & Komatsubara, A. (2016). Proposal of traffic KYT with using What-if analysis. The Human Factors in Japan, 20(2), 79-82.
https://doi.org/10.11443/jphf.20.2_79
Molloy, G. J., & O’Boyle, C. A. (2005). The SHEL model: A useful tool for analyzing and teaching the contribution of Human Factors to medical error. Academic Medicine, 80(2), 152-155.
Murata, A., Hayami, T., & Moriwaka, M. (2009). Visual information processing characteristics of drivers in prediction of dangerous situation-comparison among novice, expert and non-licensed person. In Proceedings: Fifth international workshop on computational intelligence & applications, 2009(1), 254-257. Hiroshima, Japan: IEEE SMC Hiroshima Chapter.
Nagamatsu, I., Miyazaki, I., & Harada, C. (2011). Kango kiso kyōiku ni okeru kiken yochi torēningu (KYT) wo toriireta iryō anzen kyōiku ni kansuru kōsatsu: Dōga jirei o mochiita puroguramu no kōka [A study on medical safety education incorporating risk prediction training (KYT) in nursing education: Effects of programs using movie]. Nihon kango gakkai ronbun-shū. Kango kyōiku, 42, 158-161. Retrieved from
https://iss.ndl.go.jp/books/R000000004-I023685394-00?ar=4e1f&locale=e
Nakajima, K. (2012). 4. Patient safety and quality improvement education for undergraduate medical students. Nihon Naika Gakkai Zasshi [Journal of the Japan Society of Internal Medicine], 101(12), 3477-3483. https://doi.org/10.2169/naika.101.3477
Noor, A. Y., Irniza, R., Emilia, Z. A., Anita, A. R., & Suriani, I. (2016). Kiken yochi training (KYT) in reducing accidents at workplaces: A systematic review. International Journal of Public Health and Clinical Sciences, 3(4), 123-132.
Poosanthanasarn, N., Sriboorapa, S, Fungladda, W., & Lohachit, C. (2005). Reduction of low back muscular discomfort through an applied ergonomics intervention program. The Southeast Asian Journal of Tropical Medicine and Public Health, 36(Suppl. 4), 262-270.
Reason, J. T. (1997). Managing the risks of organizational accidents. Aldershot, England: Ashgate Publishing Limited.
Stickdorn, M., & Schneider, J. (2012). This is service design thinking: Basics-tools-cases. Amsterdam, The Netherlands: BIS Publishers.
Takahashi, A., Mishina, M., Takagi, M., Shimazaki, K., Ishida, T., & Umezaki, S. (2017). Taburetto tanmatsu wo mochiita anzen kyōzai no kunren kōka to anzen kanri e no ōyō: Teisō jūtaku kenchiku genba wo taishō to shite [Effect of safety teaching materials using tablet and its application to safety management: For low-rise residential building]. Specific research reports of National Institute of Occupational Safety and Health, 47, 39-44.
Takahashi, R. (2010). Nontekunikkusukiru torēningu e no chosen [Challenge to non-technical skills training]. In K. Nakajima, & Y. Kodama (Eds.), Iryō anzen koto hajime [Beginning of medical safety] (pp. 36-51). Tokyo, Japan: Igaku Syoin.
Walton, M., Woodward, H., Van Staalduinen, S., Lemer, C., Greaves, F., Noble, D., … Barraclough, B. (2010). The WHO patient safety curriculum guide for medical schools. BMJ Quality & Safety, 19(6), 542-546. http://dx.doi.org/10.1136/qshc.2009.036970
Yoneda, T., Itami, K., Seki, K., Kawabata, A., Kubota, Y., Yasuhara, O., & Maesako, T. (2017). Changes in nursing students’ risk awareness and understanding of medical incidents after exposure to a simulated incident. Japan Journal of Educational Technology, 41(Suppl.), 17-20.
https://doi.org/10.15077/jjet.S41011
*Yoshitaka Maeda
Medical Simulation Center,
Jichi Medical University,
3311-1, Yakushiji,
Shimotsuke-shi, Tochigi, Japan
Tel: +81 285 58 7455
Email: y-maeda@jichi.ac.jp
Announcements
- Best Reviewer Awards 2025
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2025.
Refer here for the list of recipients. - Most Accessed Article 2025
The Most Accessed Article of 2025 goes to Analyses of self-care agency and mindset: A pilot study on Malaysian undergraduate medical students.
Congratulations, Dr Reshma Mohamed Ansari and co-authors! - Best Article Award 2025
The Best Article Award of 2025 goes to From disparity to inclusivity: Narrative review of strategies in medical education to bridge gender inequality.
Congratulations, Dr Han Ting Jillian Yeo and co-authors! - Best Reviewer Awards 2024
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2024.
Refer here for the list of recipients. - Most Accessed Article 2024
The Most Accessed Article of 2024 goes to Persons with Disabilities (PWD) as patient educators: Effects on medical student attitudes.
Congratulations, Dr Vivien Lee and co-authors! - Best Article Award 2024
The Best Article Award of 2024 goes to Achieving Competency for Year 1 Doctors in Singapore: Comparing Night Float or Traditional Call.
Congratulations, Dr Tan Mae Yue and co-authors! - Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors.









