Before we start to discuss the relationship between sarcopenia and obesity, we need to define the clinical diagnosis of obesity first. The body mass index (BMI) and waist circumference are commonly used for the diagnosis of obesity. BMI is calculated with the total body weight in kilogram divided by the height in meters squared. Yet, the classification of BMI score shall also take into account age, sex, and race as well, since those factors were known to influence adiposity. For simplicity, we will use the standard BMI defined by the Centers for Disease Control and Prevention in the USA for the following discussion. For the adults 20 years old and older, BMI ranges from 18.5-24.9 is considered as normal or healthy weight, and 25-29.9 is indicative as overweight. BMIs below 18.5 are underweight and above 30 are obese. Obesity could be further classified as:
- Degree 1: BMI of 30 to 34.9
- Degree 2: BMI of 35 to 39.9
- Degree 3: BMI greater than 40 (severe obesity)
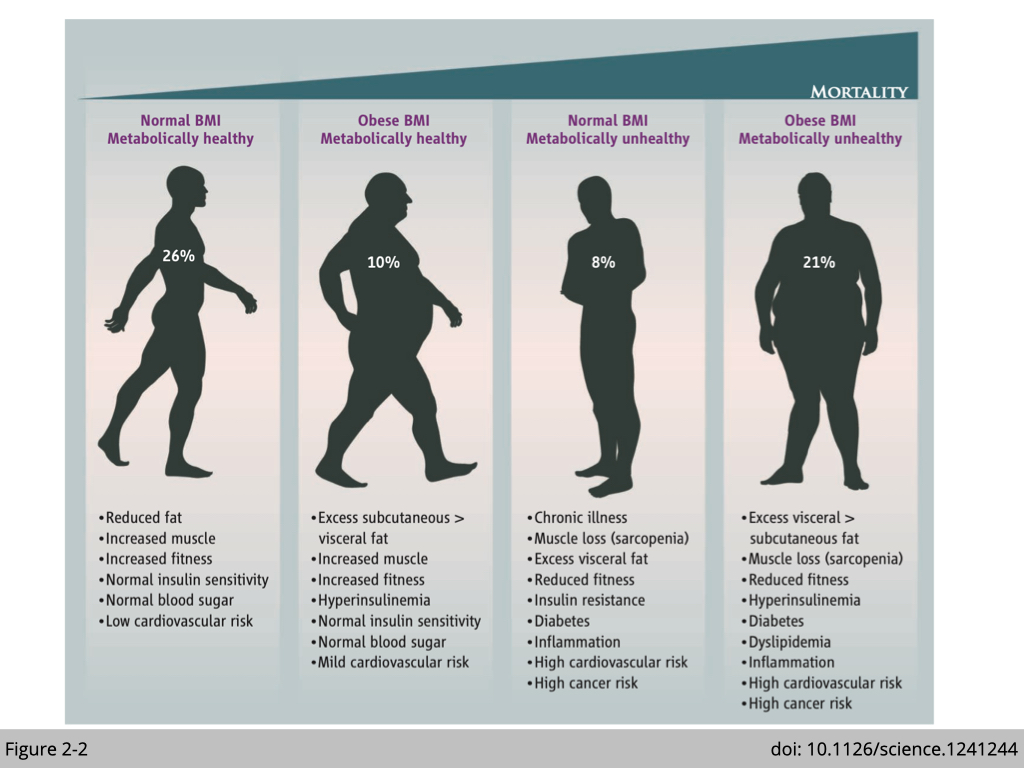
However, the “obesity-mortality paradox” has been observed in epidemiological studies on aging and general health. Studies on over a million people across different contents globally have reported a U-shape relationship between BMI and mortality. People with BMI greater than 40 or lower than 18.5 are both associated with increased mortality. Yet, people with degree one obesity have been shown to have advantages on survival from all-cause mortality, particularly the deaths from cardiovascular diseases, compared to people with normal BMI. It was estimated that about 10% of adult have obese BMI is metabolic healthy that they have normal glucose metabolism and increased muscle mass (Figure 2-2). In contrast, 8% of adults have normal BMI, but they are metabolic unhealthy with sarcopenia.
The advanced technology for body composition to distinguish lean mass and adiposity is especially required to clarify the relationship between body composition and mortality. We now know that BMI does not always reflect the adiposity and the quality (location) of adipose tissues in humans. For instance, gymnasts and weightlifters have higher BMI from the increased lean mass with relatively short statures. Moreover, visceral adiposity, not subcutaneous adiposity, has been reported to be involved in the development of metabolic and cardiovascular diseases. Visceral fat refers to the adipose tissues surrounding the organs, versus subcutaneous fat is located between the skin and the outer abdominal wall. An increase in pro-inflammatory cytokines secretion from visceral and intramuscular fat leads to systemic inflammation and insulin resistance in skeletal muscle, which we have named the condition "sarcopenic obesity." A study recruited 4,984 elderly (mean age was 71.1, 56.5% subjects are female, and the median follow-up was 102 months) to study the relationship of body composition between fat and appendicular lean mass by Dual-energy x-ray absorptiometry (doi: 10.1093/gerona/glx002.). They found that the prevalence of sarcopenic obesity was 12.6% in males and 33.5% in females. The prevalence of sarcopenic obesity increased with age in both sexes.
As obesity could directly cause sarcopenia, sarcopenia, which reduces whole-body energy utilization, could adversely lead to further obesity, creating a vicious cycle
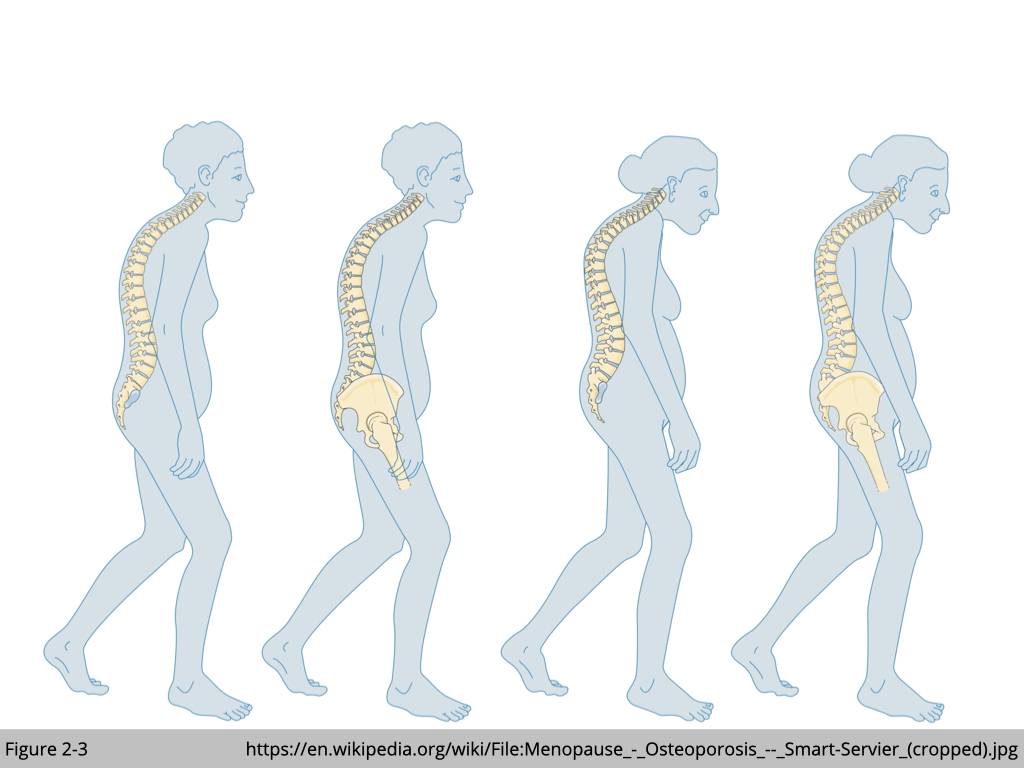
Osteoporosis is characterized by low bone mineral density and deteriorated microarchitecture of bone tissue, leading to increased susceptibility to fracture (Figure 2-3). The common way used to diagnose osteoporosis is dual energy x-ray absorptiometry (DEXA) in clinical practice. Back pain, loss of height, and a stooped posture are the typical symptoms of osteoporosis. Yet, similar to sarcopenia, there are no apparent symptoms of osteoporosis in the early stages of bone loss for people to be aware of the condition. Osteoporosis often coincides with sarcopenia in the elderly. It is, however, a challenge to dissect out a causal or associated relationship between osteoporosis and sarcopenia. Aging is the major risk factor for the development of osteoporosis and sarcopenia. There is a lifelong linear correlation between bone mineral content and lean body mass. People reach their peak bone and skeletal muscle mass in late adolescence and early adulthood. In the early 30s, gradual decreases in bone and lean muscle mass occur (~1% annually). By the age of 80, we lose about 30% of bone and skeletal muscle mass. Besides, fat infiltration and physical inactivity are other shared risk factors that worsen the conditions in osteoporosis and sarcopenia. Nonetheless, osteoporosis and sarcopenia are primary causes of immobility and frailty.
The mechanical coupling between bone and skeletal muscle was assumed the only interaction between them. Skeletal muscles attach to the bone via tendons and use bone as a lever for contraction, which thus generates force and causes movement in our body. The mechanical loading from muscle contraction strengthed the bone. For instance, a study examined the relationship of bone mineral density and muscle mass with different types of exercise training in young girls (7-9 year-olds; 14 gymnasts, 14 swimmers, and 17 controls). They found that even though gymnasts weigh less, they have greater bone mineral density per unit than swimmers and controls (doi: 10.1097/00005768-199610000-00006). On the other hand, it has been well-documented that paralysis exacerbates the development of osteoporosis. The mechanical loading on the bone does have a positive association with bone density.
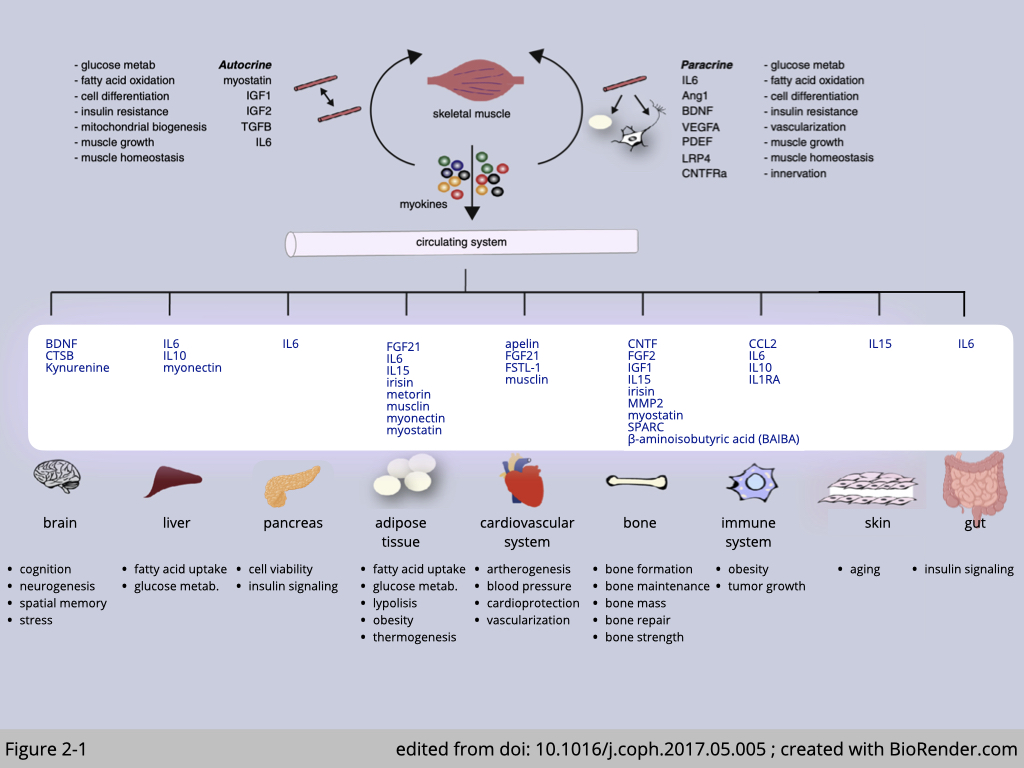
In addition to the physical interaction between bone and skeletal muscle, many studies suggest that they could also communicate chemically and metabolically (Figure 2-1). Recently, bone and skeletal muscle have been reclassified as secretory organs. High magnitude mechanical loading stimulates both bone and skeletal muscle secreting the positive factors for the other’s growth and functions. For example, β-aminoisobutyric acid (BAIBA) is secreted from skeletal muscle after exercise and has been shown to prevent bone loss from immobilization in mice (doi: 10.1016/j.celrep.2018.01.041). The positive association with BAIBA and hip bone mineral density have also been observed in human (doi: 10.1038/s42003-020-0766-y). Osteocalcin, which is exclusively expressed in the bone, has been shown to promote glucose uptake and utilization in skeletal muscle during exercise (doi: 10.1016/j.cmet.2016.05.004).
Decoding the communication between bone and skeletal muscle could provide the new therapies to treat these two highly related aging-associated diseases: osteoporosis and sarcopenia at one go.
More reading about Diagnosis and Management of Osteoporosis: https://www.aafp.org/afp/2015/0815/p261.html