- Home
- Ethical and Legal Challenges in Surgical Innovation: Frameworks for Responsible Practice
Venue: Level 1, Saffron Room, Shaw Foundation Alumni House, 11 Kent Ridge Drive, Singapore, 119244 (Map)
Date: Friday 15 November 2024
Time: 9.00am to 12.00pm
Programme
|
9:00am – 9:10am |
Introduction |
|
9:10am – 10:00am |
Talk by Professor Richard Huxtable Title: Conceptualising, evaluating, and regulating surgical innovation |
|
10:00– 10: 20 |
Break |
|
10:20 – 11:10 |
Talk by Dr Naomi Holbeach Title: Confidence-based Surgical Innovation: A framework for responsible surgical innovation |
|
11:10 -12:00 |
Panel Discussion |
Workshop Synopsis
Surgical innovation promises significant advancements in patient care but also introduces complex ethical and legal challenges. This workshop brings together experts in bioethics, law, and medicine to explore these challenges and provide frameworks for responsible innovation.
The workshop will delve into the ethical dilemmas and patient safety considerations of introducing new surgical techniques. Participants will gain insights into ensuring informed consent, the importance of professional consensus, and balancing the ethical duty to innovate with legal obligations. By examining case studies and expert frameworks, attendees will be equipped with the knowledge and tools needed to navigate the ethical and legal landscapes of surgical innovation, ensuring both patient safety and the advancement of medical practices.
Our Speakers

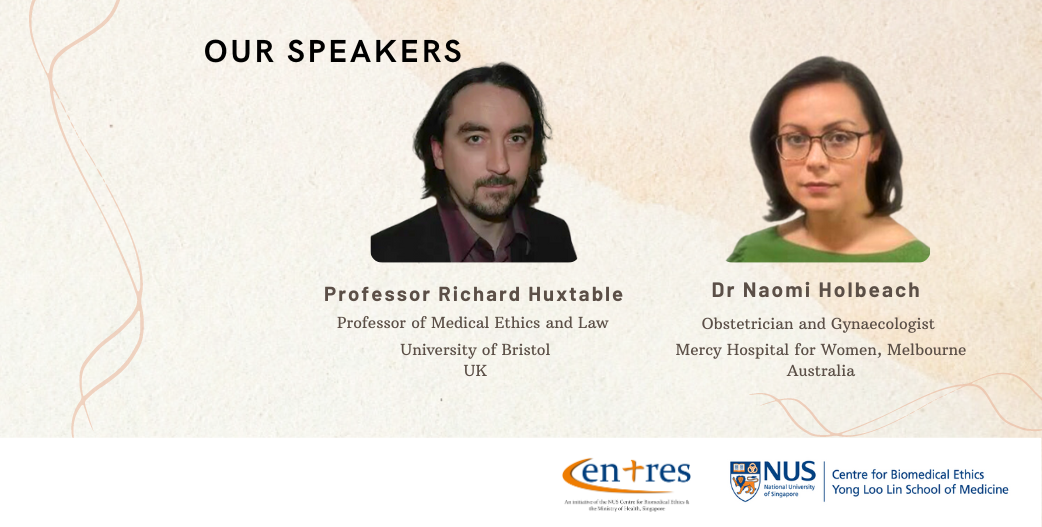
Professor Richard Huxtable
University of Bristol
Biography
Professor Richard Huxtable is the Professor of Medical Ethics and Law in University of Bristol. His research primarily concerns legal and ethical issues in end-of-life decision-making, surgery and paediatrics. He is the author of Law, Ethics and Compromise at the Limits of Life: To Treat or Not to Treat? (Routledge-Cavendish, 2012), Euthanasia, Ethics and the Law: From Conflict to Compromise (Routledge-Cavendish, 2007) and (with Dickenson & Parker) The Cambridge Medical Ethics Workbook (CUP, 2nd edn, 2010), plus numerous articles and chapters. His research has been funded by organisations including the Wellcome Trust and the European Commission and he has given invited presentations at the Royal Society of Medicine and the Royal College of Surgeons, as well as conferences worldwide.
Abstract
In promising to offer new – and presumably improved – ways of benefitting patients, surgical innovation appears to merit support and encouragement. Complications and controversies worldwide nevertheless reveal that the promise can transform into peril, with patients reportedly coming to harm from innovations involving (for example) vaginal mesh and trachea transplants. Surgical innovation, then, evidently needs careful evaluation and oversight. There are, however, at least three obstacles in the path of assessment and, ultimately, safe regulation. First, neither “surgical innovation” nor, indeed, “surgery” itself are easy to define. Even if we assume the phenomena can be satisfactorily defined, then, second, it is unclear which ethical governance or authorisation paradigm best suits surgical innovation: for example, should such innovation fall within the purview of a Research Ethics Committee (or IRB), a Clinical Ethics Committee, or some other mechanism? Finally, and perhaps most surprisingly, the very basis on which surgery can be lawfully performed continues to prove elusive. Drawing on work undertaken with colleagues at Bristol’s NIHR Biomedical Research Centre, this presentation will explore the concepts and challenges, making reference to the position in England and Wales, but with anticipated relevance beyond that jurisdiction

Dr Naomi Holbeach
Mercy Hospital for Women in Melbourne, Australia
Biography
Dr Naomi Holbeach is an Obstetrician and Gynaecologist from the Mercy Hospital for Women in Melbourne, Australia. She holds dual qualifications in law and medicine and has recently completed a PhD in bioethics on surgeons’ legal and ethical obligation about surgical innovation. Naomi is also the Academic Coordinator for Learning and Teaching and a senior lecturer in the Department of Obstetrics, Gynaecology and Newborn Health at the University of Melbourne. In this role she teaches medical students medicine, law and ethics.
Abstract
Confidence-Based Surgical Innovation is a framework that promotes responsible surgical innovation by combining evidence-based medicine and philosophical reasoning to provide surgeons with a step-by-step guide to thinking clearly about innovation that aligns with their legal and professional obligations. Using this framework addresses the problems faced by surgical innovation related to surgeons’ obligations and clinical decision-making behaviours that I identify from Australian examples.
Surgical innovation is an essential part of surgical practice, but it is inherently risky. Despite a long history of innovation in surgery and many extraordinary advances in patient care, patients can be harmed by surgical innovation. While it is appropriate to approach innovative surgery with caution in the interests of patient safety, this must be balanced with active promotion of responsible innovation.
Having analysed the legal and professional obligations of surgeons in Australia, I find that existing obligations do not support surgical innovation. Surgeons have legal and professional obligations with respect to their care of patients. These obligations apply to all care provided to patients, whether the care is innovative or not and require surgeons to have a rational basis for the treatment they offer. Usually, the rational basis for treatment arises from clinical evidence and peer professional support. However, clinical evidence and peer support may be limited or lacking for surgical innovation, and in such circumstances is not clear how to proceed so that obligations are met. This culminates in general uncertainty around surgeons’ obligations, which leads to two problems for surgical innovation – first, that much-needed surgical innovation is at risk of not happening when it should, and, second, that when it is undertaken it is not reliably undertaken responsibly.
To address this, I propose a framework to provide surgeons with a clear, stepwise approach to good reasoning about surgical innovation that meets their obligations and promotes responsible implementation of innovation. This framework combines well-established evidence-based medicine principles with philosophical reasoning. The framework, which I have called Confidence-Based Surgical Innovation, provides a structured approach to therapeutic reasoning that has to date been missing. I argue that by using philosophical reasoning alongside evidence-based medicine, we can formalise and defend conclusions about safety and efficacy of surgical innovation. Ultimately resulting in responsible innovation being offered to patients and implemented in ways that more autonomy-enhancing and more defensible in legal and disciplinary proceedings.
CME / CPE Points
CME (non-core) points for doctors, CPE points for nurses and pharmacists are being applied and subjected to approval.