Turning threats into opportunities—Transforming pharmacy education for modern pharmacy practice
Submitted: 16 July 2020
Accepted: 4 November 2020
Published online: 13 July, TAPS 2021, 6(3), 118-120
https://doi.org/10.29060/TAPS.2021-6-3/CS2392
Wai Keung Chui, Han Kiat Ho, Li Lin Christina Chai & Paul J. Gallagher
Department of Pharmacy, Faculty of Science, National University of Singapore, Singapore
I. THE CHANGING LANDSCAPE IN PHARMACY PRACTICE
Pharmacy practice in Singapore is rapidly evolving with the advent of technological innovations and changes in patient demographics. For instance, the dispensing process in hospitals have been automated; telepharmacy has made access to pharmaceutical services more convenient in the community; an aging population has brought along complex co-morbidities, chronic diseases, polypharmacy and community-based pharmaceutical care services that will require clinical interventions by pharmacists. These examples have raised the question of the “relevance of pharmacists” in the evolving health system. To stay relevant, pharmacists must move from the traditional medication supply (product focus) role to curating the optimal use of medicines by patients (patient focus) in a technology and informatics driven health system. This paradigm shift can only be enabled if the education of pharmacists is suitably re-constructed with outcomes that will future-roof their capabilities in the new healthcare ecosystem. This prompted the Department of Pharmacy at the National University of Singapore (NUS) to make a commitment to review its present programme thereby turning the threats into opportunities for its future pharmacy graduates. This case study reports the approach taken by the Department to re-engineer its curriculum for modern pharmacy practice in the twenty-first century.
II. NEEDS ANALYSIS AND RECOMMENDATIONS
In late 2018, a needs analysis was conducted by the Department to inform the design strategies. This was done through structured interviews by informed consent of key opinion leaders, and focused group discussions with alumni and students. The data collected were coded and analysed thematically. Some main themes about the graduates that came through were the weakness in applying their knowledge, their lack of an understanding of the health system and their reluctance to take leadership role. Feedback on the present curriculum included a lack of connectivity between modules that were taught in silos and the structured experiential learning was scheduled too late in the curriculum. It was recommended that a competency-based and integrated curriculum (Husband et al., 2014; Pearson & Hubball, 2012) would help students achieve the necessary competence as a health professional and apply the multidisciplinary knowledge holistically to problem solve. An introduction of systems thinking, and a longitudinal experiential learning programme across the four years will help students understand their future work environment better.
III. PROGRAMME DESIGN
Based on these recommendations, the department had to deconstruct and re-organise the current traditional teaching approach where basic sciences are taught in separate modules in years 1 to 2 while topics in pharmacy practice and therapeutics are introduced from years 3 to 4; with work-place learning happening only after year three. A Curriculum Design Group (CDG) was established to dissect and develop the curriculum. The CDG adapted the key competencies listed in the Association of Faculties of Pharmacy in Canada Educational Outcomes for First Professional Degree Programs in Pharmacy (Association of Faculties of Pharmacy of Canada, 2017) as the basis for the competency-based curriculum. The students will learn to approach pharmacy practice by skilfully integrating sub-competencies of communicator, collaborator, leader-manager, scholar-innovator, health advocate and professional roles into an overarching care provider role. The scholar role is expanded to scholar-innovator role as innovation aligns well with the core value of NUS and is also a critical attribute to safeguard against future disruptions. The key competencies under each role are carefully mapped onto the learning outcomes of themed modules. The themed modules (based on physiological systems) are designed using a theoretical framework of integrating basic, clinical and systems sciences (Gonzalo et al., 2017) (Figure 1). To help students make sense of what they learn, experiential learning is incorporated longitudinally across the four years so that students can apply their theoretical studies at the workplace when they go on clinical placements (Figure 1). This 3-pillar educational framework has been successfully applied in medical education in the US to develop medical competencies and systems thinking among the physicians (Gonzalo et al., 2017); the CDG believed that the same framework would work for pharmacists in Singapore.
Pharmacy graduates must be prepared for a health system that is driven by informatics and technology. Joseph Aoun in his book “Robot-Proof: Higher Education in the Age of Artificial Intelligence” (Aoun, 2017) recommended undergraduate students to acquire technical, data and human literacies, which he collectively refers to as the “humanics”, for them to stay ahead of the technological revolution. Therefore, subjects such as medical sociology, computational thinking, health informatics are included to cultivate the humanics in the pharmacy students. It is envisaged that this approach can better prepare the graduates to work with patients, co-workers, data and technologies in providing quality care. Furthermore, instilling characteristics of a transformational leader and familiarising students to implementation science will take a step closer to grooming the student pharmacists into future leaders.
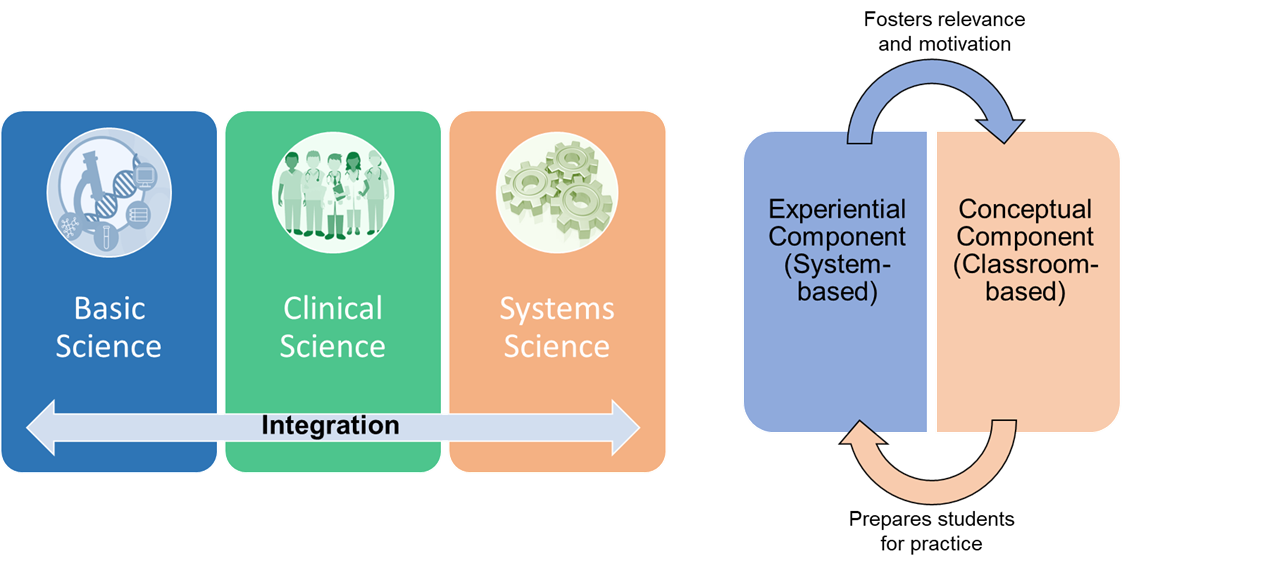
Figure 1: The theoretical framework of curricular integration. Adapted from Gonzalo et al. (2017) and Pearson and Hubball (2012).
In the new programme, students are made accountable of their own learning through pre-class preparations and interactive team-based learning (TBL) in the classroom. TBL sessions are facilitated by a scientist and a clinician who help students to use integrative thinking to solve the cases. In the laboratory, students will also work in teams to gather scientific data for inquiry-based learning. The impact of the new educational approach will be evaluated against all the four levels of the new world Kirkpatrick Model to determine the effectiveness of the curriculum.
IV. TRANSFORMING PHARMACY EDUCATION IN RESPONSE TO THREATS
The fourth industrial revolution has indeed caused disruptions to pharmacy practice. Pharmacists will have to step forward and be leaders of change when it comes to any matter related to medicines, be it optimising drug use, identifying drug-related problems or recommending cost-effective therapy. Therefore, it is the mission of NUS Department of Pharmacy to respond to the threats by transforming its professional pharmacy programme to one that can future proof its graduates who will be ready to seize new opportunities in a dynamic health system.
Notes on Contributors
Professor Christina Chai is the Head of the Pharmacy Department at NUS. She initiated the EduRx project by calling for the need to redesign the professional pharmacy degree curriculum to better prepare the graduates for the evolving healthcare landscape in Singapore.
Associate Professor Ho Han Kiat, in the capacity of the Deputy Head (Education), supported the curriculum design group in ensuring that the new pharmacy curriculum is closely aligned to both the NUS educational philosophy and the educational outcomes for pharmacy graduates.
Professor Paul Gallagher and Associate Professor Chui Wai Keung are co-leaders of the EduRx project who under their co-leadership worked with the curriculum design group to develop the competency-based and integrative pharmacy programme.
Acknowledgements
The authors would like to acknowledge the contributions made by the curriculum design group that comprises the following members: Chng Hui Ting, Fan Wenjie, Han Zhe, Priscilla How, Law Hwa Lin, Eugene Lim Zi Jie, Anson Lim Zong Neng, Tan Bee Jen, Matthias Gerhard Wacker, and Yeo Shao Jie.
Funding
There is no research funding source for the programme review project.
Declaration of Interest
The authors declare no conflict of interest concerning any aspect of this case study.
References
Aoun, J. (2017). Robot-proof: Higher education in the age of artificial intelligence. The MIT Press.
Association of Faculties of Pharmacy of Canada. (2017). AFPC educational outcomes for first professional degree programs in pharmacy in Canada 2017. https://afpc.info/system/files/public/AFPC-Educational%20Outcomes%202017_final%20Jun2017.pdf
Gonzalo, J. D., Haidet, P., Papp, K. K., Wolpaw, D. R., Moser, E., Wittenstein, R., & Wolpaw, T. (2017). Educating for the 21st-century healthcare system: An interdependent framework of basic, clinical and systems sciences. Academic Medicine, 92 (1), 35-39. https://doi.org/10.1097/ACM.0000000000000951
Husband, A. K., Todd, A., & Fulton, J. (2014). Integrating science and practice in pharmacy curricula. American Journal of Pharmaceutical Education, 78 (3), 63. https://doi.org/10.5688/ajpe78363
Pearson, M. L., & Hubball, H. T. (2012). Curricular Integration in Pharmacy Education. American Journal of Pharmaceutical Education, 76 (10), 204. https://doi.org/10.5688/ajpe7610204
*Wai Keung Chui
Department of Pharmacy,
Faculty of Science,
Block S4A, 18 Science Drive 4,
Singapore 117543.
Tel: +65 6516 2933
Email: phacwk@nus.edu.sg
Announcements
- Best Reviewer Awards 2024
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2024.
Refer here for the list of recipients. - Most Accessed Article 2024
The Most Accessed Article of 2024 goes to Persons with Disabilities (PWD) as patient educators: Effects on medical student attitudes.
Congratulations, Dr Vivien Lee and co-authors! - Best Article Award 2024
The Best Article Award of 2024 goes to Achieving Competency for Year 1 Doctors in Singapore: Comparing Night Float or Traditional Call.
Congratulations, Dr Tan Mae Yue and co-authors! - Fourth Thematic Issue: Call for Submissions
The Asia Pacific Scholar is now calling for submissions for its Fourth Thematic Publication on “Developing a Holistic Healthcare Practitioner for a Sustainable Future”!
The Guest Editors for this Thematic Issue are A/Prof Marcus Henning and Adj A/Prof Mabel Yap. For more information on paper submissions, check out here! - Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Volume 9 Number 1 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors. - Volume 8 Number 3 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2021
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2021.
Refer here for the list of recipients. - Most Accessed Article 2021
The Most Accessed Article of 2021 goes to Professional identity formation-oriented mentoring technique as a method to improve self-regulated learning: A mixed-method study.
Congratulations, Assoc/Prof Matsuyama and co-authors. - Best Reviewer Awards 2020
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2020.
Refer here for the list of recipients. - Most Accessed Article 2020
The Most Accessed Article of 2020 goes to Inter-related issues that impact motivation in biomedical sciences graduate education. Congratulations, Dr Chen Zhi Xiong and co-authors.









