General dental practitioners’ perceptions on Team-based learning pedagogy for continuing dental education
Submitted: 14 April 2021
Accepted: 24 June 2021
Published online: 4 January, TAPS 2022, 7(1), 98-101
https://doi.org/10.29060/TAPS.2022-7-1/SC2517
Lean Heong Foo & Marianne Meng Ann Ong
Department of Restorative Dentistry, National Dental Centre Singapore, Singapore
Abstract
Introduction: Team-based learning (TBL) pedagogy is a structured, flipped classroom approach to promote active learning. In April 2019, we designed a TBL workshop to introduce the New Classification of Periodontal Diseases 2017 to a group of general dental practitioners (GDPs). We aimed to investigate GDPs feedback on learning this new classification using TBL pedagogy.
Methods: Two articles related to the 2017 classification were sent to 22 GDPs 2 weeks prior to a 3-hour workshop. During the face-to-face session, they were randomly assigned to five groups. They participated in individual and group readiness assurance tests. Subsequently, the GDPs had inter- and intragroup facilitated discussions on three simulated clinical cases. They then provided feedback using a pen-to-paper survey. Based on a 5-point Likert scale (1-strongly disagree to 5-strongly agree), they indicated their level of agreement on items related to the workshop and their learning experience.
Results: Majority (94.7%, 18 out of 19 GDPs) agreed the session improved their understanding of the new classification and they preferred this TBL pedagogy compared to a conventional lecture. All learners agreed they can apply the knowledge to their work and there was a high degree of participation and involvement during the session. They found the group discussion and the simulated clinical cases useful.
Conclusion: A TBL workshop is suitable for clinical teaching of the New Classification of Periodontal Diseases 2017 for GDPs. Its structure promotes interaction among learners with the opportunity to provide feedback and reflection during the group discussions. This model might be a good pedagogy for continuing dental education.
Keywords: Team-based Learning, General Dental Practitioners, New Classification of Periodontal Diseases
I. INTRODUCTION
Team-based learning (TBL) is a flipped classroom, structured learning pedagogy that was introduced by Larry Michaelsen and has gained popularity among healthcare educators recently. TBL is learner-centric and dialectic based, and practices logical discussion used for determining the truth of a theory or opinion (Michaelsen et al., 2008). It provides the opportunity for peer-teaching by group members and can assist weaker students in understanding course materials.
Several dental educators have utilised TBL in undergraduate dentistry programmes and observed higher engagement among learners, less student contact time and faculty time, and higher course grades (Haj-Ali & Al Quran, 2013). General dental practitioners (GDPs), unlike undergraduate dental students, juggle between busy dental practice and family life. Hence, GDPs might seek active learning with direct knowledge application to manage their continuing dental education needs efficiently. The World Workshop of Periodontology recently revamped the diagnosis of periodontal diseases and proposed a new classification of staging (Stage I-IV; based on severity of disease) and grading (Grade A-C; based on disease progression) for periodontitis (Tonetti et al., 2018). We aimed to investigate GDP feedback on learning this new classification using TBL pedagogy.
II. METHODS
This is a descriptive study on GDPs’ feedback on learning the New Classification of Periodontal Diseases 2017 using a TBL approach. 22 GDPs attended the TBL workshop in April 2019.
Two articles related to the new classification were sent to the GDPs 2 weeks prior to the 3-hour workshop. Five multiple-choice questions were crafted from the two articles (Individual Readiness Assurance Test, IRAT) to assess learners’ basic understanding of the new classification. Learners were divided into five groups to discuss IRAT and provide answers using the immediate feedback assessment technique card (Group Readiness Assurance Test, GRAT). Faculty then highlighted key elements of the new classification. Three clinical periodontal cases crafted based on the 4S framework principles i.e. same problem, significant problem, specific choice, and simultaneous reporting, were used in the application process (Michaelsen et al., 2008). The key question was to diagnose the periodontal condition based on the staging and grading criteria. Lastly, learners provided implied consent by answering an anonymous pen-to-paper survey voluntarily. They answered based on their level of agreement on a 5-point Likert scale (5 indicating strongly agree, 1 indicating strongly disagree). The survey comprising 13 education-related statements: two statements related to programme content, two to presentation, six to learning experience, and three about the workshop. Three qualitative questions in the survey were: “What do you like most about the workshop?”, “What aspects of the session could be improved?” and “Other comments and feedback”.
III. RESULTS
Nineteen out of the 22 GDPs who attended the TBL workshop responded to the survey (response rate 86.4%). Results are summarised in Figure 1. We conducted a reliability analysis on the perceived task values scale comprising two subscales (learning experience and workshop) with at least three items.
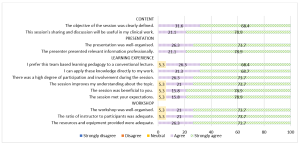
Figure 1. Learners’ feedback about the workshop
A. Content (Two items)
During the workshop, we highlighted the staging and grading criteria for the new classification. Learners provided a mean score of 4.74 (standard deviation, SD, 0.446; median 5) in two statements related to content. In general, 68.4% of them strongly agreed and 31.6% agreed the objective of the workshop was clearly defined. There were 78.9% and 21.1% of learners who strongly agreed and agreed respectively that the sharing and discussion during the workshop was useful to their clinical work.
B. Presentation (Two items)
Learners gave a mean score of 4.76 for presentation (SD 0.431; median 5). There were 73.7% learners who strongly agreed and 26.3% who agreed that the presentation was well-organised. In addition, 78.9% and 21.1% of the learners strongly agreed and agreed respectively that the presenter presented relevant information professionally.
C. Learning Experience (Six items)
Cronbach’s alpha for the learning experience subscale reached acceptable reliability at α = 0.81. The mean score for learning experience was 4.70 (SD 0.531; median 5). There were 68.4% learners who strongly agreed and 26.3% who agreed that they prefer TBL pedagogy to a conventional lecture. Also, 68.7% of the learners strongly agreed and 31.3% agreed they could apply the knowledge directly to their work. All learners agreed that there was a high degree of participation and involvement during the session. 18 learners (94.7%) agreed that the session met their expectations and improved their understanding about the topic.
D. Workshop (Three items)
The mean score for learners’ feedback on the workshop was 4.71 (SD 0.533; median 5). 18 learners (94.7%) agreed that the workshop was well organised with an adequate ratio of instructor to participants (2:22). There were 73.7% learners who strongly agreed and 26.3% who agreed that resources and equipment provided were adequate. Cronbach’s alpha for the workshop subscale reached acceptable reliability at α = 0.75.
E. Qualitative Feedback
The learners cited the following themes as their favourite component of the workshop: “group interaction and discussion” (4), “clinical case discussion” (3), “useful and relevant clinical cases” (1), “interesting readiness assurance test” (1), and “pre-reading material” (1). They also cited “active learning” (1), “correct wrong understanding” (1), “discussion improves my understanding” (1), and “great information and lecturer” (1) as positive learning experiences. Three different learners provided feedback of “best workshop ever attended”, “well done”, and “very good” respectively. One learner commented that the air-conditioning in the room was cold. One learner commented on small font size in dental charting and another learner suggested “less tests at the start”.
IV. DISCUSSION
The flipped classroom concept in TBL was suitable for GDPs to study the pre-reading articles at their own pace. The structured workshop enabled them to correct any misconception immediately and deepen their understanding about the new classification. This observation concurs with the finding that all GDPs agreed they could apply the knowledge to their work and preferred this pedagogy over a traditional lecture. This active learning process differs from a conventional didactic lecture, which is faculty-centric with less feedback and interaction. Hence, this pedagogy can be applied for some continuing dental education programmes by improving the delivery and application of new concepts. The 4S framework in the application cases are key elements to promote productive and logical discussion similar to a debate facilitated by faculty. The problem-solving aspect of TBL, along with the scaffolding and guidance by faculty, can enhance the metacognition process among learners (Hrynchak & Batty, 2012). Almost all learners agreed there was an adequate ratio of faculty to participants, emphasising the benefit of using TBL workshops to teach a large group of learners with less faculty. However, faculty needs to work more in planning and preparing the teaching materials, executing, and facilitating the session following the TBL structure and process. In addition, hurdles in conducting TBL include acceptance from faculty and learners, difficulty in supervising a large group, the customisation of the course content, and adequate training and expertise to conduct TBL effectively.
The learners also cited “group interaction and discussion” as their favourite component of the workshop. The learning theory underpinning TBL is the constructivist learning theory where the faculty exposes knowledge inconsistency during group discussion, subsequently allowing a new mental framework to be built upon the new understanding (Hrynchak & Batty, 2012). TBL is useful in healthcare education since it can promote good critical thinking and teamwork. In addition, the intra- and intergroup formal discussion provides the opportunity to reflect, give feedback, and enable peer-teaching. Self-reflection enables learners to make a judgement when modifying their existing knowledge. Peer-to-peer teaching in TBL enhances learning and aids weaker learners to understand the course material (Park et al., 2014).
Some limitations of our study were that the sample size was small, reporting participants’ self-perception on how they felt after attending the workshop and the lack of longitudinal follow-up on retention of knowledge. In addition, we did not have a separate didactic lecture on the new classification as a control group to truly compare the two different modes of teaching. Future recommendation includes having two groups of GDPs to collate their perceptions as well as include a pre and post assessment to investigate the difference in improvement and in knowledge retention comparing TBL workshop and traditional didactic lecture, and include peer evaluation in TBL to increase accountability among learners. Besides, ethnographic research method can be explored to provide insight to researchers to understand the essence of how dental professionals learn during TBL. It would be meaningful to follow up this group of GDPs to assess the accuracy of their periodontal diagnoses based on the new classification to investigate the effectiveness of the TBL workshop. Of note, TBL workshops can be adapted into an online format; this is particularly useful during the current COVID-19 pandemic to engage learners and promote active learning in an online setting.
V. CONCLUSION
In conclusion, TBL pedagogy may be another mode of teaching for GDPs in continuing dental education where participants are actively engaged, and direct application of knowledge gained can be made. During this pandemic, where face-to-face sessions are minimised, educators can consider adopting TBL pedagogy on an online platform to improve learning experience and engagement of their learners.
Notes on Contributors
Dr Lean Heong Foo is a Consultant Periodontist in Department of Restorative Dentistry and Head to the Dental Surgery Assistant Certification Programme in National Dental Centre Singapore. FLH reviewed the literature, contributed to study conception, data acquisition, data analysis, drafted and critically revised the manuscript.
Dr Marianne M. A. Ong is a Senior Consultant Periodontist & Director of Education in National Dental Centre Singapore. MO contributed to study conception, data acquisition and critically revised the manuscript. All authors gave their final approval and agreed to be accountable for all aspects of the work.
Ethical Approval
This study was exempted from formal Centralised Institutional Review Broad review by SingHealth Institutional Review Board (CIRB Ref: 2021/2133).
Data Availability
Data is deposited at Figshare. https://doi.org/10.6084/m9.figshare.14411858
Acknowledgement
The authors would like to thank Ms Safiyya Mohamed Ali for providing editorial support.
Funding
There was no funding involved in the preparation of the manuscript.
Declaration of Interest
The authors declare no conflict of interest.
References
Haj-Ali, R., & Al Quran, F. (2013). Team-based learning in a preclinical removable denture prosthesis module in a United Arab Emirates dental school. Journal of Dental Education, 77(3), 351–357.
Hrynchak, P., & Batty, H. (2012). The educational theory basis of team-based learning. Medical Teacher, 34(10), 796–801.https://doi.org/10.3109/0142159X.2012.687120
Michaelsen, L. K., Parmelee, D. X., McMahon, K. K., & Levine, R. E. (2008). Team-based learning for health professions education: A guide to using small groups to improving learning. Stylus.
Park, S. E., Kim, J., & Anderson, N. K. (2014). Evaluating a team-based learning method for detecting dental caries in dental students. Journal of Curriculum and Teaching, 3(2), 100-105. https://doi.org/10.5430/jct.v3n2p100
Tonetti, M. S., Greenwell, H., & Kornman, K. S. (2018). Staging and grading of periodontitis: Framework and proposal of a new classification and case definition. Journal of Periodontology, 89(Suppl 1), S159–S172. https://doi.org/10.1002/JPER.18-0006
*Foo Lean Heong
National Dental Centre Singapore,
5, Second Hospital Avenue,
168938 Singapore
Email: foo.lean.heong@singhealth.com
Submitted: 29 March 2021
Accepted: 28 September 2021
Published online: 4 January, TAPS 2022, 7(1), 102-105
https://doi.org/10.29060/TAPS.2022-7-1/SC2508
Mairi Scott & Susie Schofield
Centre for Medical Education (CME), School of Medicine, University of Dundee, Scotland, United Kingdom
Abstract
Introduction: The switch to online off-campus teaching for universities worldwide due to COVID-19 will transform into more sustainable and predictable delivery models where virtual and local student contact will continue to be combined. Institutions must do more to replace the full student experience and benefits of learners and educators being together.
Methods: Our centre has been delivering distance blended and online learning for more than 40 years and has over 4000 alumni across five continents. Our students and alumni come from varied healthcare disciplines and are at different stages of their career as educators and practitioners. Whilst studying on the programme students work together flexibly in randomly arranged peer groups designed to allow the establishment of Communities of Practice (CoP) through the use of online Discussion Boards.
Results: We found Discussion Boards encouraged reflection on learning, sharing of ideas with peers and tutors, reduce anxiety, support progression, and enable benchmarking. This led to a highly effective student sense of belonging to each other, our educators, and the wider University, with many highlighting an excellent student experience and maintaining a thriving CoP within the alumni body.
Conclusion: Despite being based on one large postgraduate programme in medical education, our CoP approach is relevant to any undergraduate programme, particularly those that lead to professional qualification. With our mix of nationalities, we can ‘model the way’ for enabling strong CoP’s to share ideas about best practice with a strong student and alumni network which can be shared across the international healthcare community.
Keywords: Communities of Practice, Sense of Belonging, Student Experience
I. INTRODUCTION
The sudden switch to online, dual delivery and on-campus/off-campus teaching for Universities worldwide will not be reversed at the end of the current COVID-19 crisis but will transform into a more sustainable and predictable delivery model where virtual and local student contact will continue to be combined. The switch, known as Emergency Remote Teaching (ERT) (Hodges et al., 2020) achieved much in a short timeframe but institutions need to do more to truly replace the full student experience and benefits of learners and educators being together on-site. The need for this new approach is acute in professional-based courses such as medicine where students need to learn complex skills within the context of healthcare delivery. These skills are acquired through multiple interactions with clinical colleagues in the workplace which, although often brief, are focused in real-time.
Given that the learning environment is dependent on the institutional ‘personality, spirit, and culture’ (Holt & Roff, 2004, pp. 553), human interaction is necessary to create that culture. We must develop new approaches to delivering medical education by merging established educational technologies with virtual approaches to establish on-line interaction with peers and senior colleagues such as can be achieved in Communities of Practice (CoPs) (Lave & Wenger, 1991). CoPs are social structures where people can share ideas, stories, and experiences relevant to the community’s activities. They help participants make sense of new knowledge and enable novices to benefit from working with experts, thus reducing anxiety, supporting progression, and enabling benchmarking. These components lead to the creation of a rich environment for information-sharing which has become increasingly important within healthcare delivery organisations during the COVID-19 pandemic.
We have built on over 40 years’ experience of delivering distance, blended and online Masters-level accredited medical education learning across five continents to ‘model the way’ to providing a strong student experience for online learners. Our students and alumni come from various interdisciplinary healthcare disciplines, at different stages of their career as educators and practitioners.
II. METHODS
Several Discussion Boards (DBs), usually one per study week plus one for assignment questions are created in each 12-week Moodle-based module. Students are randomly assigned to groups to work together flexibly within these peer groups. Each discussion has a ‘prompt’ linked to that week’s work, designed to create CoPs and a highly effective student sense of belonging (SoB) to each other and programme educators. In the first module students are actively encouraged to participate, with emphasis being on the ‘safe space’ created that allows them to learn effectively from and with each other. DB comments are used as part of programme enhancement and quality assurance. Students give informed consent to their evaluation comments within DBs being extracted for overall programme review.
III. RESULTS
As students move from legitimate peripheral participant to experienced member, they often express increased confidence that their posts will allow them to share their view and help colleagues. The forum posts have been analysed as part of a much larger study; the following diagram (Figure 1) highlights some of the benefits.
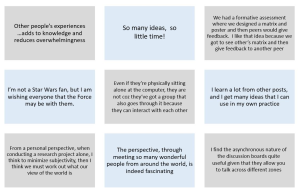
Figure 1. Sample of comments in DBs posts
Our experience over the last four years is that student levels of interaction increase the further into the programme they go, suggesting that they value and enjoy it. Overall, when asked specifically if that assumption is correct, feedback from students is exceptionally positive and they comment on their achievement of a SoB through engagement with the DBs. Many highlight the excellent student experience. Another indirect indication of success is that student module success rate averages 93% across the modules, which is high for an online learning programme.
The benefits of using DBs are threefold:
- They allow for reflection on learning in real-time due to regular module-specific weekly activities requiring students to reflect on that week’s educational materials and post their thoughts on the DBs.
- They allow sharing with peers and tutors, establishing CoPs: The DB posts create peer-to-peer dialogue, encouraging students to practise the language of the discipline in a safe, supported environment. Learning activities are based on the principle of linking previous experience with the interpretation of new knowledge, thus enabling an escalation of the complexity of questions to enhance deeper connection and dialogue. Although essentially (and importantly) it is the students as peers who are encouraged to respond to each other’s questions and comments, the tutors do monitor posts, providing input when necessary and desirable. In some modules, students are required to give peer feedback on draft assignments using a 1:4 ratio to encourage a range of views and expertise, increasing the depth and extent of their critical thinking and analysis. This also gives them practice in giving and receiving feedback, an essential skill for future medical educators.
- CoPs build trust in colleagues and a SoB within the learning environment, leading to an excellent learning experience. Students state that they value the tutor contribution as this increases the confidence they have in their own online comments, sometimes shifting the discussion to a more profitable area for new learning in a way that was not pre-planned or even at times expected.
IV. DISCUSSION
Our approach to the creation of CoPs is based on the principle that in order to establish student trust and a SoB DBs are an essential tool. Management research describes trust within organisations as being multifaceted, with the main components being capability, well-meaning intent, and integrity (Ridings et al., 2002). It is accepted that within our programmes both tutor and student capabilities have been established. Integrity is established by clearly explaining the expected mode of student behaviour at the outset and demonstrated as students work through the programme. Well-meaning intent is demonstrated by acts of positive reciprocation built up over time by asking students to give peer feedback frequently and around increasingly complex activities. Both integrity and well-meaning intent therefore need to have a continued focus during module design and delivery and throughout the assessment process.
Now that medical education has been forced to re-evaluate the place of online learning as a consequence of the COVID-19 crisis, it seems inevitable that many of the discovered benefits will lead to significant changes in the way we teach and learn. Davis (2018) explored a future medical school being one ‘without walls’ by which he meant that the artificial separation of the ‘classroom and the clinic’ would inevitably diminish as we embraced flipped classrooms and online collaborative learning.
If we adopt this approach for student learning it may also change the way we think about faculty development, as we could create extensive networks of faculty development special interest grouped CoPs beyond the ‘walls’ of our own schools. A recent study by Chan et al. (2018) in McMaster describes the creation of a Faculty Incubator – a virtual CoP which uses a longitudinal, asynchronous, online platform to deliver a one-year curriculum to support early-to mid-career educators from 30 different locations with their professional development. This widespread (geographically) collaborative approach was found to be well received, with lively interactions which broke down some of the boundaries that normally prevent early career academics from approaching unknown colleagues in different locations, colleagues they would normally never have met in person.
An additional challenge created by the COVID-19 pandemic was the necessity for healthcare professionals to make clinical decisions in an ‘evidence-poor’ disease by gathering emerging data (often by word-of-mouth) and treating patients without the certainty of a knowledge base built up over decades of robust randomised controlled trial (RCT) evidence. This is described by Rosenquist (2021, pp. 8) as a kind of “Bayesian fatigue”: a stress-induced dysphoria experienced when the corpus of knowledge that is the foundation of one’s work acquired over decades, becomes less important than information being gathered from disparate sources in real time.’ The ‘disparate sources’ referred to here are groups of widely dispersed practitioners (within current and new CoPs) who are sharing individual and collective rapid learning by experience that has become necessary when treating patients with COVID-19. These CoPs are based on the collective trust healthcare professionals express in valuing the views of colleagues struggling with similar challenges. This helps reduce that ‘Bayesian’ impact when it comes to making difficult clinical decisions in real time with limited evidence. However, trust within a CoP also comes from previous positive experience of being within other CoPs, and so it is important that we as medical educators enable our students to have experience of the value of sustainable CoPs in their own learning. Despite the limitations of the range of the study comments, we believe that given the extent of the sudden switch to ERT our findings of use of DBs to establish much appreciated CoPs justifies early dissemination through this short communication.
V. CONCLUSION
As medical educators we must have the skills necessary to establish strong and sustainable CoPs to educate current and future healthcare professionals in this effective way of learning from each other. This can be done as effectively with online learning as with on-campus interaction, allowing the possibility of the widespread creation of truly effective international CoPs sustainable for years to come.
Notes on Contributors
Professor Mairi Scott reviewed the literature, selected the data, wrote the manuscript, created the presentation and presented the materials virtually to the Conference. Dr Susie Schofield reviewed the literature, advised on the selection of the data and gave critical feedback on the manuscript. Both authors have read and approved the final manuscript.
Ethical Approval
Ethics approved was granted by School of Medicine & School of Life Sciences Research Ethics Committee, University of Dundee, Dundee, DD1 4HN on 03/05/19. Application Number: 19/41.
Data Availability
Ethical approval specified that raw data would not be made available for others out with the Centre ‘beyond the anonymised published or reported versions within the dissemination strategy’.
Acknowledgement
The authors would like to thank Dr Thillainathan Sathaananthan (PhD student) and Dr Linda Jones (PhD supervisor, Senior Lecturer) CME, University of Dundee, who produced some of the outcomes as part of research into student experiences with online learning and the use of Discussion Boards.
Funding
No grant or external funding was received for this work.
Declaration of Interest
Both authors have no conflict of interest to declare.
References
Chan, T. M., Gottlieb, M., Sherbino, J., Cooney, R., Boysen-Osborn, M., Swaminathan, A., Ankel, F., & Yarris, L. M. (2018). The ALiEM faculty incubator: A novel online approach to faculty development in education scholarship. Academic Medicine, 93(10), 1497–1502. https://doi.org/10.1097/ACM.0000000000002309
Davis, D. (2018). The medical school without walls: Reflections on the future of medical education. Medical Teacher, 40(10), 1004–1009. https://doi.org/10.1080/0142159X.2018.1507263
Hodges, C., Moore, S., Lockee, B., Trust, T., & Bond, A. (2020). The difference between emergency remote teaching and online learning. EDUCAUSE Review. https://er.educause.edu/%20articles/2020/3/the-difference-between-emergency-remote-teaching-and-online-learning
Holt, M. C., & Roff, S. (2004). Development and validation of the Anaesthetic Theatre Educational Environment Measure (ATEEM). Medical Teacher, 26(6), 553-558. https://doi.org/10.1080/01421590410001711599
Lave, J., & Wenger, E. (1991). Situated learning: Legitimate peripheral participation. Cambridge University Press.
Ridings, C. M., Gefen, D., & Arinze, B. (2002). Some antecedents and effects of trust in virtual communities: The Journal of Strategic Information Systems, 11(3-4), 271–295. https://doi.org/10.1016/S0963-8687(02)00021-5
Rosenquist, J. N. (2021). The stress of Bayesian medicine—Uncomfortable uncertainty in the face of COVID-19. New England Journal of Medicine, 384(1), 7-9. https://doi.org/10.1056/NEJMp2018857
*Mairi Scott
Centre for Medical Education,
University of Dundee
Email: m.z.scott@dundee.ac.uk
Submitted: 15 January 2021
Accepted: 12 April 2021
Published online: 5 October, TAPS 2021, 6(4), 142-145
https://doi.org/10.29060/TAPS.2021-6-4/SC2489
Anne Thushara Matthias1, Gam Aacharige Navoda Dharani1, Gayasha Kavindi Somathilake2 & Saman B Gunatilake1
1Faculty of Medical Sciences, University of Sri Jayewardenepura, Gangodawila, Sri Lanka; 2 National Centre for Primary Care and Allergy Research, University of Sri Jayewardenepura, Sri Lanka
Abstract
Introduction: Multiple factors influence doctor-patient communication. A good consultation starts with an introduction of him or herself by the doctor to the patient. The next step is to address patients in a manner they prefer. There is a paucity of data about how best to address patients in an Asian country. This study investigates how patients prefer to be addressed by doctors.
Methods: This is a cross-sectional study conducted from July 1st to August 31st, 2020 at a single Centre: Colombo South Teaching Hospital in Sri Lanka.
Results: Of 1200 patients, 63.25% reported that doctors never introduced themselves and 97.91% of patients reported, doctors never inquired how to address them. 49.9% preferred to be addressed informally (as mother, father, sister) than by the name (first name, last name, title). The older female patients, married patients, patients of lower education, and lower monthly income preferred to be addressed informally.
Conclusion: Most doctors did not introduce themselves to patients during medical consultations and did not inquire how patients wish to be addressed.
Keywords: Doctor-Patient Relationship, Medical Consultation, Professionalism, Introduction, Doctor’s Name Badge, South Asian, Sri Lanka
I. INTRODUCTION
Professionalism plays an important role in the practice of medicine. The Charter on Medical Professionalism has a set of 10 commitments. Commitment to professional responsibilities is one of them. It includes the way doctors dress and conduct themselves during a consultation (Blank et al., 2003). Abiding by these principles, doctors can improve their interaction with patients resulting in a better outcome (Gillen et al., 2018) A good introduction will facilitate a positive attitude from the patient towards the doctor. “#hellomynameis” campaign in the UK was initiated to create awareness about the importance of an introduction (Egener et al., 2017).
Professionalism is impacted by social, cultural, and economic factors. It is believed that the translation of professionalism concepts across the world should consider national cultural difference. Studies from western populations have shown that most patients prefer being addressed by their first name and for the doctor to be introduced by their full name and title (Egener et al., 2017). There is a paucity of data on how Asian patients wish to be addressed.
The Sri Lankan society is hierarchical based on age, caste, wealth, educational qualifications, and profession. Respect for doctors comes naturally in this system. Doctors are treated with great respect in rural communities. It is quite common to find doctors not introducing themselves to the patient and expecting them to know who you are. In Sri Lanka, doctors tend to address the patients mostly informally addressing the patient as a family member- ‘father, mother, uncle, sister, etc.’, in the local language assuming it would connect with the patient better. This study explores the way doctors address patients in an Asian cultural setting and the patient’s expectations.
II. METHODS
A cross-sectional study was conducted from 1st July to 31st August 2020 at the Colombo South Teaching Hospital. A total of 1200 patients were selected from the wards in a sequential, systematic manner with a skip interval of one. Informed verbal consent was obtained from the participants. The first part of the questionnaire contained demographics. Some questions asked the participants about how they wish to be addressed and how doctors addressed them and how they would like their doctor to introduce themselves. Informal methods of address were mother, father, sister, etc. Formal methods were the use of the first name, last name, or titles.
Statistical analysis including the statistical significance tests was performed using SPSS IBM SPSS Statistics Version 20 IBM Corp. (2017), IBM SPSS Statistics for Windows. Armonk, NY: IBM Corp. Pearson Chi-Square Association Test was used to identify the statistically significant associations between the categorical variables at a confidence level of 95%.
III. RESULTS
A. Demographics
(See Table 1)
Of the 1200 participants, 868 (72.33%) were female. Of the sample, 1022 (85.16%) were from urban areas.
|
Characteristics |
Number of participants (%) |
||||
|
Informal method
|
First name
|
Last name
|
No preference
|
||
|
Total |
|
599 |
427 |
77 |
79 |
|
Age |
Below 40 (< 40) (664) |
253 (38.10%) |
312 (46.99%) |
33 (4.97%) |
49 (7.38%) |
|
Above 40 (> = 40) (536) |
346 (64.55%) |
115 (21.46%) |
44 (8.21%) |
30 (5.60%) |
|
|
Education Level |
Post Graduate & Graduate (147) |
54 (36.73%) |
56 (38.1%) |
10 (6.8%) |
9 (6.12%) |
|
|
Grade 6-A/L (986) |
501 (50.81%) |
359 (36.41%) |
60 (6.09%) |
66 (6.69%) |
|
|
Grade 1-5 & Not educated (67) |
44 (65.67%) |
12 (17.91%) |
7 (10.44%) |
4 (5.97%) |
|
Income |
>100,000 (61) |
15 (24.6%) |
23 (37.7%) |
4 (6.56%) |
6 (9.84%) |
|
|
20,000-100,000 (982) |
490 (49.9%) |
357 (36.35%) |
66 (6.72%) |
64 (6.52%) |
|
|
<20000 (157) |
94 (59.87%) |
47 (29.93%) |
7 (4.45%) |
9 (0.75%) |
|
Occupation |
Skilled Occupations (581) |
251 (43.2%) |
230 (39.59%) |
40 (6.88%) |
84 (14.46%) |
|
|
Unskilled occupations (591) |
339 (57.36%) |
178 (30.11%) |
37 (6.26%) |
37 (6.36%) |
|
|
A/L & Uni students (28) |
9 (32.14%) |
19 (67.86%) |
– |
– |
Table 1. Difference between how patients wish to be addressed and vice versa
B. How Doctors Addressed Patients
Of the 1200 patients, 1175 (97.91%) reported that doctors never inquired how to address them at the beginning of the consultation (Matthias, 2021). A large proportion, 1124 (93.66%) reported that doctors have addressed them informally and 599 (49.9%) preferred being addressed informally, 427 (35.58%) preferred to be addressed by their first name, and 77 (6.41%) by their last name. Only 18, preferred to be addressed by their title (Dr/Rev).
More females preferred to be addressed informally when compared to the males (451/868 (51.96%) vs 148/332 (44.58%) (Pearson Chi-Square = 4.345, p = 0.037). Married patients preferred to be addressed informally when compared to the unmarried/divorced/separated (578/1089 (53.1%) vs 21/111 (18.9%), Pearson Chi-Square = 54.339, p < 0.001). The ethnicity of the patients and the area they are from (Urban/Rural) had no significant impact on how they desired to be addressed.
Over 65% of the patients (44/67) with a lower level of education preferred being addressed in an informal way whereas only 36.7% (54/147) of the graduates/post graduates preferred the informal way (Pearson Chi-Square = 23.264, p < 0.001). Monthly family income was a statistically significant variable and patients with a higher family income (Over LKR 100,000) preferred to be addressed more formally when compared to patients with an income below LKR 20,000 (40/61 = 65.57% Vs 54/157 = 34.39%, Pearson Chi-Square = 23.928, p < 0.001). The occupations of the patients are also a significant factor which affected their preference in the way being addressed with 57.4% of the patients with unskilled occupations (UN) and 43.2% of the ones with skilled occupations preferring the informal way (339/591 = 57.36% vs 251/581 = 43.20%, Pearson Chi-Square = 34.771, p < 0.001). Older patients (40 and above) preferred to be addressed informally when compared to others. (346/536 = 64.6% Vs 253/664 = 38.1%, p < 0.001).
Of 1059 patients, 495 (46.7%) preferred being addressed the informal way as they felt it made the doctor-patient relationship more personal and 627 (59.2%) patients felt the doctor treated them as their relative. Of the Doctors, 759 (63.25%) did not introduce themselves to the patients and 865 patients (72.08%) prefer doctors to wear a name badge. 718(59.8%) wanted doctors to introduce themselves with the title, doctor’s designation and specialty. 246(20.5%) wanted doctors to tell their title and first name. Only 4(0.3%) didn’t want doctors to introduce themselves.
IV. DISCUSSION
One important finding from our study was that doctors did not introduce themselves to patients. In most state sector hospitals in Sri Lanka, doctors do not wear a white coat or a name badge at present. A study done in the UK showed that 59.1% of patients and in our study 72% felt that doctors should wear name badges as a form of identification (Van Der Merwe et al., 2016). In our study, 98% of patients reported that doctors never inquired how to address them at the beginning of the consultation. To improve this aspect, these areas should be included in the objectives of the medical curriculum and continuous medical education programs of young doctors. The “Personal and professional development stream” which is taught in the medical faculty at Sri Jayewardenepura in Sri Lanka is an avenue that can be used for this purpose.
Social, cultural, ethnic, and other demographic factors can influence preferred modes of address. In our study, 50% prefer to be addressed in the informal way. There are several possible reasons for this. Sri Lankan people have long-standing cultural and religious beliefs. Sri Lankan traditions revolve around two dominant religions Buddhism & Hinduism. Filial piety, respect for one’s parents and elders, is a concept that is present in Asian countries. Addressing a person as a mother, father, son, etc. is considered as showing respect. The patients feel the doctors treat them as their own family or relative when they are addressed this way.
In studies done in most western countries, patients wish to be addressed by their first name. The higher the income and higher the education level of the patient, the lower is their preference for being addressed the informal way as they might perceive it as less professional. To solve the dilemma of whether to call the patient formally or informally and to make sure the patient is addressed according to their preference, the best approach would be to question the patient about their preferred name during their initial consultation and to record that in the patient’s records.
A. Strengths and Limitations
The large number of participants and recruiting from different wards; medical, surgical, paediatric, gynecology, and obstetrics to cover patients who were in the hospital for different illnesses are strengths. Not only did the study examine the patients’ preferred method of address, it examined the reasons behind the preference.
V. CONCLUSION
Our findings support a patient preference for informal greetings from their doctors in half the study population. It is not safe to assume that the patient can be addressed anyway the doctor deems right and it is good practice to ask patients how they prefer to be called at the beginning of the consultation. Doctors should introduce themselves clearly to patients and the current rates of introduction are inadequate. Majority of the patients prefer doctors to wear a name badge. In order to address patients in a culturally appropriate and patient preferred method it is always useful to ask the patient how they wish to be addressed.
Notes on Contributors
Anne Thushara Matthias was involved in conceptualisation, Methodology, Validation, Writing – Review & Editing, Supervision, Gam Aacharige Navoda Dharani was involved in investigation and data Curation, Gayasha Kavindi Somathilake was involved in formal analysis and Saman B Gunatilake was involved in writing final draft and review.
Ethical Approval
Ethical approval was from the Ethics Review Committee of the Colombo South Teaching Hospital(ERC 873/2020). There were no ethical issues. Informed consent was taken from the participants.
Data Availability
The datasets used during the current study are available from the corresponding author on reasonable request https://figshare.com/s/e6db9a7246f9ef08474a10.6084/m9.figshare.13633949 (Matthias, 2021).
Funding
No funding sources are associated with this paper.
Declaration of Interest
The authors declare that they have no competing interests.
References
Blank, L., Kimball, H., McDonald, W., & Merino, J. (2003). Medical professionalism in the new millennium: A physician charter 15 months later. Annals of Internal Medicine, 138(10), 839–841. https://doi.org/10.7326/0003-4819-138-10-200305200-00012
Egener, B. E., Mason, D. J., McDonald, W. J., Okun, S., Gaines, M. E., Fleming, D. A., Rosof, B. M., Gullen, D., & Andresen, M. L. (2017). The charter on professionalism for health care organizations. Academic Medicine, 92(8), 1091–1099. https://doi.org/10.1097/ACM.0000000000001561
Gillen, P., Sharifuddin, S. F., O’Sullivan, M., Gordon, A., & Doherty, E. M. (2018). How good are doctors at introducing themselves? #hellomynameis. Postgraduate Medical Journal, 94(1110), 204–206. https://doi.org/10.1136/postgradmedj-2017-135402
Matthias, T. (2021). Patient preferences of how they wish to be addressed in a medical consultation – Study from Sri Lanka. https://figshare.com/s/e6db9a7246f9ef08474a
Van Der Merwe, J. W., Rugunanan, M., Ras, J., Röscher, E. M., Henderson, B. D., & Joubert, G. (2016). Patient preferences regarding the dress code, conduct and resources used by doctors during consultations in the public healthcare sector in Bloemfontein, free state. South African Family Practice, 58(3), 94–99. https://doi.org/10.1080/20786190.2016.1187865
*Anne Thushara Matthias
Faculty of Medical Sciences,
University of Sri Jayewardenepura
Email: thushara.matthias@sjp.ac.lk
Submitted: 21 January 2021
Accepted: 16 April 2021
Published online: 5 October, TAPS 2021, 6(4), 135-141
https://doi.org/10.29060/TAPS.2021-6-4/SC2484
Caroline Choo Phaik Ong1,2, Candy Suet Cheng Choo1, Nigel Choon Kiat Tan2,3 & Lin Yin Ong1,2
1Department of Paediatric Surgery, KK Women’s and Children’s Hospital, SingHealth, Singapore; 2SingHealth Duke-NUS Academic Medical Centre, Singapore; 3Department of Neurology, National Neuroscience Institute, SingHealth, Singapore
Abstract
Introduction: The COVID-19 pandemic accelerated use of technology like videoconferencing (VC) in healthcare settings to maintain clinical teaching and continuous professional development (CPD) activities. Sociomaterial theory highlights the relationship of humans with sociomaterial forces, including technology. We used sociomaterial framing to review effect on CPD learning outcomes of morbidity and mortality meetings (M&M) when changed from face-to-face (FTF) to VC.
Methods: All surgical department staff were invited to participate in a survey about their experience of VC M&M compared to FTF M&M. Survey questions focused on technological impact of the learning environment and CPD outcomes. Respondents used 5-point Likert scale and free text for qualitative responses. De-identified data was analysed using Chi-squared comparative analysis with p<0.05 significance, and qualitative responses categorised.
Results: Of 42 invited, 30 (71.4%) responded. There was no significant difference in self-reported perception of CPD learning outcomes between FTF and VC M&M. Participants reported that VC offered more convenient meeting access, improved ease of presentation and viewing but reduced engagement. VC technology allowed alternative communication channels that improved understanding and increased junior participation. Participants requested more technological support, better connectivity and guidance on VC etiquette.
Conclusion: VC technology had predictable effects of improved access, learning curve problems and reduced interpersonal connection. Sociomaterial perspective revealed additional unexpected VC behaviours of chat box use that augmented CPD learning. Recognising the sociocultural and emotional impact of technology improves planning and learner support when converting FTF to VC M&M.
Keywords: Teleconferencing, Morbidity and Mortality Meeting, Continuous Professional Development, Sociomaterial Theory
I. INTRODUCTION
The COVID-19 pandemic instigated worldwide social distancing and rapid uptake of technology to replace face to face (FTF) communication. Healthcare professionals at clinical workplaces adopted educational technological tools to maintain teaching for students, trainees and continuous professional development (CPD) activities (Cleland et al., 2020). Likewise, our hospital-based department pivoted from FTF to interactive web-based videoconferencing (VC) (Zoom) to continue patient-care quality audits and CPD learning.
Before the pandemic, there was limited interest in teleconferencing for health professions education apart from remote learning and formal CPD webinars (Chipps et al., 2012). VC for informal CPD like the Morbidity and Mortality meeting (M&M) was mentioned only to boost attendance of faculty based at distant campuses. The M&M is a regular audit practice of surgical departments that constitutes an important type of informal CPD for individual and organisational learning (de Feijter et al., 2013). Many guidelines exist for FTF M&M but there are none for VC M&M.
Sociomaterial theory examines the mutual relationship of humans with sociomaterial forces and the resultant changes i.e., humans acting on and influenced by objects, nature, culture and/or technology. It provides a useful perspective to evaluate the effect of VC CPD learning and practice by highlighting the importance of materiality – in this case, technology – that is overlooked by other human-centric sociocultural educational theories (Fenwick, 2014). Using sociomaterial framing, we aimed to review the impact of changing from FTF to VC M&M in terms of CPD learning outcomes and user experience.
II. METHODS
A. Description of Context
On 7 Feb 2020, Singapore declared Orange Alert (severity level 3 out of 4) on the national Disease Outbreak Response System in response to the COVID-19 pandemic. Nationwide infection control measures required staff social distancing in public hospitals. Our department (Appendix A: department context and demographics) organises weekly Journal club and M&M as regular CPD; these were converted from FTF to VC meetings from 25 March 2020 till present. Singapore has widespread digital literacy and familiarity with computer usage; our hospital has used electronic health records since 2018. These factors facilitated our rapid pivot to VC meetings.
B. Description of Study
With institutional research board ethics waiver (CIRB Ref: 2020/2697), we sent an email inviting all department staff to participate in a survey about their experience of VC M&M compared to FTF M&M. The sampling frame comprised 18 permanent staff and 24 temporary staff on rotation in the department, from 1 April to 30 June 2020.
The primary outcomes of the survey were self-reported perceptions comparing FTF and VC M&M, addressing categories of CPD learning relevant to M&M: knowledge, practice change, attitude, user outcomes and intention to change (Table 1: Q1-Q3). We asked additional questions (Q4-14) about the FTF/ VC learning environments to elicit possible technological effects on primary outcomes. Face validity of the questionnaire was assessed by authors CCPOng, NCKTan and LYOng who are physicians familiar with M&M.
Recruitment, data collection, data entry and de-identification was performed by author CSChoo (clinical research coordinator) who is outside the department clinical hierarchy. Survey non-responders were given two reminders by CSChoo before the final 3-week deadline. Consent was implied if participants returned the completed survey. Authors CCPOng and CSChoo analysed the de-identified data. Participants responded whether they agreed with the statement, using a 5-point Likert scale. We carried out Chi-squared comparative analysis on 3 grouped categories: (strongly agree+ agree); (neutral) and (disagree+ strongly disagree).
III. RESULTS
A. Descriptive Demographics
We received responses from 30 people out of 42 invited (71.4%) with similar response rates for permanent staff 13/18 (72.2%) and temporary staff 17/24 (70.8%). Appendix A provides details on age, gender, job grade of respondents and prior familiarity with VC.
B. Survey Findings
The participants had attended on average 18.7 (SD 13.4) FTF M&M and 15.1(SD 8.3) VC M&M in the preceding 12 months. Apart from VC M&M, all had attended some other VC event such as administrative meetings, tutorials, webinars and non-work-related workshops or dinners.
|
Q |
Perception |
Analysis* group |
FTF M&M |
VC M&M |
p-value |
|||||||||
|
Strongly disagree & Disagree |
Neutral |
Strongly Agree & Agree |
Strongly disagree & Disagree |
Neutral |
Strongly Agree & Agree |
|||||||||
|
Q1 |
I learnt new medical knowledge |
whole |
0 |
5(16.7) |
25 (83.3) |
1 (3.3) |
0 |
29 (96.7) |
0.043 |
|||||
|
sub |
0 |
1 (4.2) |
23 (95.8) |
1 (4.2) |
0 |
23 (95.8) |
0.368 |
|||||||
|
Q2 |
I learnt new skills (e.g. clinical, teaching, communication, research, team, practical) |
whole |
0 |
7 (23.3) |
23 (76.7) |
1 (3.3) |
5 (16.7) |
24 (80.0) |
0.508 |
|||||
|
sub |
0 |
3 (12.5) |
21 (87.5) |
1 (4.2) |
3 (12.5) |
20 (83.3) |
0.599 |
|||||||
|
Q3 |
I would change my practice based on what I learnt |
whole** |
0 |
7 (24.1) |
22 (75.9) |
1 (3.3) |
3 (10.0) |
26 (86.7) |
0.233 |
|||||
|
sub** |
0 |
3 (13) |
20 (87.0) |
1 (4.2) |
2 (8.3) |
21(87.5) |
0.548 |
|||||||
|
Q4 |
Junior staff are comfortable presenting |
whole |
2 (6.7) |
8 (26.7) |
20 (66.7) |
1 (3.3) |
3 (10.0) |
26 (86.7) |
0.184 |
|||||
|
sub |
2 (8.3) |
3 (12.5) |
19 (79.2) |
1 (4.2) |
2 (8.3) |
21 (87.5) |
0.729 |
|||||||
|
Q5 |
Participants are comfortable to ask questions to clarify |
whole |
4 (13.3) |
9 (30.0) |
17 (56.7) |
3 (10.0) |
7 (23.3) |
20 (66.7) |
0.728 |
|||||
|
sub |
4 (17.7) |
5 (20.8) |
15 (62.5) |
3 (12.5) |
6 (25) |
15 (62.5) |
0.890 |
|||||||
|
Q6 |
Participants are comfortable to raise concerns or disagree with management |
whole |
3 (10.0) |
10 (33.3) |
17 (56.7) |
4 (13.3) |
5(16.7) |
21 (70.0) |
0.328 |
|||||
|
sub |
3 (12.5) |
6 (25.0) |
15 (62.5) |
4 (16.7) |
4 (16.7) |
16 (66.7) |
0.750 |
|||||||
|
Q7 |
Tone of discussion is respectful |
whole |
4 (13.3) |
10 (33.3) |
16 (53.3) |
1 (3.3) |
6 (20.0) |
23 (76.7) |
0.132 |
|||||
|
sub |
3 (12.5) |
6 (25.0) |
15 (62.5) |
1 (4.2) |
5 (20.8) |
18 (75.0) |
0.506 |
|||||||
|
Q8 |
Participants are engaged during the meeting |
whole |
2 (6.7) |
9 (30.0) |
19 (63.3) |
6 (20.0) |
8 (26.7) |
16 (53.3) |
0.314 |
|||||
|
sub |
2 (8.3) |
4 (16.7) |
18 (75.0) |
6 (25.0) |
7 (29.2) |
11(45.8) |
0.105 |
|||||||
|
Q9 |
I can see the slides clearly |
whole |
0 |
9 (30.0) |
21 (70.0) |
2 (6.7) |
1 (3.3) |
27 (90.0) |
0.01 |
|||||
|
sub |
0 |
4 (16.7) |
20 (83.3) |
2 (8.3) |
1 (4.2) |
21 (87.5) |
0.148 |
|||||||
|
Q10 |
I can follow the discussion well |
whole |
0 |
5 (16.7) |
25 (83.3) |
3 (10.0) |
3 (10.0 |
24(80.0) |
0.172 |
|||||
|
sub |
0 |
1 (4.2) |
23 (95.8) |
3 (12.5) |
3 (12.5) |
18 (75.0) |
0.100 |
|||||||
|
Q11 |
It is easy to provide comments during the meeting |
whole |
3 (10.0) |
8 (26.7) |
19 (63.3) |
6 (20.0) |
6 (20.0) |
18 (60.0) |
0.519 |
|||||
|
sub |
3 (12.5) |
3 (12.5) |
18 (75.0) |
6 (25.0) |
6 (25.0) |
12 (50.0) |
0.202 |
|||||||
|
Questions about VC M&M only |
||||||||||||||
|
Q12 |
I find it easy to navigate the buttons/ commands |
Strongly disagree & Disagree |
Neutral |
Strongly Agree & Agree |
||||||||||
|
3 (10%) |
3 (10%) |
24 (80%) |
||||||||||||
|
Q13 |
I prefer to ask questions / comment by |
Typing |
No preference |
Audio |
||||||||||
|
15 (50%) |
12 (40%) |
3 (10%) |
||||||||||||
|
Q14 |
I prefer to have the video on/ off for |
Myself |
Host |
Presenter |
Participant |
|||||||||
|
On |
4 (13.3%) |
12 (40%) |
21 (70%) |
2 (6.7%) |
||||||||||
|
Off |
22 (73.3%) |
3 (10%) |
1 (3.3%) |
8 (26.7%) |
||||||||||
|
No preference |
4 (13.3%) |
15 (50%) |
8 (26.7%) |
20 (66.7%) |
||||||||||
Table 1. Results of the survey
Table 1 shows the collated responses to survey questions comparing experience of FTF and VC M&M (Q1-11) and questions specific to VC technology (Q12-14). There were six participants who either had zero experience of FTF M&M or had experienced FTF M&M only in other departments, not ours. We carried out subgroup analysis excluding these 6 persons to remove possible influence of other M&M styles, since the study focus was on impact of VC technology.
In general, self-reported perceptions of CPD outcomes were similar for both FTF and VC M&M. Participants appreciated that VC allowed us to continue M&M practice during the pandemic while acknowledging both positive and negative technological influences on process. Two questions (Q1 and Q9) had minor differences that were significant on whole group analysis but not significant on subgroup analysis. There was a trend towards decreased engagement for VC M&M compared to FTF M&M (Q8) that was not statistically significant.
When using VC (Table 1: Q12-14; Appendix B qualitative responses), more participants preferred to ask questions or comment by typing in the chat box than speaking on microphone. The most common reason given was to avoid interrupting meeting flow; some highlighted that the chat box facilitated junior staff participation. A few felt that keeping ‘video-on’ for all participants improved engagement but the rest preferred to have own ‘video-off’ with presenter ‘video-on’ to reduce distraction. Participants felt that while technology offered easier meeting access and simplified scheduling, it sometimes reduced engagement and interfered with community-building. Participants preferred more technological support, clearer guidance on expected VC behaviours, better infrastructure and connectivity.
A copy of the informed consent, survey questions and anonymised database are available at https://doi.org/10.6084/m9.figshare.13611611.v1.
IV. DISCUSSION
Sociomaterial perspectives offer new ways to conceptualise health professions education beyond individual cognitive and sociocultural educational lenses (Fenwick, 2014). Underpinned by diverse theories like cultural-historical activity theory, actor-network theory, and complexity theory, it recognises that “objects and humans act upon one another in ways that mutually transform their characteristics and activity” (Fenwick, 2014). Therefore, sociomaterial perspectives illuminate how technology (VC) and related infrastructure (devices and internet connectivity) interact with humans to modify the VC CPD learning environment.
In our context, widespread device penetration and free hospital Wi-Fi access aided rapid adoption of technology. Institution policy mandates internet separation from patient electronic health records, so staff use personal devices instead of hospital computers for meeting access, but it was otherwise straightforward to convert to VC M&M. Nevertheless, some unanticipated issues and VC behaviours manifested.
Introducing new technology is commonly associated with distress with learning how to use it. We chose Zoom as the most user-friendly VC platform because majority had no prior experience with VC. Unfortunately, early issues like ‘Zoom-bombing’ induced the company to make frequent user-interface changes that confused some users. A few participants (both younger and older) felt inadequately supported during their learning curve. We had provided a simple guidance document with link to online Zoom technical support but most preferred trial and error and asking for help during meetings.
Technical support alone is insufficient to address discomfort caused by social aspects of changed processes. We anticipated that uncertainty about protocols or inappropriate participant behaviours could lead to disengagement with poor CPD outcomes. We preempted these risks by following the same CPD framework as FTF M&M (e.g. moderator controls discussion, presentation template, focus on peer review learning without blame) and instituted additional VC safeguards for patient confidentiality by limiting patient identifiers, preventing recording and confirmation of attendee identity for meeting admission. We naturally evolved VC etiquette of queueing using the ‘raise-hand’ button while the moderator invites discussants by name and manages their order.
An ethnographic study of distributed VC in undergraduate medical education found that unintended ‘technologies of exposure’ – visual, curricular and auditory, discomforted the faculty and students (MacLeod et al., 2019). Similarly, many in our study disliked having their ‘video-on’. Although ‘video-on’ could improve interpersonal trust, visual exposure discomfort may interfere with aims of improved engagement and relationship-building. Originally, our department encouraged but did not mandate universal ‘video-on’. Gradually, it became the norm for all to have ‘video-off’ except the host and presenter. Despite ‘video-off’, we can maintain honest conversations necessary for M&M because of trust built through years of training and working together. Prolonged loss of FTF contact may erode trust, hence we created a departmental WhatsApp chat group to enhance social connection.
VC technology afforded unexpected learning contributions. The chat box promotes participation of reticent staff, both senior and junior, especially those preferring written expression; it augments understanding of audio discussion and allows sharing of links to supporting literature. The ease of participation empowers juniors and shifts focus from the vocal few who dominated FTF M&M. While the VC constraint of turn-taking for speakers slows down discussions, it improves interprofessional respect and meeting discipline when host can ‘mute’ the recalcitrant interrupter.
V. CONCLUSION
Sociomaterial perspectives highlight how VC technology changes the CPD learning environment of the M&M. VC provides improved access for participation and alternative communication channels but potentially reduces engagement. Recognising constraints and trade-offs of technology-driven enhancements allows better planning and learner support in VC CPD.
Note on Contributor
Caroline Choo Phaik Ong reviewed the literature, designed the study, analysed de-identified data and wrote the manuscript. Candy Suet Chong Choo performed data collection and de-identification, analysed the data and gave critical feedback to the writing of the manuscript. Nigel Choon Kiat Tan reviewed the literature, advised the design of the study and gave critical feedback to the writing of the manuscript. Lin Yin Ong advised design of the study and gave critical feedback to the writing of the manuscript. All the authors have read and approve the final manuscript.
Ethical Approval
This study received institutional research board ethics waiver (CIRB Ref: 2020/2697).
Acknowledgement
The authors would like to acknowledge the participants of the survey for sharing their responses freely.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of Interest
All the authors have no declarations of conflicts of interest.
Data availability
A copy of the informed consent, survey questions and anonymised database are available at http://doi.org/10.6084/m9.figshare.13611611.v1 under CC0 licence.
References
Chipps, J., Brysiewicz, P., & Mars, M. (2012). A systematic review of the effectiveness of videoconference-based tele-education for medical and nursing education. Worldviews on Evidence-Based Nursing, 9(2), 78-87. https://doi.org/10.1111/j.1741-6787.2012.00241.x
Cleland, J., Tan, E. C. P., Tham, K. Y., & Low-Beer, N. (2020). How COVID-19 opened up questions of sociomateriality in healthcare education. Advances in Health Sciences Education, 25(2), 479-482. https://doi.org/10.1007/s10459-020-09968-9
de Feijter, J. M., de Grave, W. S., Koopmans, R. P., & Scherpbier, A. J. J. A. (2013). Informal learning from error in hospitals: what do we learn, how do we learn and how can informal learning be enhanced? A narrative review. Advances in Health Sciences Education, 18(4), 787-805. https://doi.org/10.1007/s10459-012-9400-1
Fenwick, T. (2014). Sociomateriality in medical practice and learning: Attuning to what matters. Medical Education, 48(1), 44-52. https://doi.org/10.1111/medu.12295
MacLeod, A., Cameron, P., Kits, O., & Tummons, J. (2019). Technologies of exposure: Videoconferenced distributed medical education as a sociomaterial practice. Academic Medicine, 94(3), 412-418. https://doi.org/10.1097/ACM.0000000000002536
*Caroline CP Ong
KK Women’s and Children’s Hospital,
100 Bukit Timah Road,
Singapore 229899
Tel: +65 63941113
Fax: +65 62910161
Email: Caroline.ong.c.p@singhealth.com.sg
Submitted: 27 January 2021
Accepted: 1 April 2021
Published online: 5 October, TAPS 2021, 6(4), 131-134
https://doi.org/10.29060/TAPS.2021-6-4/SC2478
Lean Heong Foo & Marianne Meng Ann Ong
Department of Restorative Dentistry, National Dental Centre Singapore, Singapore
Abstract
Introduction: The novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has caused the COVID-19 pandemic which started in 2020. This resulted in a disruption to educational activities across the globe. Dental education, in particular, was affected because of its vocational nature where learners come into close contact with patients when performing dental procedures.
Methods: This is a narrative review with no research data analysis involved.
Results: Social distancing measures introduced to curb the spread of the infection revolutionised the advancement of online education as the virtual environment is a safer place to conduct teaching compared to face-to-face teaching. In this article, we share our experience at the National Dental Centre Singapore (NDCS) in ensuring the safety of our faculty and learners when conducting didactic and clinical education during the pandemic. Didactic lectures were conducted in the virtual environment via synchronous and non-synchronous teaching. Essential clinical education was conducted in small groups with safe management measures in place. In addition, we provide guidelines to highlight the importance of meticulous planning, thorough preparation, and seamless delivery in conducting effective synchronous teaching.
Conclusion: Safe management measures put in place to ensure the well-being of our faculty and learners can ensure dental education continuity during the pandemic.
Keywords: Dental Education, Education Continuity, COVID-19
I. INTRODUCTION
The COVID-19 pandemic is severely affecting dental professionals since the Department of Labor Occupational and Health Administration United States of America (USA) published guidelines associating aerosol-generating procedures (AGP) in dentistry with SARS-CoV-2 virus spread. Many dental schools in the USA and Asia Pacific have desisted clinical practice and simulation sessions, causing severe disruption in dental training (Chang et al., 2021). Innovative guidelines were developed to conduct dental education during the pandemic (Hong et al., 2021). Singapore has undergone five phases during the pandemic: Pre-pandemic, Circuit Breaker (CB), Phase 1, Phase 2, and Phase 3 (current). We share our experience in continuing dental education for oral healthcare team learners (residents, dental technicians trainees, dental assistant trainees) in NDCS during the pandemic.
II. CLINICAL ADJUSTMENTS
After the Ministry of Health Singapore (MOH) raised the Diseases Outbreak Response System Condition (DORSCON) level from yellow to orange on 7th February 2020 (Pre-pandemic), NDCS senior management immediately adopted team segregation by establishing three self-contained teams comprising clinicians, dental surgery assistants, lab technicians, patient service associate executives, and health attendants (Tay et al., 2020). Learners at NDCS were also assigned to teams. All staff and learners were briefed on safe management measures to observe during clinical sessions. They were required to wear a surgical mask at all times except during meals, perform hand hygiene with an alcohol-based hand sanitiser, and report their temperature twice daily online. Triage and risk assessment of patients were carried out (Hong et al., 2021; Tay et al., 2020) and dental procedures were limited to emergency procedures to relieve pain, ongoing dental treatment, and dental clearance before medical procedures during CB. Use of personal protective equipment (PPE) comprising an eye shield, N95 mask or respirator, surgical gown, and gloves were indicated for all AGP while the use of an eye shield, surgical mask, and surgical gown was indicated for non-AGP following a risk-based assessment (Tay et al., 2020). Patients with suspected COVID-19 or who had close contact with a confirmed case were treated in a negative pressure room with proper PPE. All patients were required to rinse with cetylpyridinium chloride mouth rinse before their procedure. A 15-minute window in between patients was implemented to disinfect the operatory until Phase 3.
III. EDUCATION PROGRAMME ADJUSTMENTS
We conduct three structured education programmes in NDCS–National Institute of Technical Education (NITEC) Dental Assisting (DA), NITEC Dental Technology (DT), and National University of Singapore Master of Dental Surgery Residency Training Programme (RTP) for six dental specialties. In addition, Singapore Institute of Technology (SIT) Diagnostic Radiography (DR) students have observation attachments at NDCS. During CB, Phase 1, and Phase 2, we postponed the new intake of learners for DA due to logistic issues with our collaborators. The posting of DR learners to our centre was also halted. All existing DA and DT learners were allocated to the same clinical team and completed their programme during the pandemic. Residents in the RTP were divided into two groups; one group was based in NDCS and the other in National University Centre for Oral Health Singapore during the 7-week CB. From Phase 1 onwards, the two groups of residents started weekly alternating rotations for their clinical sessions between the two institutions.
NDCS education activities are classified into didactics and clinical sessions. We conducted didactics using synchronous and non-synchronous formats while clinical sessions gradually resumed from Phase 1 to 3 following prevailing MOH and institutional policies. Synchronous teaching and seminars were carried out using Zoom and WebEx online platforms. Voice annotated presentations and e-learning modules were launched in the SingHealth e-learning platform, Wizlearn, for non-synchronous teaching. Clinical sessions were conducted with a small clinical supervisor-learner ratio (1:5), triage of patients, use of complete PPE with an N95 mask, hand hygiene, and high suction evacuator for AGP (Tay et al., 2020). Face-to-face sessions for essential hands-on clinical skills building were organised in Phase 2 and 3 with safe management measures in place such as small instructor-learner ratio, safe distances between learners and instructors, segregation of learners and instructors in groups, donning of surgical masks, meticulous hand hygiene, and proper disinfection after equipment use (Tay et al., 2020).
IV. GUIDELINES FOR ONLINE SYNCHRONOUS TEACHING
Mayer’s theory of multimedia learning (Mayer, 2002) describes the learning process in online education by highlighting the dual channels (auditory and visual) and three stages of memory (sensory, working, and long-term) for processing information. The learner’s eyes and ears capture diagrams and text in the multimedia presentation with sensory memory input. These are converted into a pictorial and verbal mode respectively in the working memory and integrated with prior knowledge from the long-term memory. Educators should prevent cognitive overload in content planning, as learners have limited capacity to hold the pictorial and verbal mode in working memory. A three-phase guide highlighting salient information for conducting effective online synchronous teaching is provided.
A. Meticulous Planning
To understand learners, faculty can adopt a 5W and 1 H concept [(who (the learners), where (location of teaching), why (learning objectives), what (lesson content), when (duration), and how (online platform in this context)] when planning a teaching module. Besides, faculty can construct the learning objectives and teaching activities using Bloom’s taxonomy based on learning outcomes. Bloom’s taxonomy covers six cognitive domains in the following order: knowledge, comprehension, application, analysis, synthesis, and evaluation, where a higher-order is more complicated for the learners to master and demonstrate.
B. Thorough Preparation
Apart from teaching material, a faculty guide is recommended. It should contain the schedule and details of the teaching session, teaching activities, and probing questions and answers for reference; to ensure all the teaching tasks are completed within the planned schedule. Handouts are used to reduce cognitive overload and as a backup when the connection is down. Generally, a good camera, laptop or smartphone, internet connection, a simple background with light, and a quiet room are sufficient for online teaching.
C. Seamless Delivery
Good online synchronous teaching platforms include Zoom, WebEx, Microsoft Teams, Google Meet, Mikogo, and Slack with breakout rooms and annotation board features that are included in the premium subscription of these platforms. A dry run is recommended to familiarise oneself with the functions on the various platforms. Setting the learning climate during the session by preparing learners to respond at appropriate times is crucial. The faculty should look at the camera frequently to keep eye contact with learners. Backup plans that include standby internet access and soft copy handouts are useful when connection is down. Increased feedback and communication between faculty and learners is crucial in online teaching and can be achieved by:
i) Using a learning management system such as GoSoapBox to allow learners to input text individually, particularly useful for clinical case discussion.
ii) Using Slido or Poll Everywhere to conduct needs analysis or summative or formative assessment between teaching.
iii) Utilising the question and answer segment to assess learners’ responses and check progress.
iv) Using the chatbox to allow learners to post questions and comments.
Teleconferencing has limited non-verbal cues coupled with milliseconds delay in observation by other participants that can subconsciously force our brain to restore the synchrony present in face-to-face contact. This overworking can lead to tiredness and discomfort from virtual teleconferencing tools, termed as ‘Zoom fatigue’. Recommendations to reduce Zoom fatigue include taking a rest in between brief lessons and turning off the camera when muted to reduce stimulus and mental fatigue. Netiquette, a blend of ‘internet etiquette’, refers to a code of good behaviour for both educators and learners (Table 1) that should be practised in an online environment (Lateef, 2020) to promote courteous communication between learners and educators for a pleasant learning experience. Evaluation of online education can be conducted during the session by performing formative and summative assessment; assessing quality and completion rate of learners’ assignment; analysing learners feedback from the post-session questionnaire as well as learners’ grade during module assessment and performance in the clinic.
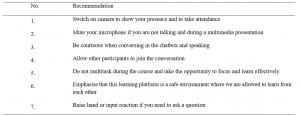
Table 1. Netiquette for online education
Note: Adapted from “Computer-based simulation and online teaching netiquette in the time of COVID 19,” by F. Lateef, 2020, EC Emergency Medicine and Critical Care, 4(8), 84-91.
V. MOVING FORWARD
It may take years to return to pre-COVID-19 normalcy, where physical interaction and large gatherings were social norms. Moving forward, we can consider a hybrid or blended learning module alongside limited face-to-face sessions confined to essential skill-based training. However, the effectiveness of online learning compared to traditional modes of clinical teaching has not been elucidated. Dentistry is a practical vocation that requires developing surgical and psychomotor skills to perform specific tasks. Online learning addresses the delivery of didactics but translating theory into practice which involves hands-on skills, teamwork and communication are challenging in the virtual setting. Virtual and augmented reality programmes such as Spatial, coupled with simulation video demonstration, may be suitable for skill-based training in dental education in the virtual environment. Psychological support for faculty and learners and forming a digital technology community of practice among educators can help to improve resilience and coping mechanisms during this challenging period. With safe management measures in place to ensure the well-being of our faculty and learners, we can adapt and continue education activities while looking for innovative ways to deliver clinical teaching effectively in dentistry amidst this pandemic.
Notes on Contributors
Dr Lean Heong Foo is a Consultant Periodontist in the Department of Restorative Dentistry and Head to the Dental Surgery Assistant Certification Programme. FLH reviewed the literature, contributed to the conception, data acquisition, drafted and critically revised the manuscript.
Dr Marianne Meng Ann Ong is a Senior Consultant Periodontist & Director of Education in National Dental Centre Singapore. MO contributed to the conception, data acquisition and critically revised the manuscript. All authors gave their final approval and agree to be accountable for all aspects of the work.
Ethical Approval
This is a narrative review related to dental education continuity during the COVID-19 pandemic and no ethical approval is required.
Data availability
This paper is a narrative review with no data analysis.
Acknowledgement
The authors would like to thank Ms Safiyya Mohamed Ali for providing editorial support.
Funding
There is no funding involved in the preparation of the manuscript.
Declaration of Interest
The authors declare no conflict of interest.
References
Chang, T., Hong, G., Paganelli, C., Phantumvanit, P., Chang, W., Shieh, Y., & Hsu, M. (2021). Innovation of dental education during COVID-19 pandemic. Journal of Dental Sciences, 16(1), 15-20. https://doi.org/10.1016/j.jds.2020.07.011
Hong, G., Chang, T., Terry, A., Chuenjitwongsa, S., Park, Y., Tsoi, J. K., Kusdhany, M. F. L. S., Egusa, H., Yamada, S., Kwon, J., Seow, L., Garcia, M. C. A. G., Wong, M. L., Ayuchai, P., & Hsu, M. (2021). Guidelines for innovation in dental education during the coronavirus disease 2019 pandemic. Journal of Oral Science, 63(1), 107-110. https://doi.org/10.2334/josnusd.20-0399
Lateef, F. (2020). Computer-based simulation and online teaching netiquette in the time of COVID 19. EC Emergency Medicine and Critical Care, 4(8), 84-91.
Mayer, R. E. (2002). Multimedia learning. Psychology of Learning and Motivation, 41, 85-139.
Tay, J. R. H., Ng, E., Ong, M. M. A., Sim, C., Tan, K., & Seneviratne, C. J. (2020). A risk-based approach to the COVID-19 pandemic: The experience in National Dental Centre Singapore. Frontiers in Medicine, 7. https://doi.org/10.3389/fmed.2020.562728
*Foo Lean Heong
National Dental Centre Singapore
5, Second Hospital Avenue,
168938 Singapore
Email: foo.lean.heong@singhealth.com.sg
Submitted: 31 August 2020
Accepted: 17 February 2021
Published online: 13 July, TAPS 2021, 6(3), 91-94
https://doi.org/10.29060/TAPS.2021-6-3/SC2353
Melissa Su Yi Yong, Xing Tong Yong, Olga Hillary Li Chew & Kuan Chen Zenne T’ng
Speech Therapy Department, Tan Tock Seng Hospital, Singapore
Abstract
Introduction: During the COVID-19 epidemic in Singapore, there was an urgent demand to train more nurses within a short timeframe to perform the Water Swallow Test (WST). The previous training model involved training with actual patients and was time-consuming. Hence, the model was revamped and standardised patients (SPs) were engaged for nurses’ training. This study further investigated nurses’ feedback about the new training model and compared the efficiency and learner-reported outcomes of the previous and new models.
Methods: Nurses who completed WST training from January 2018 to July 2020 were enrolled. Training records were accessed to determine the number of nurses trained under the previous and new models. Nurses were invited to complete post-training evaluation forms and their responses were analysed. Descriptive statistics and the Mann-Whitney U test were used for data analysis.
Results: Under the previous model, 52 nurses were trained over 2 years, whereas under the new model, 112 nurses were trained over two months. From the evaluation form responses, the majority of nurses trained under the new model agreed that they achieved the learning objectives and were confident in performing the WST. There was also no significant difference (p>0.05) found between learner-reported outcomes for both training models.
Conclusion: Our findings demonstrated that the new model that engaged SPs was more efficient in training more nurses. Nurses were also satisfied with the new training model, which achieved similar learner-reported outcomes as the previous model.
Keywords: Water Swallow Test, Standardised Patients, Train-the-Trainer, Dysphagia Screening
I. INTRODUCTION
The Water Swallow Test (WST) is a screening tool used to determine if a patient i) is at risk of aspiration, ii) requires swallowing assessment by a Speech Therapist (ST), and iii) can commence oral feeding (Suiter & Leder, 2008). In hospitals, doctors and nurses perform the WST on patients. Given the importance and potential medical sequelae of the WST, nurses require training before performing the test with patients.
At our institution, WST training is conducted using principles of train-the-trainer (Pearce et al., 2012) and flipped classroom model (Betihavas et al., 2016) to certify nurses as providers and trainers. A provider can conduct the WST on patients, and a trainer can train new providers and conduct the WST.
Previously, training was targeted at nurses in Stroke and Intensive Care Unit (ICU) wards. Trainers and providers had to complete an online module and quiz. Practical training was then conducted on actual patients either by a ST or certified trainer. Each practical was three hours and conducted with suitable patients.
When COVID-19 cases surged in Singapore, there was a pressing requirement to train more providers in ICU wards and at the National Centre for Infectious Diseases (NCID). However, there were challenges in continuing with the existing training model. Training with actual patients was too lengthy to meet the demand for more providers and could not be conducted during the outbreak to minimise patient contact. Therefore, the WST training model was revamped and standardised patients (SPs) were engaged (Kowitlawakul et al., 2015) to overcome the above challenges.
Under the new model, training was targeted at nurses in ICU, outbreak and general wards. Nurses had to complete an online module and quiz before attending training sessions in performing the WST with SPs. Eight providers were scheduled per session, which lasted three hours. The SPs were either a ST, nurse, or therapy assistant due to restrictions in the hospital’s visiting policy to engage professional SPs during the outbreak. The SP followed a standardised script demonstrating different signs of dysphagia. Figure 1 shows details on the previous and new training models.
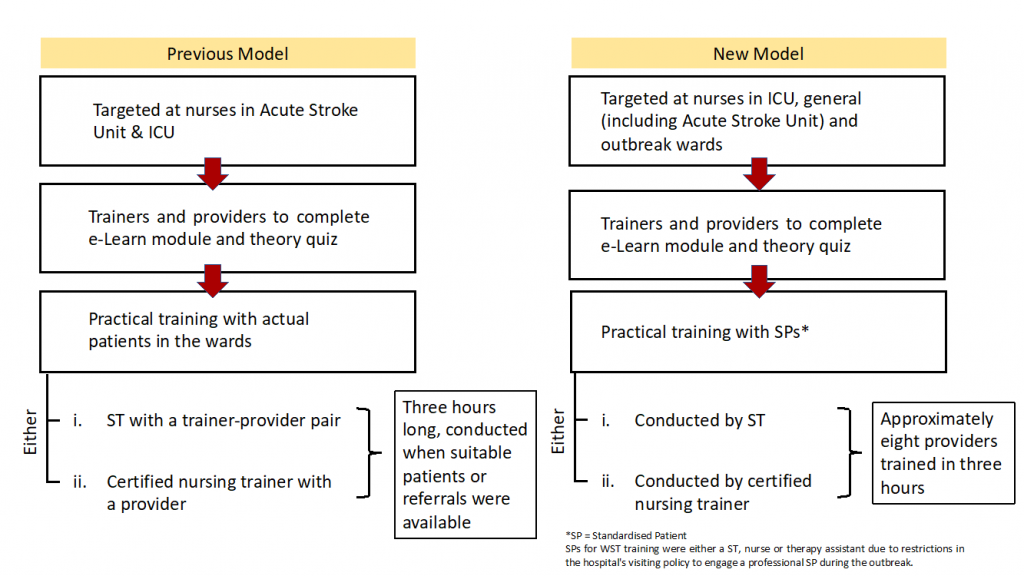
Figure 1: Previous and New Training Models
With the new training model implemented, the following research questions were posed:
1) Is the new training model more efficient in training providers to perform the WST compared to the previous model?
2) Are providers trained under the new model confident that they have achieved the learning objectives of the training and in performing the WST?
3) Is the new training model able to achieve similar learner-reported outcomes for providers as compared to the previous model?
It was hypothesised that:
1) The new training model is more efficient in training providers than the previous model.
2) Majority of providers trained under the new model will feel confident that they achieved the training learning objectives and in performing the WST.
3) The new training model will achieve similar learner-reported outcomes for providers when compared to the previous model.
II. METHODS
Nurses who completed WST training as providers from January 2018 – July 2020 were enrolled. Nurses were trained using the previous training model from January 2018 – April 2020. The new training model was implemented from May 2020.
In order to evaluate the efficiency in training providers under both models, nursing training records were accessed retrospectively to obtain the numbers and dates of providers who completed their training from January 2018 – July 2020. Total training hours under the previous model were computed based on the number of providers who completed training (three hours per provider). Under the new model, total training hours were calculated based on the number of training sessions (three hours per session) conducted from May – July 2020.
In order to evaluate the providers’ confidence in achieving the training’s learning objectives and in performing the WST, providers trained under both models were invited to complete an anonymous course evaluation form generated by the authors and select their responses on a 5-point Likert scale (i.e., strongly agree, agree, neutral, disagree, strongly disagree). The evaluation form was updated along with the new training model, however, these three statements remain unchanged in both versions and were used to analyse learner-reported outcomes:
1. I have a clear understanding of the contraindications of performing the WST.
2. I am confident of accurately identifying all the signs of dysphagia during the WST.
3. I am confident of performing the WST independently.
For data analysis, ‘strongly agree’ and ‘agree’ responses were collapsed into a single category and assigned a score of 1, ‘neutral’ response was assigned a score of 2, and ‘disagree’ and ‘strongly disagree’ responses were collapsed into a single category and assigned a score of 3. Statistical analysis was performed using SPSS statistics version 27.0. Descriptive statistics and the Mann-Whitney U test were used to analyse the evaluation form responses.
Implied consent was obtained from providers who voluntarily completed the form. This study was exempted from a formal NHG Domain Specific Review Board review.
III. RESULTS
A. Number of Providers Trained and Duration Required
Under the previous training model, 52 providers were trained over 24 months (January 2018 – December 2019). The total number of training hours was 156 hours (i.e., 52 providers x three hours). Under the new model, 112 providers were trained in 15 training sessions over two months (end May – mid-July 2020). The total training hours were 45 hours (i.e., 15 sessions x three hours).
Hence, one provider was trained every three-hourly training session and an average of 2.17 providers were trained per month under the previous model. Contrastingly, an average of 7.57 providers were trained every three-hourly training session and an average of 56 providers were trained per month under the new model.
B. Evaluation Form Responses
13 evaluation form responses (Nprevious = 13) were received under the previous model, and 111 responses (Nnew = 111) were received under the new model. The mean scores obtained for the three selected statements were:
1. I have a clear understanding of the contraindications of performing the WST (Previous model: M = 1.08, SD = 0.277; New model: M = 1.22, SD = 0.624).
2. I am confident of accurately identifying all the signs of dysphagia during the WST (Previous model: M = 1.08, SD = 0.277; New model: M = 1.23, SD = 0.567).
3. I am confident of performing the WST independently (Previous model: M = 1.15, SD = 0.555; New model: M = 1.22, SD = 0.563).
C. Comparison of Learner-Reported Outcomes
Scores from the new evaluation form (mean ranks = 62.76, 63.03, 62.90) were higher than scores from the previous form (mean ranks = 60.31, 57.96, 59.08) for all three statements. A Mann-Whitney U test indicated that the differences in scores between the previous and new model for all three statements were not statistically different, UStatement1 (Nnew = 111, Nprevious = 13) = 693.00, z = -0.438, p = 0.661; UStatement2 (Nnew = 111, Nprevious =13) = 662.50, z = -0.786, p = 0.432; UStatement3 (Nnew = 111, Nprevious = 13) = 677.00, z = -0.608, p = 0.543.
The above data set and analysis is available online (Yong et al., 2020).
IV. DISCUSSION
A. Efficiency of New Training Model
The new training model was more efficient than the previous model. Comparing the average number of providers trained per month, the new model was 25 times more efficient. Engagement of SPs allowed more staff to be trained in a single session by seven-fold, versus training with actual patients. Several factors made the new model more efficient: i) greater control over scheduling, ii) saving time from identifying suitable patients for training, and iii) reduced motion waste from accessing actual patients. Hence, more nurses could be trained to meet the needs of outbreak wards.
B. Feedback on Training
The mean rating scores for the three statements in the new evaluation form indicated that providers were satisfied with their training, as they mostly agreed or strongly agreed to achieving the training learning objectives and were confident in performing the WST.
C. Comparison of Learner-reported Outcomes under Both Models
No significant differences were found between responses in the previous and new evaluation forms. Thus, regardless of whether providers trained with actual patients or SPs, most perceived they fulfilled their learning objectives and felt confident to perform the WST independently. These findings indicated that providers did not perceive their training quality to be compromised with the use of SPs and shorter training duration.
D. Limitations
A limitation was that only 25% of providers completed the optional evaluation form under the previous model. The staff who responded likely had a positive training experience and this could lead to potential selection bias. We also acknowledge that the three statements from the evaluation form require further validity and reliability testing to analyse providers’ confidence levels and can be explored in future studies.
V. CONCLUSION
Our study demonstrated that having standardised patients as part of the training method translated to a significant increase in the efficiency of WST training. Potential scale-up of this WST training method can ensure that there is a steady pool of providers and trainers in the workforce to cope during peacetime and crises. Adopting the WST as part of routine dysphagia screening ultimately ensures safer feeding management and early access to Speech Therapy intervention. Further directions include investigating the effectiveness and validity of the new WST training model in various healthcare settings, such as acute and community hospitals and nursing homes, to improve training standards for dysphagia screening in the region, especially in light of the ongoing COVID-19 pandemic.
Notes on Contributors
Yong Su Yi Melissa and Yong Xing Tong evaluated the training model, conducted the training and wrote the manuscript. Olga Hillary Chew Li conducted the training and performed data collection. Zenne T’ng Kuan Chen initiated the design of the training model and gave critical feedback to the writing of the manuscript. All authors read and approved the final manuscript.
Ethical Approval
This study has been reviewed by NHG Domain Specific Review Board (DSRB) for determination of ethics requirement and does not require formal review (NHG DSRB Ref: 2020/00953).
Acknowledgements
We would like to acknowledge:
Senior Nurse Educator Kylie Tang and Nurse Educator Zhao Yue for their feedback in the design of the training model, accessing training records for data collection and collaboration in facilitating WST training for the Nursing Services department.
Senior Speech Therapist Ei Leen Fong for vetting the final manuscript
Principal Speech Therapist Kwong Seh Ling for her guidance in the data analysis and feedback on the manuscript.
Funding
There is no funding involved for this study.
Data Availability
All available data can be accessed publicly via https://doi.org/10.6084/m9.figshare.13110617.
Declaration of Interest
The authors declare there are no conflicts of interest.
References
Betihavas, V., Bridgman, H., Kornhaber, R., & Cross, M. (2016). The evidence for ‘flipping out’: A systematic review of the flipped classroom in nursing education. Nurse Education Today, 38, 15-21. https://doi.org/10.1016/j.nedt.2015.12.010
Kowitlawakul, Y., Chow, Y. L., Salam, Z. H., & Ignacio, J. (2015). Exploring the use of standardized patients for simulation-based learning in preparing advanced practice nurses. Nurse Education Today, 35(7), 894–899. https://doi.org/10.1016/j.nedt.2015.03.004
Pearce, J., Mann, M. K., Jones, C., van Buschbach, S., Olff, M., & Bisson, J. I. (2012). The most effective way of delivering a train-the-trainers program: A systematic review. The Journal of Continuing Education in the Health Professions, 32(3), 215–226. https://doi.org/10.1002/chp.21148
Suiter, D. M., & Leder, S. B. (2008). Clinical utility of the 3-ounce water swallow test. Dysphagia, 23(3), 244–250. https://doi.org/10.1007/s00455-007-9127-y
Yong, M., Yong, X. T., Chew, O., & Tng, Z. K. C. (2020). Training nurses to perform water swallow test with use of standardised patients (raw data & analysis) [Data set]. Figshare. https://doi.org/10.6084/m9.figshare.13435310.v2
*Yong Su Yi Melissa
Tan Tock Seng Hospital,
11 Jalan Tan Tock Seng,
Singapore 308433
Tel: +65 8522 8013
Email: melissa_sy_yong@ttsh.com.sg
Submitted: 31 August 2020
Accepted: 9 December 2020
Published online: 13 July, TAPS 2021, 6(3), 87-90
https://doi.org/10.29060/TAPS.2021-6-3/SC2394
Juanita S. M. Kong1*, Boon See Teo2*, Yueh Jia Lee1, Anu Bharath Pabba1, Edmund J.D. Lee1 & Judy C. G. Sng1
1Department of Pharmacology, Yong Loo Lin School of Medicine, National University of Singapore, Singapore; 2Department of Family Medicine, Yong Loo Lin School of Medicine, National University of Singapore, Singapore
*Equal contribution; first co-authors are in alphabetical order
Abstract
Introduction: With the COVID-19 pandemic, Singapore underwent a national lockdown in which most organisations, including schools were closed. Halting face-to-face tutorials resulting in decreased clinical contact for medical students. Prior to the pandemic, we had developed the Virtual Integrated Patient (VIP). Equipped with conversational technology, it provides students online practice in various clinical skills such as history-taking, physical examination and investigations. The aim of this paper is to describe the supplementary use of VIP in the second-year class, in which a pilot study was conducted.
Methods: The VIP platform was introduced to the cohort and used to supplement the teaching of history-taking in the “Communication with Patients” (CWP) module for second-year students. Traditionally, CWP tutorials involve face-to-face history-taking from standardised patients (SPs). Students, who consented to participating in the trial, had an additional 3 weeks’ access to VIP to practice their history-taking skills. They completed a survey on their user experience and satisfaction at the end of the 3 weeks.
Results: Out of the 106 participants, 87% strongly agreed or agreed that using VIP helped in remembering the content while 69% of them felt that VIP increased their confidence and competence in history-taking.
Conclusion: VIP was well-received by students and showed promise as a tool to supplement history-taking tutorials, prior to students’ encounter with SPs and real patients. Hence, this trend showed its potential as an alternative when clinical rotations were delayed or cancelled. Further research can be done to evaluate its effectiveness in this context.
Keywords: Medical Education Tool, Virtual Patients, Communication, Skill Acquisition, Chatbot, Conversational
I. INTRODUCTION
Clinical skills that are commonly practised face-to-face were a challenge for students to practise during the onset of the Novel Coronavirus (COVID-19) in Singapore. Singapore underwent a 2-month lockdown during which time most non-essential organisations, including medical schools were closed nationwide. In our institution, lectures and tutorials were moved online and face-to-face clinical teaching on campus and in hospitals were cancelled. This move necessitated the use of virtual tools, such as remote meeting through Zoom and the use of virtual patient simulators that do not require the students to be physically on campus.
Virtual patient simulators have been used in a wide range of medical education settings, ranging from the teaching of clinical reasoning, procedural skills, communication skills, and integrated performance to critical thinking (Kononowicz et al., 2019). In recent years, there has been increasing use of virtual patients in the healthcare sector and technology improvements will continue to grow. The Virtual Integrated Patient (VIP) is a virtual patient simulator that was created by our team prior to the pandemic. It leverages on artificial intelligence (AI) technology advancements in the area of naturalistic conversational technology. Prior to VIP, existing technology platforms were focused on the linear, semi-linear and menu-driven (with drop-down option boxes) simulators and there were very few developed in free-text conversations (Kononowicz et al., 2015). The VIP has a natural language processor that is flexible to adapt and adjust to conduct a realistic conversation that can enhance specific skill acquisition (Cendan & Lok, 2012; Kononowicz et al., 2019).
The next unique feature of the VIP is the random patient generator (Figure 1a and b). Every time a student logs in, a new patient is generated. They can revisit the past patients if they have not completed the case and restart where they have left off. The random patient generator provides a realistic situation for users that no two doctors will see the same patient at the same time increasing in variability of patients and potentially, diagnoses. Users can also probe into their virtual patients’ history in their unique ways. Integration of natural language processing using conversational technology has allowed users to chat with the virtual patient as though they are chatting with a real person (Figure 1c). The virtual patient is trained with data sets and is AI-learning enabled. Wi-fi connectivity allows VIP to be accessed anywhere and at any time. It is a safe environment where students are able to make mistakes without any penalty and learn from it. VIP has interfaces for history-taking through a chatbot, physical examination, and laboratory investigations as seen in Figure 1c to d.
The aim of this short communication is to describe how VIP has been employed in a history-taking module for second-year medical students. VIP may play a role in providing a platform for users to consistently practise their skills during a global pandemic where face-to-face tutorials are limited.

Figure 1. a to d. Screenshots of the Virtual Integrated Patient (VIP) interface; b. An example of a random patient generator with no same patient; c. In the history-taking screen, the user can chat with a randomly generated virtual patient, who generates answers using the pre-loaded content and the natural language processor; d. Left: The physical examination screen. d. Right: The laboratory investigations screen which provides realistic case information given explicit buttons throughout interface for easy navigation. Bottom Panel: e to f: Skill Retention Confidence survey results.
II. METHODS
This study’s information sheet, study plan, instruction slides, and survey forms were submitted to the National University of Singapore’s (NUS) institutional review board (IRB) for assessment. It was approved with the study approval code of S-19-263.
VIP was introduced to Phase II “Communications with Patients” (CWP) module in Academic Year (AY) 2019/2020. In this module, students usually clerk a total of three to six standardised patients (SPs) for three sessions over a course of 3 weeks. VIP was introduced to supplement the CWP curriculum. On top of clerking three to six SPs in 3 weeks, participants were given access to VIP during the same 3 weeks. VIP was loaded with cases that complemented and reinforced the contents taught during tutorials, with the aim to deepen students’ understanding of the tutorial content and train them to use the history-taking framework taught during the module.
The VIP team introduced the VIP computer programme and how to use it during the first lecture of the CWP module. Recruitment was done and informed consent was taken from the willing participants for the study. All Phase II students enrolled in the course (n=296) were divided into two groups: the first group received access at the first tutorial (intervention group) and the other group with no access (control group). Eventually, all students from both groups (intervention and control) had received access to the VIP by the end of first week and they could practise over the remaining 2 weeks of the study. Participants were asked to complete a survey at the end of 3 weeks. This is to provide an insight on their confidence levels in executing the history taking exercise and key takeaways with VIP usage at the end of the study.
Students who declined to participate in the study would still have received access to the VIP, but only after the study period of 3 weeks. This ensured fairness for all second-year medical students to have 6 months to practice on the VIP system before their OSCE (Objective Structured Clinical Examination) at the end of the semester.
Following the 3 weeks of tutorials, students were encouraged to continue practising using the VIP prior to the OSCE which was scheduled to be at the end of the academic year. The original study protocol included collection of participants’ history-taking scores at the OSCE, but this was not possible as the OSCE was cancelled due to the COVID-19 situation in Singapore.
III. RESULTS
We obtained quantitative survey responses (n=106 respondents out of 298; 35% response rate). They indicated positively to VIP with 87% of students feeling that using VIP helped in remembering the content. And 69% of the students strongly agreeing or agreed that VIP increased their confidence in taking history (Figure 1f and g).
Students also provided qualitative responses of the key takeaways with the supplementary usage of VIP with their curriculum. First, they indicated that they were able to execute the history-taking procedures more efficiently with additional practice on the VIP. Second, students indicated that they could better remember the methodological content taught in class after repeated usage, thus reinforcing the procedural history-taking skills. Last but not least, survey respondents also reported enhanced understanding of the multiple facets of presenting cases. Where they learnt more about each diagnosis from the summary page after each case completion.
IV. DISCUSSION
VIP was well-received by students in CWP. Users’ survey responses reiterated that more practice aided their skill acquisition, helping them to score in their examinations. By keeping the simulation realistic, they could transfer the skills back into their clinical attachments in future. Also, adding VIP supplementary to the planned curriculum, students were provided additional practice that past years students have requested for in course feedback.
Traditionally, CWP students could only clerk three to six SPs during the whole course of module over a span of 3 weeks. Thereafter, they would not have any chance to practice their history-taking skills through the clerking of SPs until their OSCE which would happen half a year later. Over the years, students provided feedback that they did not receive adequate practice prior to the OSCE and practising on their friends was not feasible due to the hectic nature of their curricular commitments. However, this barrier could not be overcome due to the constraints of the packed timetable of the Phase II students. Therefore, current phase II students who reported that VIP enhances their efficiency and has provided them with adequate practice suggest that VIP is a promising supplement for the course.
One key objective of the VIP is to focus on the processes of getting to a diagnosis rather than just the right diagnosis itself. Medical students’ focus usually stems from the diagnoses to symptom as they are taught in that framework. The enhanced understanding of case definition through the case summaries were welcomed due to the realistic nature of their experiences and how it can be related in the actual clinics. This therefore enhances the students’ enthusiasm toward the usage of the platform. Furthermore, the intention of this was to ease the performance anxiety faced by the students by preparing them in a low-stakes environment, helping them to boost their confidence, in facing SPs or real patients. The study results resonated with this purpose as the students reported greater confidence and efficiency in taking family history after using VIP.
Moreover, the availability of VIP appealed to the students. Due to their curricular commitments, students are more often than not, on the go. While travelling or waiting for a class, where there is available Wi-Fi connectivity, they can log on and practise clerking patients on the simulator. Some students who were not able to attend tutorials were slightly disadvantaged as they would lose one or two SP clerking from the 3 weeks.
V. CONCLUSION
With greater confidence and better utilisation of CWP framework among the students who utilised VIP, VIP is promising as a tool to supplement face-to-face history-taking tutorials. It may have potential use in a pandemic situation where medical students have reduced access to in-person clinical teaching. However, further research is needed to establish its effectiveness as an alternative to in-person clinical teaching.
Notes on Contributors
Author 1, Juanita Kong, was involved in the data collection, analysis, writing, reading, and the final submission of this manuscript. Author 2, Teo Boon See was involved in the planning and execution of this study, writing, reading, and the submission of this manuscript. Both Authors 1 and 2 have equal contribution to the manuscript. Author 3, Lee Yueh Jia, was involved in the data collection, analysis and the reading of this manuscript. Author 4, Anu Bharath Pabba, was involved in the data collection and programming of the tool. Author 5, Edmund Lee was involved in the conceptualisation of the study, data collection, analysis, reading and the final approval of this manuscript. Judy Sng, was involved in the conceptualisation of the study, data collection, analysis, reading and the final approval of this manuscript.
Acknowledgements
We would like to thank the students who participated and provided us with additional feedback when we requested for it. Additionally, we would like to thank all the people who has helped us along the way. Last but not the least, we are grateful for the people who believed in this project.
Funding
The development of the VIP was initially funded by the MOE Tertiary Research Funding (2018 to 2020). It is currently supported by the Yong Loo Lin School of Medicine, under the Innovation Project.
Declaration of Interest
There are no conflicts of interests in this study.
References
Cendan, J., & Lok, B. (2012). The use of virtual patients in medical school curricula. Advances in Physiology Education, 36(1), 48–53. https://doi.org/10.1152/advan.00054.2011
Kononowicz, A. A., Zary, N., Edelbring, S., Corral, J., & Hege, I. (2015). Virtual patients – What are we talking about? A framework to classify the meanings of the term in healthcare education. BMC Medical Education, 15(1), 1–7. https://doi.org/10.1186/s12909-015-0296-3
Kononowicz, A. A., Woodham, L. A., Edelbring, S., Stathakarou, N., Davies, D., Saxena, N., Tudor Car, L., Carlstedt-Duke, J., Car, J., & Zary, N. (2019). Virtual patient simulations in health professions education: Systematic review and meta-analysis by the digital health education collaboration. Journal of Medical Internet Research, 21(7), e14676. https://doi.org/10.2196/14676
*Judy C. G. Sng
Department of Pharmacology,
Yong Loo Lin School of Medicine,
National University of Singapore
MD3, 16 Medical Drive #04-01
Singapore 117600
Tel: +65-65163676
Email: phcsngj@nus.edu.sg
Submitted: 30 August 2020
Accepted: 12 November 2020
Published online: 13 July, TAPS 2021, 6(3), 83-86
https://doi.org/10.29060/TAPS.2021-6-3/SC2390
Rahman Habeebul
Department of Psychiatry, Tan Tock Seng Hospital, Singapore
Abstract
Introduction: Archetypes in psychology are complete models of behaviours, thoughts and feelings, representative of universal experiences. From Plato’s description of Forms to Jung’s analytical introduction to archetypes in psychology, to common use of Moore’s masculine archetypes in popular culture, we use such “complete representations” to enable change.
Methods: In examining psychologically driven responses to the recent and ongoing pandemic crisis, the use of a graphic representation of interacting archetypes is proposed—the ‘archetypogram’.
Results: Drawing on concepts from psychodynamic therapy practise, including Transactional Analysis and Jungian theory, four main archetypes are proposed for their interdependence—the prisoner, the soldier, the sage and the jester/trickster, and a model describing their interactions is presented with the intention of enabling helpful behaviours in response to crisis. The model further proposes positive and negative positions within each archetype, labelled as ‘creating’ and ‘consuming’ behaviours respectively. The ‘archetypogram’ thus is a visual representation of three main components – the four archetypes, creating vs consuming behaviours, and movement between the various positions. Use of the ‘archetypogram’ is aimed at enabling individuals in crisis to move from consuming to creating behaviours.
Conclusion: The ‘archetypogram’ is a model of change which may be applied to persons distressed in crisis, and is able to move behaviours towards positive and creating self-states.
Keywords: Archetypes, Psychology, Crisis, Distress
I. INTRODUCTION
This was a crisis borne on the wings of travellers, leaving in its wake the term ‘a new norm’. In reflecting on observed and experienced emotional responses to the crisis, a structure emerged that identified three main themes—1) feelings of helplessness 2) seemingly never-ending activity and 3) a wish to be able to rise above billowing waves of information and misinformation. Hence the archetypes of a prisoner, a soldier and a sage seemed appropriate.
It was expected that psychological reactions of anxiety, worry, grief and helplessness would run their course in this new crisis, but behavioural responses were unpredictable, from hoarding of toilet roll to disregard of rules and breaking of lockdown laws, to apathy. Why was there a difference between a leader of a nation (Luce, 2020) and a 9-year-old girl (Harris, 2020); one denying the problem at its outset, and the other, deciding to sew personal protective equipment (PPE) gowns to help her local doctors? What enables one person to do what needs to be done in crisis, and yet paralyses another into inaction? Many concepts have been put forth, with names such as grit, resilience, and growth mindset, but are there quick descriptors we can apply, that can help us move out of unhelpful states into more effective, useful ways of being?
II. OBSERVATIONAL PERSPECTIVE
We gravitate towards archetypes—“whole” descriptions of images that we identify with externally, and which we identify within ourselves internally. Jung’s description of archetypes has enabled a scaffold on which we can build our understanding of basic human reactions and behaviours in a Gestalt manner. In archetypes we unite both unconscious and conscious domains of being, and place intention second to observation.
The first evident experiences observed in the thick of the outbreak were feelings of being stuck, or being held hostage by the situation with feelings of helplessness that imprison the person. The prisoner was both angry and sad, and endured a mind filled with comparisons e.g. “Were there other prisoners being better treated? Was the suffering equal? Would someone else gain whilst we were denied of something possibly essential to our well-being, such as PPE?” Locus of control was felt externally (Rotter, 1954).
Amongst those who would put action to thought, a different set of behaviours was noted. There was a sense of constant effort, of having to negotiate endless tasks for a small ‘win’. Life was a blur of activity with anticipation of further problems, and resentment (signalling a slip back into prisoner state), but most times the effort of doing kept away negative emotions. This seemed to be the role of a tireless soldier, who would get wounded through unpreparedness.
There was yet a third group, who seemed untouched by the outbreak. They would go about their usual activities, or turn to alternatives effortlessly. This group I called the sage, and hypothesised that few of us would achieve the transcendental nature they exuded, in keeping with Maslow’s topmost hierarchy of being values (Maslow, 1998).
However, referencing Transactional Analysis (Berne, 1961) where the ego-states of Parent, Adult and Child were further divided into negative and positive functional states depending on how stable they were, a further split within the three archetypes could be seen, with negative positions and positive positions. Hence, for the prisoner archetype, whilst inactivity was observed as a behaviour, the prisoner in a positive position was able to plan, or conserve parts of themselves for further action, to either rise as a soldier or guide as a sage.
The positive position of soldier archetype was decisive, enabling energy to effect change without burning themselves out, and able to make difficult decisions. Behaviour was internally motivated and pragmatically guided by agency.
For the sage archetype, the positive position enabled them to nurture those around, lending stability to the system while being transcendental- as encompassed in the description by Maslow who placed this at the apex of the hierarchy of needs. Such a person is ‘care-ing’, not just caring of those around him or her, but also actively engaged in ‘care’ which is a constant state of being present.
III. INTERVENTIONAL PERSPECTIVE
Pathological emotions, thoughts and behaviours were proposed to arise from a primary prisoner state. Subsequently, as responses to helplessness and anger, three main behaviours were noted. 1) Continued inactivity (staying in the helpless prisoner state). 2) Busyness in ‘doing’, but where excessive activity was used to deflect uncomfortable feelings of helplessness (escape into soldiering) or 3) Non-responsiveness, where the uncomfortable feelings are avoided altogether (escape into sageing). These corresponded to efforts to defeat the source of conflict, but being ineffective, resulted in inaction (self-defeat), ineffective activity (other-defeat) or avoidance (reality-defeat).
Figure 1. The Crisis Archetypogram
If we were to look to the negative positions, we see the behaviours as ‘consuming’, where either time, effort or emotional energy are consumed with poor outcomes, or no change in adapting to crisis.
If we were to look to the positive positions, we see the behaviours as ‘creating’ – ideas are born, work is done to engage parts of the system, there is nurturing of others and effort is concise, allowing adaptation and solving of problems.
In looking at ‘creating’ from the positive position, a further archetype emerges—that of the jester. This was the archetype who was flexible and not imprisoned, not always embattled nor always aloof and calm. This archetype would defuse tense situations with humour as a mature defence mechanism. The utility of the jester lies in the ability to bind people (and oneself) to a common cause; in the absence of hugs, laughter does a fair job of oxytocin production, and of fostering attachment. Pulled into negativity however, the jester’s negative position manifests as a trickster who would undermine with cunning the work done by the planning prisoner, the decisive soldier and the nurturing sage. The trickster at work was observed in the form of self-sabotage, or by disrupting efforts of the group with jokes belittling the efforts of others.
A. Completing the Circle – The ‘Archetypogram’
The ‘Archetypogram’ in Figure 1 seeks to visually represent the interconnectedness of the various archetypes, in positive (creating) and negative (consuming) positions. How may we use such a crisis archetypogram to help ourselves and those around us?
The first step would be to identify where we are in the archetypogram—remembering that the position we are holding is temporary and a state (a current and temporary manner of being or interacting in domains of thoughts, feelings and behaviour), not a trait (longer term more durable repeated patterns of interactions).
The second regular step is to move to creating rather than consuming, and meeting the needs of the future instead of being mired in the past. In times of crisis, resources are limited. By moving to a creating state (which is often creative), we make better use of resources available, or contribute more if we agree to change. In a consuming state, time is a price to pay for opportunity lost when not moving forward, even if no other resources are used (anxiety paralysis).
B. Limitations in Change
Having applied the archetypogram in change management, limitations in effectiveness have been observed in situations where either there was a clinical disorder giving rise to anxiety and depression, or if there was resistance to the idea of change being possible within the archetypogram (similar to being in the pre-contemplative state of change). It is hoped that with development of the archetypogram, limited therapy sessions may be used to address clinical disorders.
IV. CONCLUSION
Whilst it is ideal that we move in the general direction of actualization we need to be mindful of limitations in resources; flexibility in approach is paramount, as is being kind to ourselves no matter the approach we adopt.
In a crisis, the ‘work to do’ therefore is to:
1. Identify the state we are in – Prisoner/ Soldier/ Sage/ Jester-Trickster.
2. Identify the outcome of our behaviours – creating or consuming.
3. Identify how we can move ourselves from a consuming to a creating position, first by moving within our archetype (e.g. from angry/ helpless prisoner, to a conserving/ planning prisoner), then up archetypes (eg on to a decisive soldier, and eventually to a nurturing and care-ing sage). The movement can be internal via self-awareness (a practiced skill incorporating conservation of energy by mindfulness/ relaxation exercises and problem solving) or external via a coach, counsellor or therapist.
4. Be aware of the tendency to move upwards within the consuming rank states where avoidance and burnout from the sage and soldier states respectively can reinforce a primary angry / helpless prisoner’s distressed negative position.
5. Be mindful that the distressed position is often at the base of what one feels and thinks as ‘problems’. Emotional responses of grief, anxiety and anger arise from helplessness or loss, and these responses can be true of individuals as well as groups, but still amenable to working through with the aid of the archetypogram.
In conclusion, while the use of archetypes in verbal tradition is established, the visual archetypogram proposes an exciting model to move behaviours in crisis towards positive and creating self-states, in fields ranging from coaching, to counselling, to psychotherapy.
Note on Contributor
Dr Habeebul Rahman is solely responsible for all observations and ideas contained within this manuscript.
Ethical Approval
Ethics review (including informed consent) was not sought for this manuscript owing to the hypothetico-deductive nature of the paper.
Acknowledgement
The writer wishes to acknowledge TTSH Department of Psychiatry, Organisational Development and Operations for their contribution to the development of this work.
Funding
No funding was sought or obtained for this paper.
Declaration of Interest
No conflicts of interest.
References
Berne, E. (1961). Transactional analysis in psychotherapy: A systematic individual and social psychiatry. Grove Press.
Harris, E. (2020, May 11). For Malaysian schoolgirl, homework is sewing PPE gowns to help beat coronavirus. Reuters https://www.reuters.com/article/us-health-coronavirus-malaysia-protectiv-idUSKBN22N037
Luce, E. (2020, May 17). Inside Trump’s coronavirus meltdown. The Straits Times. https://www.straitstimes.com/world/united-states/inside-trumps-coronavirus-meltdown
Maslow, A. H. (1998). Toward a psychology of being. Wiley.
Rotter, J. B. (1954). Social learning and clinical psychology. Prentice-Hall.
*Rahman Habeebul
Tan Tock Seng Hospital,
11 Jalan Tan Tock Seng,
Singapore 308433
Email: habeebul_rahman@ttsh.com.sg
Submitted: 16 July 2020
Accepted: 16 September 2020
Published online: 13 July, TAPS 2021, 6(3), 95-98
https://doi.org/10.29060/TAPS.2021-6-3/SC2342
Shin Ying Thng, Bao Yu Geraldine Leong, Guat Keng Yvonne Goh, Ching Ching Elaine Tan, Jimmy Kock Keng Goh & Kaibin Kelvin Kuan
Emergency Department, Changi General Hospital, Singapore
Abstract
Introduction: Singapore was one of the earliest countries affected by the COVID-19 outbreak, requiring our emergency department to respond urgently to this surge. A designated Fever Area (FA) with a resuscitation room was rapidly set up to manage patients at risk of COVID-19. Our paper describes measures put into this new area to optimise safety outcomes of these patients.
Methods: Plan-Do-Study-Act (PDSA) cycles incorporating in-situ simulation in the FA resuscitation room were conducted. Using varied resuscitation scenarios and facilitated debriefing, we identified safety gaps and took immediate steps to rectify them in a collaborative manner involving various respective stakeholders.
Results: Following reflective debriefing and studying of work processes, latent safety threats were identified resulting in successful improvements and modifications to protocols, equipment, staffing and processes in the FA resuscitation area.
Conclusion: PDSA cycles involving in-situ simulation helped to identify safety threats and refine work processes in a newly set up FA facility. As a result, our healthcare team was more prepared to manage the complexities of COVID-19 patients in a high-risk environment.
Keywords: Simulation, COVID-19, Medical Education
I. INTRODUCTION
Singapore was one of the first countries to be affected by the COVID-19 pandemic and has the highest number of Covid-19 cases in South East Asia to date. When the COVID-19 outbreak first reached Singapore, healthcare facilities had to prepare for a surge of patients with suspected or confirmed COVID-19. Our Emergency Department (ED) serves a 1006 bed hospital and sees an average of 400 patients daily pre-COVID-19. We were required to quickly reconfigure our space, equipment and staff. There was a need to segregate high risk or suspect COVID cases to be seen in a separate area in order to minimise cross-infection risks to our vulnerable patients. There was also a need to limit exposure of high-risk patients to a designated team of doctors and healthcare professionals in order to ensure continuity of services.
An area comprising the original admission transit area (with three isolation negative pressure rooms) and unused outpatient clinics next to the main ED underwent reconfiguration to become the new designated Fever Area (FA). This was to allow easy access to shared ED resources. The new FA had a combined capacity of 58 patients. Two FA resuscitation rooms were set up to cater for rapidly deteriorating patients that will require endotracheal intubation and resuscitation, both for COVID related complications as well as non-infectious related medical emergencies, such as an acute myocardial infarction or an acute surgical abdomen. Adequate resuscitation and stabilisation facilities in the FA were needed to minimise unnecessary movements of these infectious critically ill patients to the resuscitation area in the main ED, thus, decreasing the risk of cross-infection in other personnel.
The first few patient resuscitations conducted in the FA were challenging. There were many issues raised by the healthcare team concerning resuscitating and performing high-risk procedures in an unfamiliar environment. The FA team recognised an urgent need to improve system workflow competence in the FA resuscitation area. The healthcare team had to be shown that the improved FA resuscitation rooms were as well equipped as the main ED resuscitation area to handle critically ill patients and that such patients can be stabilized effectively there.
II. METHODS
In-situ simulation was the chosen modality as many of the difficulties encountered were systemic issues related to acute care in the unfamiliar FA resuscitation rooms and appropriate usage of Personal Protective Equipment (PPE) in such a scenario. In-situ simulation occurs where the case scenario is simulated in the actual clinical care area with real inter-professional teams instead of in an artificial setting in the simulation centre. By carrying out in-situ simulation, the team hoped to be able to recognise and remedy potential active failures and latent threats (Couto et al., 2018) present in the FA resuscitation rooms before any real-life adverse outcomes (Raemer et al., 2018) can occur.
Four emergency physicians and two nurse clinicians experienced in simulation design and debriefing conducted four in-situ simulation sessions with a high-fidelity mannequin in the FA (Dieckmann et al., 2020). Safety of all faculty, staff and patients were a priority and careful measures were taken to ensure participants and patients were not put at risk by simulating in-situ (Knight et al., 2018). Simulation sessions were conducted at the time of lowest patient load and all participants were outfitted in full PPE. They were also educated prior on potential safety hazards of in-situ simulation. Participant numbers for each simulation session were kept small at five to six with two facilitators.
The simulation scenarios, comprising of COVID-19 patients deteriorating from acute myocardial infarction, respiratory failure and cardiac arrest, were designed to challenge the complexities of adapting clinical management, manpower and equipment requirement and existing workflows to an infectious setting.
A multidisciplinary team comprising of eight nurses, six doctors and two radiographers involved in patient care at the FA participated in four simulation sessions held over two months. Verbal informed consent was taken from participants prior to simulation and confidentiality of participants was ensured. Centralised Institution Review Board (CIRB) review was submitted and waiver of consent was obtained. After each simulation scenario, formalised debriefing was carried out immediately, focusing on work process issues, communication failures and latent threats identified within the FA. Questions were crafted to guide participants to attain dialogical reflection and to move past a description of errors. They were encouraged to consider the implications of observations and come up with solutions for change using Fleck’s framework of reflection levels (Kihlgren et al., 2015).
The list of ideas generated was gathered and studied for common themes. A separate session was held where clinical, operational and administrative representatives brainstormed to find feasible and practical solutions to each problem identified. Immediate steps were taken to implement improvements and modifications to clinical protocols, equipment, staffing and workflows. Plan-Do-Study-Act (PDSA) quality improvement cycles were used to evaluate the improvements instituted after each simulation. This was carried out by a multidisciplinary team, comprising of medical, nursing and allied health staff.
III. RESULTS
The latent safety threats that surfaced were broadly categorised into five descriptive categories: Equipment, Organization, Staffing, Communication and Protocol (Refer to Table 1).
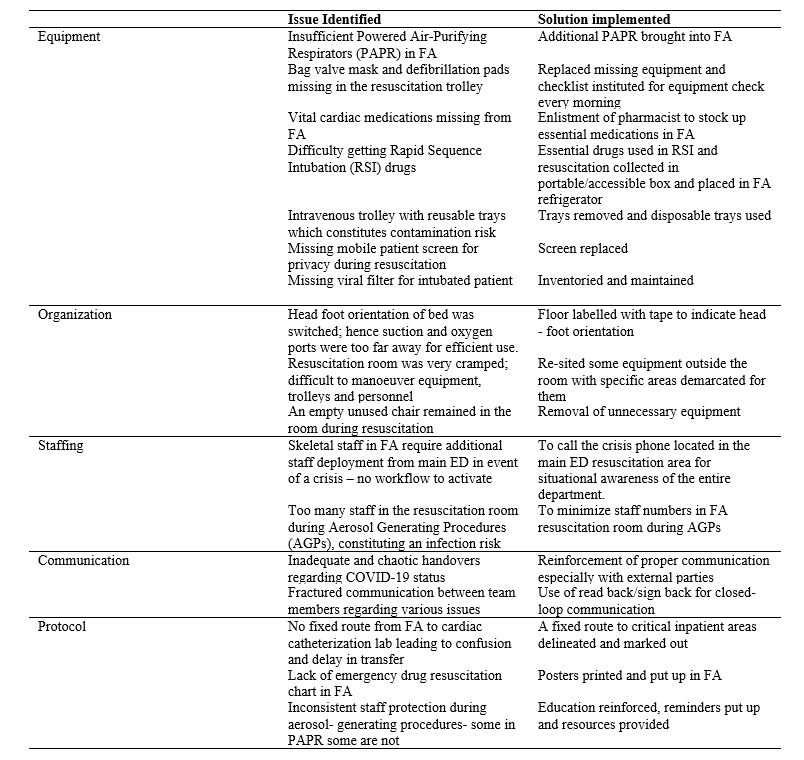
Table 1: Results
In-situ simulation uncovered the problems of insufficient Powered-Air Purifying Respirators (PAPR) and viral filters, as well as, missing defibrillator pads and bag valve masks from resuscitation trolleys. A checklist of essential equipment and medications was created with mandatory checks and re-stocking carried out by the FA nurses every morning. Medications vital for resuscitation were also found to be inadequate. A pharmacist was recruited to draw up and stock an essential list of drugs in the FA. Medications, which required refrigeration, were packed in a portable box so they could be easily brought to the FA resuscitation room from the fridge when required. Drug and resuscitation charts were put up as reminders and easy reference to improve patient safety.
Workspace organization issues that surfaced from in-situ simulation included the need to maintain patient privacy with mobile screens during resuscitation. Confusion over the head-foot orientation of the trolley bed resulted in suction and oxygen ports being too far for efficient use when it was placed in the wrong configuration. To correct this, the FA resuscitation room floor was labelled with tape indicating the proper orientation. The small FA resuscitation room area made manoeuvring equipment, trolleys and personnel difficult. Efforts were taken to re-site equipment to specific demarcated areas outside the FA resuscitation room, with the added benefit of reducing equipment contamination. A crisis phone was set up so that existing staff in FA could quickly call for additional staff deployment in event of a surge, thus improving communication and increasing situational awareness of the entire department to emergent needs at the FA.
Protocols were also adapted to the needs of the FA. During a resuscitation scenario, too many healthcare workers crowded into the room, raising a safety concern. It was protocolised that staff numbers should be minimized in the FA resuscitation room, especially during Aerosol Generating Procedures (AGP). PPE use was a barrier to communications, with “handovers” and “read back” being disrupted or unclear. The importance of adhering to these communication tools was reinforced. There was no fixed route identified for the transport of infectious patients to critical inpatient areas, thus, these were delineated so as to minimize confusion and decrease the infectious footprint, and risk of cross-infection to others. Staff protection during AGP was found to be inconsistent; hence PPE education was reinforced and educational resources provided to staff.
IV. CONCLUSION
Many issues were surfaced and lessons learnt via in-situ simulation, which allowed immediate risk mitigation to be carried out. Simple, immediate changes were made in FA with the available resources, resulting in improved patient and staff safety—which is especially important during surges due to the COVID-19 pandemic. We have successfully used in situ simulation with PDSA cycles to test and develop new facilities and protocols whilst managing the demands of a pandemic. Similar outcomes had also been demonstrated in other in-situ simulation studies. Using this modality to test pre-existing protocols and equipment in the FA resuscitation rooms offered an opportunity for the identification of potential threats and service gaps that would otherwise not have been detected as efficiently via conventional reporting systems (Knight et al., 2018). This method of PDSA testing is useful in the rapidly evolving COVID-19 situation, and may be replicated in other hospitals and regions safely when required. It ensures the safety of healthcare workers and actively improves patient safety despite the limitations of the pandemic.
A follow-up study to look at the usage of the FA resuscitation area, number of critically ill patients in the FA being transferred into the main ED resuscitation room, and patient morbidity and mortality data would be necessary to further determine the success of our intervention at a higher Kirkpatrick level of behavioural change to improve patient outcomes in the FA.
Notes on Contributors
Dr Elaine Tan carried out the literature search and instituted the changes. Dr Geraldine Leong ran the simulation, wrote the manuscript and instituted the changes. Dr Jimmy Goh set up the fever area, advised regarding the manuscript and instituted the changes. Dr Kelvin Kuan ran the simulation, wrote the manuscript and instituted the changes. Dr Thng Shin Ying designed the simulation, ran the simulation, and wrote the manuscript. Dr Yvonne Goh designed the simulation, ran the simulation and wrote the manuscript.
Ethical Approval
This study was exempted from CIRB review- 2020/2640.
Acknowledgements
The authors would like to acknowledge the staff of Changi Simulation Institute for their technical help and assistance with this project. We would also like to thank Dr Syahid Hassan for providing his expertise in the methodology of this project.
Funding
No funding was required.
Declaration of Interest
The authors state no conflict of interest.
References
Couto, T. B., Barreto, J. K. S., Marcon, F. C., Mafra, A. C. C. N., & Accorsi, T. A. D. (2018). Detecting latent safety threats in an interprofessional training that combines in situ simulation with task training in an emergency department. Advances in Simulation, 3(1), 23. https://doi.org/10.1186/s41077-018-0083-4
Dieckmann, P., Torgeirsen, K., Qvindesland, S. A., Thomas, L., Bushell, V., & Langli Ersdal, H. (2020). The use of simulation to prepare and improve responses to infectious disease outbreaks like COVID-19: Practical tips and resources from Norway, Denmark, and the UK. Advances in Simulation, 5, 3. https://doi.org/10.1186/s41077-020-00121-5
Kihlgren, P., Spanager, L., & Dieckmann, P. (2015). Investigating novice doctors’ reflections in debriefings after simulation scenarios. Medical Teacher, 37(5), 437-443. https://doi.org/10.3109/0142159X.2014.956054
Knight, P., MacGloin, H., Lane, M., Lofton, L., Desai, A., Haxby, E., Macrae, D., Korb, C., Mortimer, P., & Burmester, M. (2018). Mitigating latent threats identified through an embedded in situ simulation program and their comparison to patient safety incidents: A retrospective review. Frontiers in Pediatrics, 5, 281. https://doi.org/10.3389/fped.2017.00281
Raemer, D., Hannenberg, A., & Mullen, A. (2018). Simulation safety first: An imperative. Simulation in Healthcare, 13, 373-375. https://doi.org/10.1097/SIH.0000000000000341
*Thng Shin Ying
Changi General Hospital
2 Simei Street 3
Singapore, 529889
Email: thng.shin.ying@singhealth.com.sg
Submitted: 2 April 2020
Accepted: 3 June 2020
Published online: 5 January, TAPS 2021, 6(1), 109-113
https://doi.org/10.29060/TAPS.2021-6-1/SC2243
Wen Hao Chen1, Shairah Radzi1, Li Qi Chiu2, Wai Yee Yeong3, Sreenivasulu Reddy Mogali1
1Lee Kong Chian School of Medicine, Nanyang Technological University, Singapore; 2Department of Emergency Medicine, Tan Tock Seng Hospital, Singapore; 3Singapore Centre for 3D Printing, School of Mechanical and Aerospace Engineering, Nanyang Technological University, Singapore
Abstract
Introduction: Simulation-based training has become a popular tool for chest tube training, but existing training modalities face inherent limitations. Cadaveric and animal models are limited by access and cost, while commercial models are often too costly for widespread use. Hence, medical educators seek a new modality for simulation-based instruction. 3D printing has seen growing applications in medicine, owing to its advantages in recreating anatomical detail using readily available medical images.
Methods: Anonymised computer tomography data of a patient’s thorax was processed using modelling software to create a printable model. Compared to a previous study, 3D printing was applied extensively to this task trainer. A mixture of fused deposition modelling and material jetting technology allowed us to introduce superior haptics while keeping costs low. Given material limitations, the chest wall thickness was reduced to preserve the ease of incision and dissection.
Results: The complete thoracostomy task trainer costs approximately SGD$130 (or USD$97), which is significantly cheaper compared to the average commercial task trainer. It requires approximately 118 hours of print time. The complete task trainer simulates the consistencies of ribs, intercostal muscles and skin.
Conclusion: By utilising multiple 3D printing technologies, this paper aims to outline an improved methodology to produce a 3D printed chest tube simulator. An accurate evaluation can only be carried out after we improve on the anatomical fidelity of this prototype. A 3D printed task trainer has great potential to provide sustainable simulation-based education in the future.
Keywords: Medical Education, Chest Tube, Thoracostomy, Simulation, 3D Printing
I. INTRODUCTION
Training opportunities in procedures such as chest tube insertions are increasingly limited amidst a growing population of trainees. Yet, the deliberate practice remains essential to improving proficiency and preventing possible complications such as lung parenchymal damage (Hernandez, El Khatib, Prokop, Zielinski, & Aho, 2018). Hence, many institutions have adopted simulation-based training to provide realistic training opportunities while mitigating harm to patients.
Cadaveric and animal models are limited by access and cost, and raise religious and ethical concerns (Kovacs, Levitan, & Sandeski, 2018). In addition, commercial models tend to be very costly (e.g. Trauma-Man® at USD~$25,000). As such, new modalities are desired.
Three-dimensional (3D) printing can accurately recreate anatomical details from imaging data through precision modelling and a wide range of compatible printing materials (Mogali et al., 2018). Together with its decreasing cost, it has become an attractive technology for creating inexpensive and anatomically accurate simulation modalities.
A previous study from the Federal University of Parana, Brazil (Bettega et al., 2019) outlined the development and evaluation of a low-cost chest tube simulator. The bony structures were 3D printed, while the remainder of the model was manually assembled using silicone sheets, foam pads, and balloons.
They compared 2 groups of participants using a porcine rib model, and their 3D printed simulator respectively. They found subjective improvements in confidence and safety amongst both groups and showed no difference between the objective grades. Hence, they concluded that their 3D printed simulator was equivalent to the animal model concerning the simulation of a chest tube placement.
However, there exist many other 3D printing technologies and materials, which can potentially be applied to create superior haptics and anatomical detail. Hence, this paper aims to outline a methodology of integrating multiple 3D printing modalities to create a cost-efficient 3D printed chest tube simulator.
II. METHODS
An anonymised computerized tomography (CT) file of a healthy human thorax (2.5 mm slices thickness) in Digital Communication in Medicine (DICOM) format was downloaded from the databank provided by 3D Slicer (https://www.slicer.org/, Version 4.10.2). The CT data was available freely for research and educational use at the time of this study.
3D Slicer was employed to segment the thoracic bony structures using a radiodensity based threshold algorithm, which traces the bone based on the Hounsfield units. Due to a lack of contrast possibly from the poor resolution of the CT images, we were not able to segment the respective soft tissue layers using thresholding. Hence, the intercostal muscles were manually drawn with the paintbrush function. Intrathoracic organs were all removed to create a central cavity. From initial experimentation, we found that incision and dissection were too difficult to perform if the task trainer was printed at the true thoracic thickness. Hence, a decision was made to thin out the chest wall. At the 4th and 5th intercostal space midaxillary line, the mean chest wall thickness is 39mm (Laan et al., 2016), but our model measured at 18mm at this corresponding anatomical landmark.
Further processing was done to smoothen the contours of the model (see Appendix, A). Subsequently, the anatomical structures were saved as stereolithography (STL) file and exported into Materialise Magics (Version 20 by Materialise, Belgium).
On Magics, cut and Boolean techniques were used to create the replaceable component. This space was demarcated by the 5th to 6th intercostal space, between anterior axillary to the mid axillary line. To create a secure fit for the replaceable piece, a groove was created and reinforced using the cut and punch function which generates teething to maximise friction. The main frame measured 23cm (length) x 19.5cm (width) x 23.5cm (height), while the replaceable part measured 9cm (length x 8.1cm (width) x 0.8cm (height). The Fix Wizard and Shrink Wrap Part functions were used to repair the surface mesh and eliminate holes and loose shells. The models were then exported using IdeaMaker® (Raise3D, USA) and uploaded to the printer.
The model was printed in two parts: the main frame was printed using fusion deposition modelling (FDM). This technology extrudes a continuous filament of melted thermoplastic, repeated by layer based on the design coordinates. Bones were printed with polylactic acid (PLA) which is a rigid material while the intercostal muscles were printed with thermoplastic urethane (TPU) which is a flexible material. Support was printed using PLA. We utilised a dual nozzle extrusion printer (Raise3D Pro 2, Raise3D, USA) to allow us to print the bony and soft tissue simultaneously, thereby increasing convenience. The following settings were used: printing speeds were reduced to 25mm/s, retraction of the TPU extrusion head was disabled, nozzle temperatures were set at 200°C, and build plate temperature was at 65°C. Post-print processing was done to remove the support, with subsequent filing and sanding.
The replaceable part was printed using Objet500 Connex 3 (Stratasys Ltd, Eden Prairie, MN), a multi-material printer utilising material jetting technology. This technology drops liquid photopolymers onto the build tray and simultaneously cures the material using UV light. As such, we can mix plastic and rubber to create hybrid consistencies (Mogali et al., 2018) of varying shore hardness. Two materials were selected to achieve the desired haptics: VeroWhite (FullCure, RGD835) was the stiff plastic photopolymer used for bones, while Tango Plus (FullCure, 930) was the rubber photopolymer used for simulating soft tissue. Support resin (FullCure, 706) was also used for printing. Post-printing processing was required to remove the support resin.
Skin coloured silicone sheets of 5 mm thickness were wrapped around the model using generic superglue. The task trainer was cable tied to stainless steel supports and screwed onto a laminated wood baseplate. Cut sponges were wrapped in duct tape to simulate the lung parenchyma and placed into the central cavity created.
III. RESULTS
The completed task trainer is shown in Figure 1. Both the main frame and replaceable piece provided simulation for the ribs, intercostal muscles, and skin.
The 3D thoracostomy task trainer costs approximately SGD$130 (or USD$97) (excluding manpower and printer cost)–see Appendix, B). The baseplate and mount were repurposed and did not add to costs.
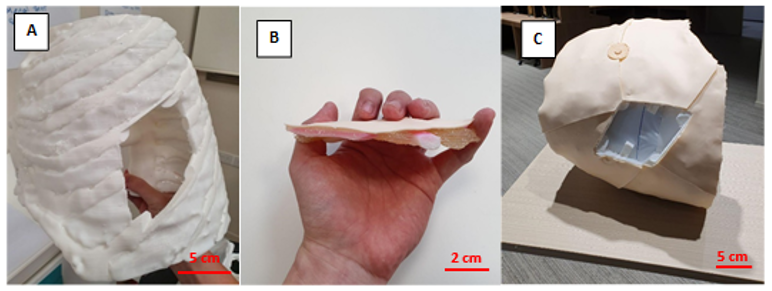
Note. A = completed hemithorax main frame using FDM printing; B= replaceable piece; C = task trainer without the replaceable piece. Figure 1. Photos of the completed task trainer
The main frame required 676g of polylactic acid and 114g of thermoplastic urethane. The replaceable piece required 30g of VeroWhite, 22g of Tango Plus, and 66g of Support706. It took a total of approximately 118 hours to print the entire task trainer.
IV. DISCUSSION
Our methodology addressed several issues with the model as outlined by the Brazilian team (Bettega et al., 2019). The proposed methodology here required less manual assembly of components, thereby saving time and improving fabrication. By utilising dual extrusion printing, construction was simplified while integrating an additional material for varying consistencies. The creation of a replaceable piece also meant long term savings in the cost of utilising this model. These logistical advantages would make it easier to adopt our proposed task trainer.
Secondly, simple materials such as foam pads and silicone sheets were inferior in simulating human tissue. Our utilisation of material jetting technology with the Objet500 Connex 3 (Stratasys Ltd, Eden Prairie, MN) printer allowed us to blend plastic and rubber materials to better recreate the consistency of human tissue. This technology and blend of materials have been extensively validated in other simulation models (Mogali et al., 2018).
Cost remains an important impedance to the widespread use of simulation in procedural education. We performed a surface comparison of our product against an existing commercial model in use by a local hospital in Singapore (LF03770U by Lifeform, NASCO, USA). The task trainer outlined here (~USD$97) is significantly cheaper than the commercial trainer (~USD$1,800). Also, our material blend provides superior haptics and bony structures in the replaceable component, as compared to a plain silicone insert in the Lifeform model. These should provide improvements in the quality and quantity of simulation opportunities for training physicians.
Unfortunately, we were not able to recreate the anatomical thickness of the thorax given our material limitations at the time of writing. This inaccurate depth of dissection creates a confounding variable when evaluating our task trainer against existing cadaveric or commercial simulators. Hence, an evaluation of this task trainer was withheld to address this limitation in our future prototype. Moving forward, we plan to invite physicians to validate the efficacy of our improved task trainer.
V. CONCLUSION
We have outlined the methodology for creating a 3D printed tube thoracostomy task trainer using a combination of printing technologies. The outlined task trainer could potentially provide superior haptics at a lower cost while improving fabrication. However, an equitable validation against an existing modality of simulation can only be done after we achieve a comparable anatomical fidelity.
In our continued search for sustainable simulation models, 3D printing shows great potential in reproducing anatomical detail with superior cost efficiency. The growing availability of 3D printing infrastructure makes the large-scale adoption of such task trainers ever more realistic. It makes it therefore worthwhile to invest in the creation of the perfect 3D printed task trainer.
Notes on Contributors
Mr. Wen Hao Chen is an undergraduate medical student with the Lee Kong Chian School of Medicine, Singapore. He was involved in the development of the task trainer, along with co-authoring the submitted manuscript.
Dr. Shairah Radzi is a research fellow with the Lee Kong Chian School of Medicine, Singapore. She was involved in the development of the task trainer, along with co-authoring the submitted manuscript.
Dr. Li Qi Chiu is a consultant physician in the Department of Emergency Medicine in Tan Tock Seng Hospital, Singapore. She was involved in the development of the task trainer, along with co-authoring the submitted manuscript.
Assoc. Prof Wai Yee Yeong is the Associate Chair (Students) of the School of Mechanical and Aerospace Engineering, Nanyang Technological University, Singapore. She was involved in the development of the task trainer, providing her technical expertise on the 3D printing process, along with co-authoring the submitted manuscript.
Asst. Prof Sreenivasulu Reddy Mogali is the Head of Anatomy and Principal Investigator in Clinical Anatomy and Medical Education at Lee Kong Chian School of Medicine, Singapore. He was involved in the development of the task trainer, along with co-authoring the submitted manuscript. He serves as the principal investigator.
Ethical Approval
Approved by Nanyang Technological University’s Institutional Review Board (2019-07-017). The CT scans used were anonymised and provided free for education and research use by 3D Slicer (https://www.slicer.org/, Version 4.10.2).
Acknowledgement
The authors thank the staff and faculty of the Lee Kong Chian School of Medicine, Nanyang Technological University, Singapore for supporting this research; Singapore Centre for 3D Printing, Nanyang Technological University for their technical support.
Funding
This project was funded by the Ministry of Education Research Start-Up Grant, Lee Kong Chian School of Medicine, Nanyang Technological University Singapore.
Declaration of Interest
All authors declare no conflict of interest. The authors alone are responsible for the content and writing of the article.
References
Bettega, A. L., Brunello, L. F. S., Nazar, G. A., De-Luca, G. Y. E., Sarquis, L. M., Wiederkehr, H. de A., … Pimentel, S. K. (2019). Chest tube simulator: Development of low-cost model for training of physicians and medical students. Revista Do Colégio Brasileiro de Cirurgiões, 46(1). https://doi.org/10.1590/0100-6991e-20192011
Hernandez, M. C., El Khatib, M., Prokop, L., Zielinski, M. D., & Aho, J. M. (2018). Complications in Tube Thoracostomy: Systematic review and Meta-analysis. The Journal of Trauma and Acute Care Surgery, 85(2), 410–416. https://doi.org/10.1097/TA.0000000000001840
Kovacs, G., Levitan, R., & Sandeski, R. (2018). Clinical Cadavers as a Simulation Resource for Procedural Learning. AEM Education and Training, 2(3), 239–247. https://doi.org/10.1002/aet2.10103
Laan, D. V., Vu, T. D. N., Thiels, C. A., Pandian, T. K., Schiller, H. J., Murad, M. H., & Aho, J. M. (2016). Chest Wall Thickness and Decompression Failure: A Systematic Review and Meta-analysis Comparing Anatomic Locations in Needle Thoracostomy. Injury, 47(4), 797–804. https://doi.org/10.1016/j.injury.2015.11.045
Mogali, S. R., Yeong, W. Y., Tan, H. K. J., Tan, G. J. S., Abrahams, P. H., Zary, N., … Ferenczi, M. A. (2018). Evaluation by medical students of the educational value of multi-material and multi-colored three-dimensional printed models of the upper limb for anatomical education. Anatomical Sciences Education, 11(1), 54–64. https://doi.org/10.1002/ase.1703
*Sreenivasulu Reddy Mogali
11 Mandalay Road, Singapore 308232
Lee Kong Chian School of Medicine,
Nanyang Technological University
Email: sreenivasulu.reddy@ntu.edu.sg
Announcements
- Best Reviewer Awards 2024
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2024.
Refer here for the list of recipients. - Most Accessed Article 2024
The Most Accessed Article of 2024 goes to Persons with Disabilities (PWD) as patient educators: Effects on medical student attitudes.
Congratulations, Dr Vivien Lee and co-authors! - Best Article Award 2024
The Best Article Award of 2024 goes to Achieving Competency for Year 1 Doctors in Singapore: Comparing Night Float or Traditional Call.
Congratulations, Dr Tan Mae Yue and co-authors! - Fourth Thematic Issue: Call for Submissions
The Asia Pacific Scholar is now calling for submissions for its Fourth Thematic Publication on “Developing a Holistic Healthcare Practitioner for a Sustainable Future”!
The Guest Editors for this Thematic Issue are A/Prof Marcus Henning and Adj A/Prof Mabel Yap. For more information on paper submissions, check out here! - Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Volume 9 Number 1 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors. - Volume 8 Number 3 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2021
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2021.
Refer here for the list of recipients. - Most Accessed Article 2021
The Most Accessed Article of 2021 goes to Professional identity formation-oriented mentoring technique as a method to improve self-regulated learning: A mixed-method study.
Congratulations, Assoc/Prof Matsuyama and co-authors. - Best Reviewer Awards 2020
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2020.
Refer here for the list of recipients. - Most Accessed Article 2020
The Most Accessed Article of 2020 goes to Inter-related issues that impact motivation in biomedical sciences graduate education. Congratulations, Dr Chen Zhi Xiong and co-authors.









